College of Health
33 Hip Mechanics as a Reflection of Physical Function in Aging Adults with Early to Late-Stage Hip Osteoarthritis
Hunter Blake Carlson and Jesse C. Christensen (Physical Therapy & Athletic Training)
Faculty Mentor: Jesse C. Christensen (Physical Therapy & Athletic Training, University of Utah)
Abstract
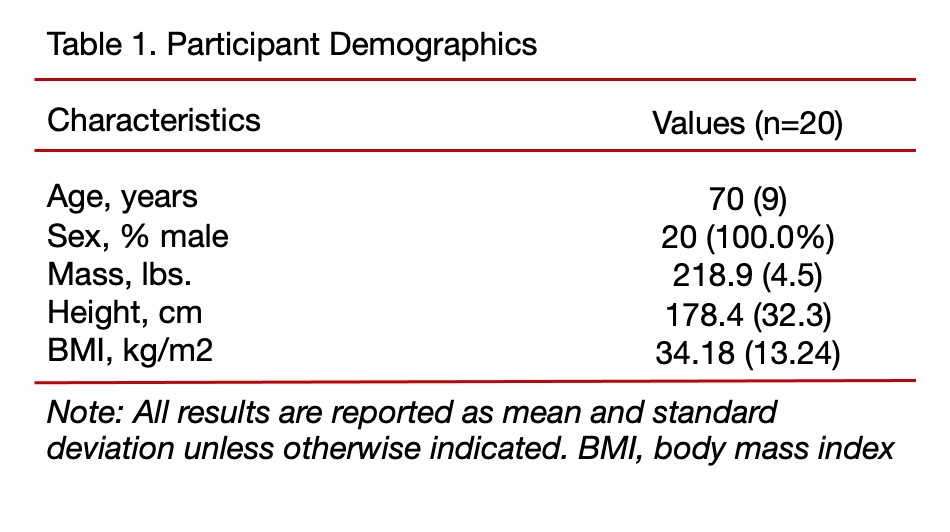
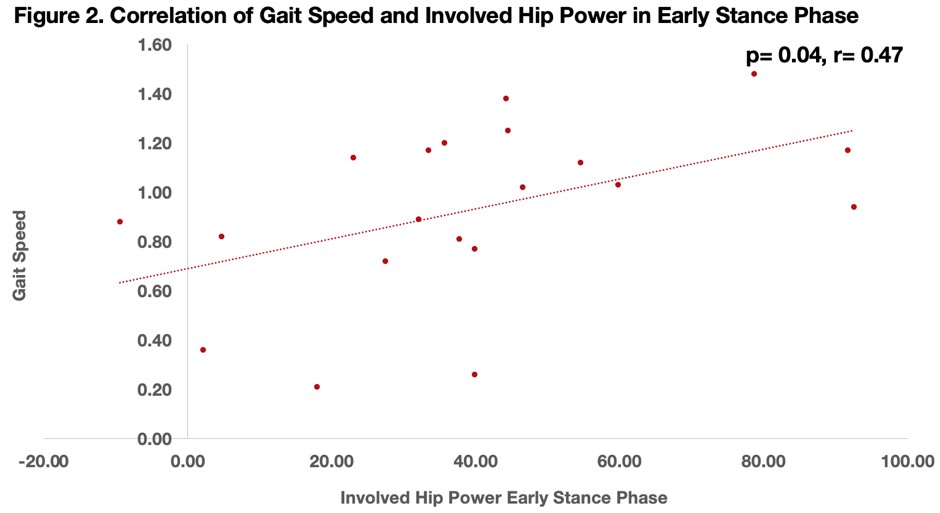
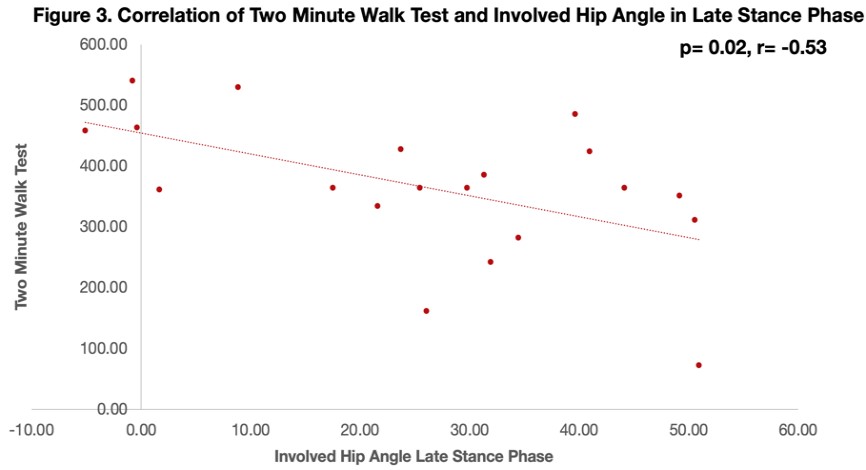
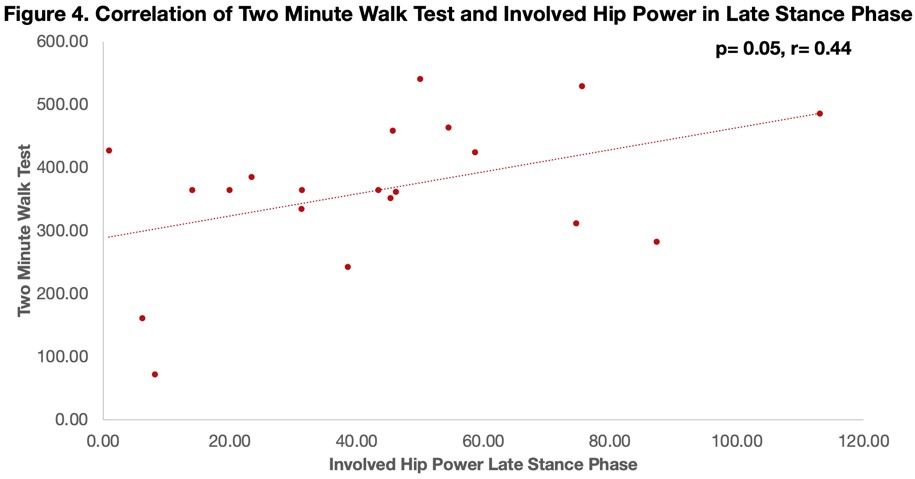
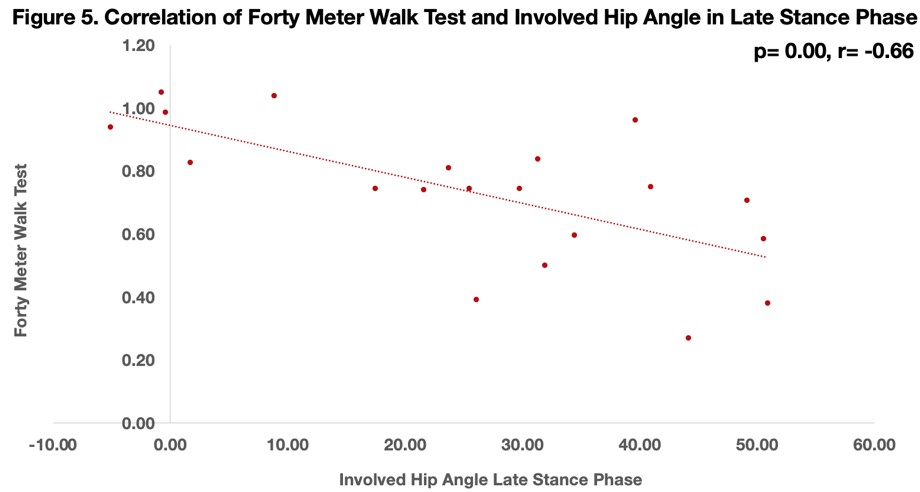
Osteoarthritis is the most common joint disease in the world. [12] Its prevalence in the hip joint is observed to have dramatic adverse effects on the quality of life of aging adults and can contribute to more significant health issues. [1] Hip osteoarthritis (HOA) results in progressive joint pain and muscle loss, abnormal hip mechanics, and poor functional performance. [4, 8] To date, it is unknown how the abnormal hip mechanics brought on by HOA relate to functional performance. Therefore, this study aims to compare the relationship between deficits in hip mechanics of the frontal (primary) and sagittal (secondary) planes onto physical function, using validated functional performance tests in adults with HOA. We hypothesized that more significant deficits in the involved limb’s hip mechanics (angle, moment, power) would be associated with poorer Two Minute Walk Test (2MWT) and Forty Meter Walk Test (40MWT) performance. We also hypothesized that more significant deficits in hip mechanics would be associated with greater hip abduction, knee extension, and knee flexion weakness of the involved limb. This hypothesis was explored, but no significant differences were found during the study. The results of this study demonstrated the following: 1) slower gait speeds were associated (p= 0.04, r= -0.47) with greater hip flexion angle in the late stance phase of the involved limb