College of Health
35 Cognitive Impact of Subjective and Objective Sleepiness
Joshua Chang and Christopher Depner (Health, Nutrition, and Kinesiology)
Faculty Mentor: Christopher Depner (Health, Kinesiology, and Recreation, University of Utah)
Introduction
1Partial sleep deprivation has been shown to evoke significant cognitive and neurobehavioral deficits amongst adults and adolescents. 2Despite significant research on the correlation between sleep, mood, and cognition, there is a promising avenue for further analysis on understanding potential links between these variables and the established trait-like interindividual susceptibilities among people with habitual short sleep duration in the real world. 3Findings from a study in postpartum women showed inaccurately interpreting physiological sleep duration could spawn negative emotions and thus worsen cognitive ability throughout the day. Alternatively, such inaccurate interpretations of sleep could also cause the individual to believe they slept well, leading them to overestimate their cognitive abilities after a night of poor sleep. Such circumstances could have deadly public health and safety consequences for individuals in safety critical fields like the medical, military, and transportation industries. The aim of this study is to investigate the links between subjective and objective sleepiness, cognitive performance, and inter-individual vulnerabilities to insufficient sleep.
Methods
12 healthy adults (6M/6F), aged 24±5y (mean±SD), completed a 47-day protocol that consisted of two 4-day laboratory visits separated by 10 days. Prior to each of the two 4-day laboratory visits participants maintained two weeks of ~9 hours/night sleep opportunities. Participants were provided controlled energy balanced diets for two days before and throughout each laboratory visit. Sleep opportunities for each laboratory visit consisted of 9 hours on night 1 (baseline), 5h on nights 2 and 3 (insufficient sleep), and recovery sleep on night 4. We assessed objective sleepiness with the Multiple Sleep Latency Test (MSLT) and subjective sleepiness with the Karolinska Sleepiness Scale (KSS). These tests were administered 5 times every 2h during scheduled wakefulness over the final 24 hours of baseline and during sleep restriction in each of the laboratory visits. Ability to sustain attention was assessed every 2h during scheduled wakefulness with the Psychomotor Vigilance Test (PVT) during each of the laboratory visits.
Protocol
Figure 1.
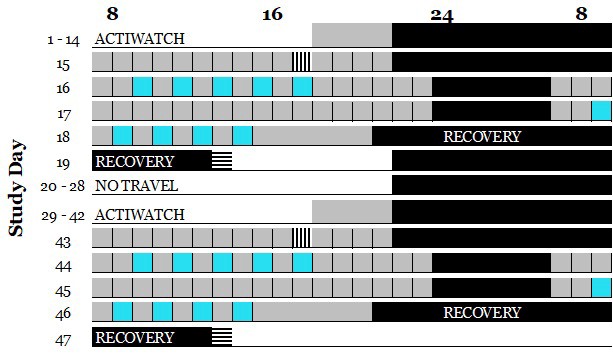
Days 1-14 & 29-42 baseline ambulatory home monitoring with scheduled 9-hour nightly sleep opportunities. Days 15 & 43 laboratory baseline assessments with 9-hour nightly sleep opportunities and energy balanced food intake. Days 16-17 & 44-45 laboratory insufficient sleep assessments with 5-hour nightly sleep opportunities. Sleep was restricted to 5 hours for time in bed by delaying bedtime and advancing waketime by 2 hours each. Vertical bars represent the start of each laboratory visit and horizontal bars represent the end of each laboratory visit. Blue boxes represent MSLT and KSS tests administered in parallel with each other
Results
Figure 2. Increase in objective sleepiness over the course of the study.
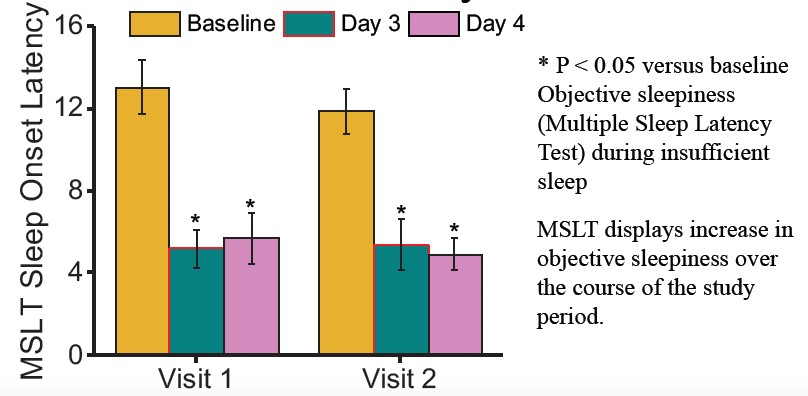
Figure 3.