during self-selected walking; 2) faster gait speeds were associated (p= 0.04, r= 0.47) with greater hip power output in the early stance phase of the involved limb during self-selected walking; 3) more distance covered during the 2MWT was associated (p= 0.02, r= -0.53) with greater hip flexion angle in the late stance phase of the involved limb during self-selected walking; 4) more distance covered during the 2MWT was associated (p= 0.05, r= 0.44) with greater hip power in the late stance phase of the involved limb during self-selected walking; 5) slower 40MWT times were associated (p< 0.01, r= -0.66) with greater hip flexion angle in the late stance phase of the involved limb during self-selected walking. No relationships between muscle strength and functional performance were observed. These findings demonstrate that adaptations in walking gait patterns of adults with HOA affect their overall functional performance, which could influence their quality of life and ability to participate in activities of daily living. Future studies can look at other planes of motion to attempt to build a more complete profile of the functional adaptations arising ii from HOA. This more complete profile can be used to address adults’ concerns, improve quality of life metrics, and offset functional disability that is influenced by HOA.
Introduction
Osteoarthritis is the most common joint disease, affecting approximately 32 million adults within the United States, and contributes to nearly $140 billion/year in healthcare costs needed to manage this debilitating disease. [19, 29] The hip joint is one of the most common joints affected by the disease leading to debilitating joint pain and functional limitations. [1, 9, 14, 24] Hip osteoarthritis (HOA) disproportionately affects older adults 75 years of age and older and relates to a greater risk of a sedentary lifestyle contributing to an increased risk of health-related comorbidities. Additionally, HOA has been shown to increase age-adjusted mortality by 20 percent. [12] Adults with HOA demonstrate poor hip mechanics with tasks such as walking and transferring in/out of chairs. As it pertains to walking, adults with HOA demonstrate slower walking speed, shorter step length, and longer stance time on the non-involved limb. [3,4] Regarding transferring in/out of chairs, adults with HOA demonstrate a reduced hip range of motion and greater reliance on the non-involved limb when compared to healthy-matched peers. [8] Additionally, adults with HOA demonstrate decreased physical function, muscle strength, and atrophy related to the disuse of the involved limb. More specifically, hip abduction, knee extensor, and knee flexor strength are significantly reduced in the HOA-affected limb relative to a healthy limb. Cross-sectional areas of the quadriceps, hamstrings, and gluteal muscles have shown significant reduction when compared to the healthy limb or healthy-matched peers. Adults with HOA have also been shown to have poorer functional performance on the Two Minute Walk Test (2MWT) and 30-Second Sit-to-Stand Test when compared to healthy peers. [6, 8]
The current strategies for managing HOA include exercise, weight management, braces, nonsteroidal anti-inflammatory drugs, topical treatments, and corticosteroid injections. [12, 13, 18] These methods are implemented to decrease pain and improve mobility brought on by the HOA-affected limb. When managing HOA becomes too difficult, or pain levels are too high to tolerate, total hip arthroplasty is the recommended strategy. Unfortunately, as hip pain is commonly resolved following surgery, adults still present with poor hip mechanics and functional performance. Ultimately, these impairments can result in reduced physical function and increased risk for sedentary health behavior even after the HOA pain is resolved.