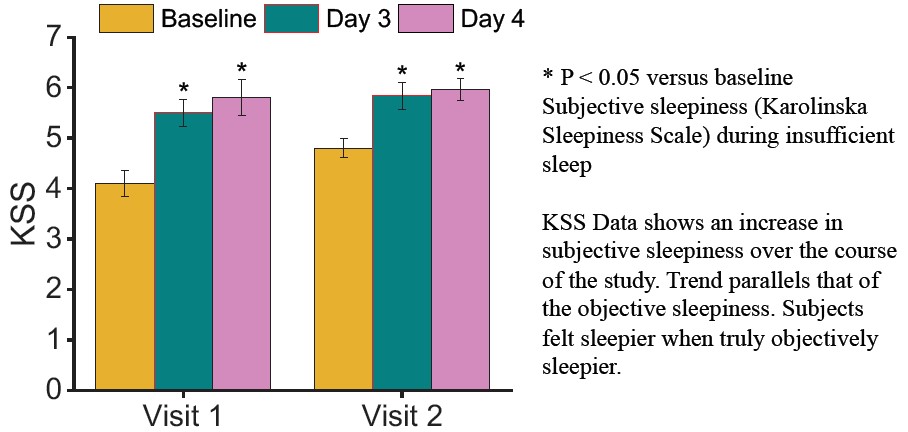
Figure 4.
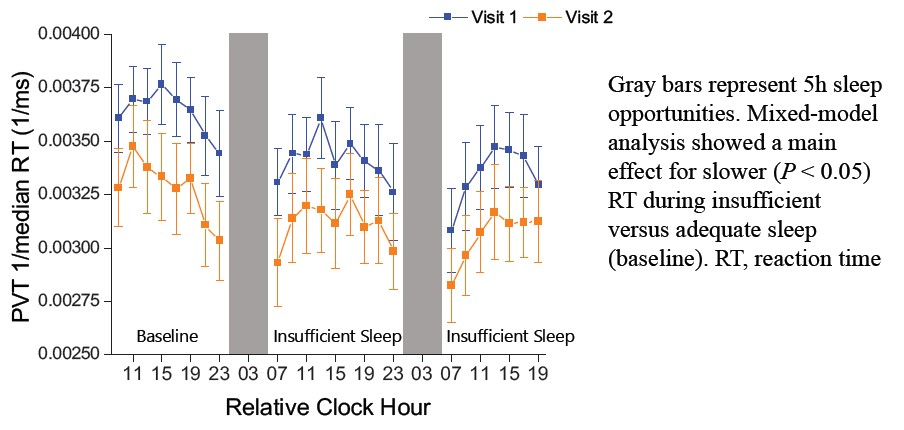
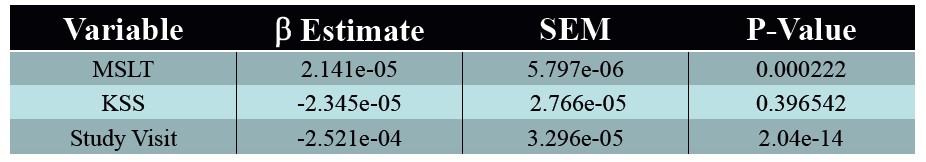
Figure 5. Full linear mixed model regression with MSLT, KSS, and study visit with sustained attention (PVT). Analysis shows objective duration is most strongly correlated with PVT performance.
Conclusion
As the study day progressed and subjects experienced insufficient sleep, they reported an increasing sense of sleepiness. Objective measures of sleepiness revealed a consistent decline in median PVT reaction time during periods of insufficient sleep in comparison to baseline adequate sleep, and subjects fell asleep faster during these periods. Full mixed model analyses demonstrated that the strongest correlation existed between objective sleepiness and PVT reaction time. These results indicate that subjective sleepiness is an unreliable predictor of sustained attention, which is a crucial factor for public safety. Therefore, these findings underscore the critical need for remedial action in essential fields such as medicine, military, and transportation, where sleep is often limited.
References
- Goel, N., Rao, H., Durmer, J. S., & Dinges, D. F. (2009). Neurocognitive consequences of sleep deprivation. Seminars in neurology, 29(4), 320–339. https://doi.org/10.1055/s-0029-1237117
- Banks, S., & Dinges, D. F. (2007). Behavioral and physiological consequences of sleep restriction. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine,
- (5), 519–528. 3Insana, S. P., Stacom, E. E., & Montgomery-Downs, H. E. (2011). Actual and perceived sleep: associations with daytime functioning among postpartum women. Physiology & behavior, 102(2), 234–238. https://doi.org/10.1016/j.physbeh.2010.11.017