Therefore, this study aims to compare the relationship between deficits in hip mechanics of the frontal (primary) and sagittal (secondary) planes onto physical function, using validated functional performance and muscle strength metrics in adults with HOA. We hypothesized that greater deficits in the involved limb’s hip mechanics (angle, moment, power) would be associated with poorer 2MWT and Forty Meter Walk Test (40MWT) performance. We also hypothesized that greater deficits in hip mechanics would be associated with greater hip abduction, knee extension, and knee flexion weakness of the involved limb.
Methods
This project involved bringing adults with late-stage HOA into the marker-based Gait Laboratory at the VA Salt Lake Health Care System. Adults completed several validated gait tests of 2MWT and 40MWT. Data collected this way was compared and processed via Nexus 2.1.1 software (Vicon, Oxford Metrics Ltd., Oxford, UK) and Visual3D (C-motion, Inc., Germantown, MD, USA). A cohort of 20 adults was used in this quality improvement project, with their pre-operative data collected 1-2 weeks before undergoing total hip replacement due to late-stage HOA.
All adults with HOA underwent testing at the VA Gait Laboratory using instrumented walkway with 12 embedded force plates (Bertec, Columbus OH, USA) and 24 infrared cameras (Nexus, Centennial CO, USA). Adults with HOA will be asked to 1) walk on a 5-meter 4 walkway, and we will analyze ten clean foot strikes between both limbs on the embedded force plates and 2) perform the 2MWT and 3) perform the 40MWT to compare hip mechanics of affected and nonaffected HOA limbs.
All adults were told the following basic script for the 2MWT:
- We are going to have you walk for two minutes. We will have a timer counting down, so you do not need to worry about how much time is left in the test.
- The goal is to walk as far as possible within the two-minute window. There is no need to achieve a specific distance. Walk at a speed that is comfortable and manageable for you.
- We will do two practice walk tests before we collect the test trial. This will allow us to ensure that everything is working correctly and that you are not in any pain.
- If you need to stop the trial at any point, please let us know, and we can stop. We go at your pace and your comfort level.
All adults were told the following basic script for the 40MWT:
- Start with both feet on the start line.
- At start, walk as quickly as possible while maintaining your balance.
- Walk to the 10-meter mark, turn around, and return to the start mark.
- You will repeat this four times until you walk 40 meters between the start lines and the 10-meter mark.
- Go ahead and get ready to start.
- If you need to stop the trial at any point, please let us know, and we can stop. We go at your pace and your comfort level.
The 5m Walkway Test was used to collect data to compare to the distance covered during the 2-Minute Walk Test. The 40MWT was used to determine how functional an individual’s gait was and how the compensations brought on by HOA affected their ability to perform functional movements.
After the data has been collected, the data collected during the 2MWT and 40MWT was determined to be viable and appropriate to use for further analysis. This was integral as we used the two tests to comprehensively understand HOA and subsequent compensations. Kinematic and kinetic data were recorded and synchronized using Nexus 2.1.1 software (Vicon, Oxford Metrics Ltd., Oxford, UK). Inverse dynamic computation and extraction of hip mechanic variables will be conducted using Visual3D (C-motion, Inc., Germantown, MD, USA). Trajectory and analog data were low-pass filtered at 6 Hz and 25 Hz respectively using a fourth-order Butterworth digital filter based on residual analysis.
Results
Slower gait speeds were associated (β=-24.2, t=-2.27, p=0.04, Figure 1) with greater hip flexion angle in the late stance phase of the involved limb during self-selected walking. Faster gait speeds were associated (β=36.2, t=2.27, p=0.04, Figure 2) with greater hip power output in the early stance phase of the involved limb during self-selected walking. More distance covered during the 2MWT was associated (β=-0.08, t=-2.26, p=0.02, Figure 3) with less hip flexion angle in the late stance phase of the involved limb during self-selected walking. More distance covered during the 2MWT was associated (β=0.11, t=2.06, p=0.05, Figure 4) with greater hip power in the late stance phase of the involved limb during self-selected walking. Slower 40MWT times were associated (β=-53.1, t=-3.74, p=0.00, Figure 5) with greater hip flexion angle in the late stance phase of the involved limb during self-selected walking. These results reflect that hip 5 angle and power were the most affected biomechanical measures of late-stage HOA. The biomechanical measures demonstrate that walking gait adaptations in late-stage HOA include a shorter stride and less muscular power produced per stride. These functional decrements mean that adults with HOA will walk slower and cover less distance, inferring an overall decrease in the ability to perform activities of daily living (ADL).
Discussion
The results of this project highlighted deficiencies in two areas, hip angle and hip power, during the functional performance tests of adults with HOA. Hip angle relates to the degrees of flexion and extension between the hip joint and torso, while hip power is the muscular force exerted through the joint. A medium negative correlation (r=-0.47) was found between functional performance in validated gait trials and hip angle. The decreased hip angle in the late stance phase, post-mid-stance until toe-off of the gait cycle, suggests that adults with late-stage HOA take shorter strides. This means a slower walking gait, more steps needed to cover a required distance, and overall limitations in mobility in ADLs. In contrast, a medium positive correlation (r=0.47) was found between the 2MWT and gait speed. We can conclude that adults with more functional HOA move faster and produce more power per stride. Adults with more functional HOA and the ability to move better regarding ADLs suggest fewer pain symptoms or greater muscular strength. However, further research is needed to explore those relationships further. Limitations in ADLs may also cause a cascade of effects. This includes decreased physical activity, which may lead to chronic diseases offset by regular physical activity. This demonstrates how HOA and the functional adaptations in the gait may lead to drastic overall life changes. Therefore, finding the deficits in hip angle and hip power may lead to the ability of adults to continue to participate in ADLs and not develop additional chronic diseases.
Potential factors influencing the validity of the results include non-diagnosed osteoarthritis or other orthopedic conditions, inaccurate placement of tracking markers, small sample size (n=20), and only male participants being involved in the study. Underlying and non-diagnosed orthopedic conditions can contribute to gait compensation patterns that we concluded to result from HOA. This could mean that HOA could be minorly responsible for the resulting hip angle and power conclusions. Inaccurate placement of tracking markers could also influence the results. While known and consistent anatomical markers were used for tracking marker placement, they were applied by a researcher, which could lead to human error, influencing the conclusions found concerning biomechanical data. The cohort size increased from 10 to 20 over this project. This was done to improve the quality of the relationships, if any were to exist, and reduce bias from potential outliers skewing the data. Finally, the data may look different if female participants were involved in this study. Different anatomical structures, male versus female, may influence our findings. In addition, female adults may have different compensation patterns than male participants and may influence the resulting hip biomechanics data.
References
Allison, K., et al., Gluteal tendinopathy and hip osteoarthritis: Different pathologies, different hip biomechanics. Gait Posture, 2018. 61: p. 459-465.
Bahl, J.S., et al., Biomechanical changes and recovery of gait function after total hip arthroplasty for osteoarthritis: a systematic review and meta-analysis. Osteoarthritis Cartilage, 2018. 26(7): p. 847-863.
Constantinou, M., et al., Hip joint mechanics during walking in individuals with mild-to-moderate hip osteoarthritis. Gait Posture, 2017. 53: p. 162-167.
Diamond, L.E., et al., Hip joint moments during walking in people with hip osteoarthritis: a systematic review and meta-analysis. Osteoarthritis Cartilage, 2018. 26(11): p. 1415-1424.
Gossec, L., et al., OMERACT/OARSI initiative to define states of severity and indication for joint replacement in hip and knee osteoarthritis. J Rheumatol, 2007. 34(6): p. 1432-5.
Hall, M., et al., Hip biomechanics during stair ascent and descent in people with and without hip osteoarthritis. J Orthop Res, 2017. 35(7): p. 1505-1514.
Harding, P., et al., Do activity levels increase after total hip and knee arthroplasty? Clin Orthop Relat Res, 2014. 472(5): p. 1502-11.
Higgs, J.P., et al., Individuals with mild-to-moderate hip osteoarthritis exhibit altered pelvis and hip kinematics during sit-to-stand. Gait Posture, 2019. 71: p. 267-272.
Hulet, C., et al., [Functional gait adaptations in patients with painful hip]. Rev Chir Orthop Reparatrice Appar Mot, 2000. 86(6): p. 581-9.
Hurwitz, D.E., et al., Gait compensations in patients with osteoarthritis of the hip and their relationship to pain and passive hip motion. J Orthop Res, 1997. 15(4): p. 629-35.
Jones, D.L., A public health perspective on physical activity after total hip or knee arthroplasty for osteoarthritis. Phys Sportsmed, 2011. 39(4): p. 70-9.
Katz, J.N., K.R. Arant, and R.F. Loeser, Diagnosis and Treatment of Hip and Knee Osteoarthritis: A Review. JAMA, 2021. 325(6): p. 568-578.
Kolasinski, S.L., et al., 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol, 2020. 72(2): p. 220-233.
Kolk, S., et al., Gait and gait-related activities of daily living after total hip arthroplasty: a systematic review. Clin Biomech (Bristol, Avon), 2014. 29(6): p. 705-18.
Loureiro, A., et al., Individuals with mild-to-moderate hip osteoarthritis have lower limb muscle strength and volume deficits. BMC Musculoskelet Disord, 2018. 19(1): p. 303.
Loureiro, A., P.M. Mills, and R.S. Barrett, Muscle weakness in hip osteoarthritis: a systematic review. Arthritis Care Res (Hoboken), 2013. 65(3): p. 340-52.
Lunn, D.E., G.J. Chapman, and A.C. Redmond, Hip kinematics and kinetics in total hip replacement patients stratified by age and functional capacity. J Biomech, 2019. 87: p. 19-27.
Malik, A.T., et al., What Are the Costs of Hip Osteoarthritis in the Year Prior to a Total Hip Arthroplasty? J Arthroplasty, 2020. 35(2): p. 313-317.e1.
Maradit Kremers, H., et al., Prevalence of Total Hip and Knee Replacement in the United States. J Bone Joint Surg Am, 2015. 97(17): p. 1386-97.
O’Brien, J., et al., Improving physical activity, pain and function in patients waiting for hip and knee arthroplasty by combining targeted exercise training with behaviour change counselling: study protocol for a randomised controlled trial. Trials, 2018. 19(1): p. 425.
Polkowski, G.G. and J.C. Clohisy, Hip biomechanics. Sports Med Arthrosc Rev, 2010. 18(2): p. 56-62. 7
Rasch, A., et al., Reduced muscle radiological density, cross-sectional area, and strength of major hip and knee muscles in 22 patients with hip osteoarthritis. Acta Orthop, 2007. 78(4): p. 505-10.
Simonsen, E.B., et al., Bone-on-bone forces during loaded and unloaded walking. Acta Anat (Basel), 1995. 152(2): p. 133-42.
Steinhilber, B., et al., Stiffness, pain, and hip muscle strength are factors associated with self-reported physical disability in hip osteoarthritis. J Geriatr Phys Ther, 2014. 37(3): p. 99-105.
Sultan, A.A., et al., Hip Osteoarthritis Patients Demonstrated Marked Dynamic Changes and Variability in Pelvic Tilt, Obliquity, and Rotation: A Comparative, Gait-Analysis Study. Surg Technol Int, 2018. 32: p. 285-292.
van den Bogert, A.J., L. Read, and B.M. Nigg, An analysis of hip joint loading during walking, running, and skiing. Med Sci Sports Exerc, 1999. 31(1): p. 131-42.
Vissers, M.M., et al., Physical functioning four years after total hip and knee arthroplasty. Gait Posture, 2013. 38(2): p. 310-5.
Zeni, J., Jr., et al., Relationship between physical impairments and movement patterns during gait in patients with end-stage hip osteoarthritis. J Orthop Res, 2015. 33(3): p. 382-9.
Murphy, L.B., et al., Medical Expenditures and Earnings Losses Among US Adults With Arthritis in 2013. Arthritis Care Res (Hoboken), 2018. 70(6): p. 869-876.

