School of Medicine
58 Opioid Misuse in Rural and Urban Prostate Cancer Survivors
Tashianna Gray; Brock O'Neil; and Mia Hashibe
Faculty Mentor: Brock O’ Neil (Surgery, University of Utah)
Abstract
Background: Rural and urban cancer disparities in prostate cancer survival are well-documented. The cause of worse outcomes among rural prostate cancer survivors is not well-understood. Prior research has shown that rural communities have higher use of prescribed and illicit opioid use than many urban communities. Furthermore, opioid therapy is the utilization of drugs, short-term or long term to reduce pain. Patients that experience moderate pain may be prescribed weak opioids that include Codeine or Tramadol; while those who experience severe pain may be prescribed stronger opioids such as Morphine. These opioids can be taken in various ways including slow release and a needle under the skin. Their versatility can make them highly addictive in treatment options: post-surgery, radiation therapy, and systematic therapies. For instance, one in four patients receiving long-term opioid therapy in a primary care setting struggles with opioid addiction. This addiction can spiral and can have grave side effects in patients.
Objective: The purpose of this research is to investigate whether persistent opioid use after treatment may explain the observed worse survival among rural prostate cancer survivors. We hypothesize that rural patients are more likely to receive a prescription for opioids more than a year after prostate cancer treatment than urban counterparts.
Methods: Our methods include the retrospective cohort study using the Utah Population Database linked with all-payer claims data. More specifically, men with prostate cancer were diagnosed between 2012 and 2017. Also, we reviewed relevant literature that identified health disparities that rural patients have compared to urban patients.
Results: Reviewing this data, we identified 960 rural prostate cancer survivors and matched them to 6,026 urban counterparts. We found that rural survivors are older, more likely to be non-Hispanic white, have higher-stage disease at diagnosis, and forgo initial treatment compared to urban men.
Conclusions: Overall, differences in persistent opioid use after treatment for prostate cancer do not appear to explain observed differences between rural and urban prostate cancer survivors.
Persistent opioid use was not uncommon ranging from 12.6% to 19.9% and similar between rural and urban survivors. This trend was shown in all three figures; more specifically, patient use of opioids after the three different types of treatment is represented in those figures to interpret the insignificant differences.
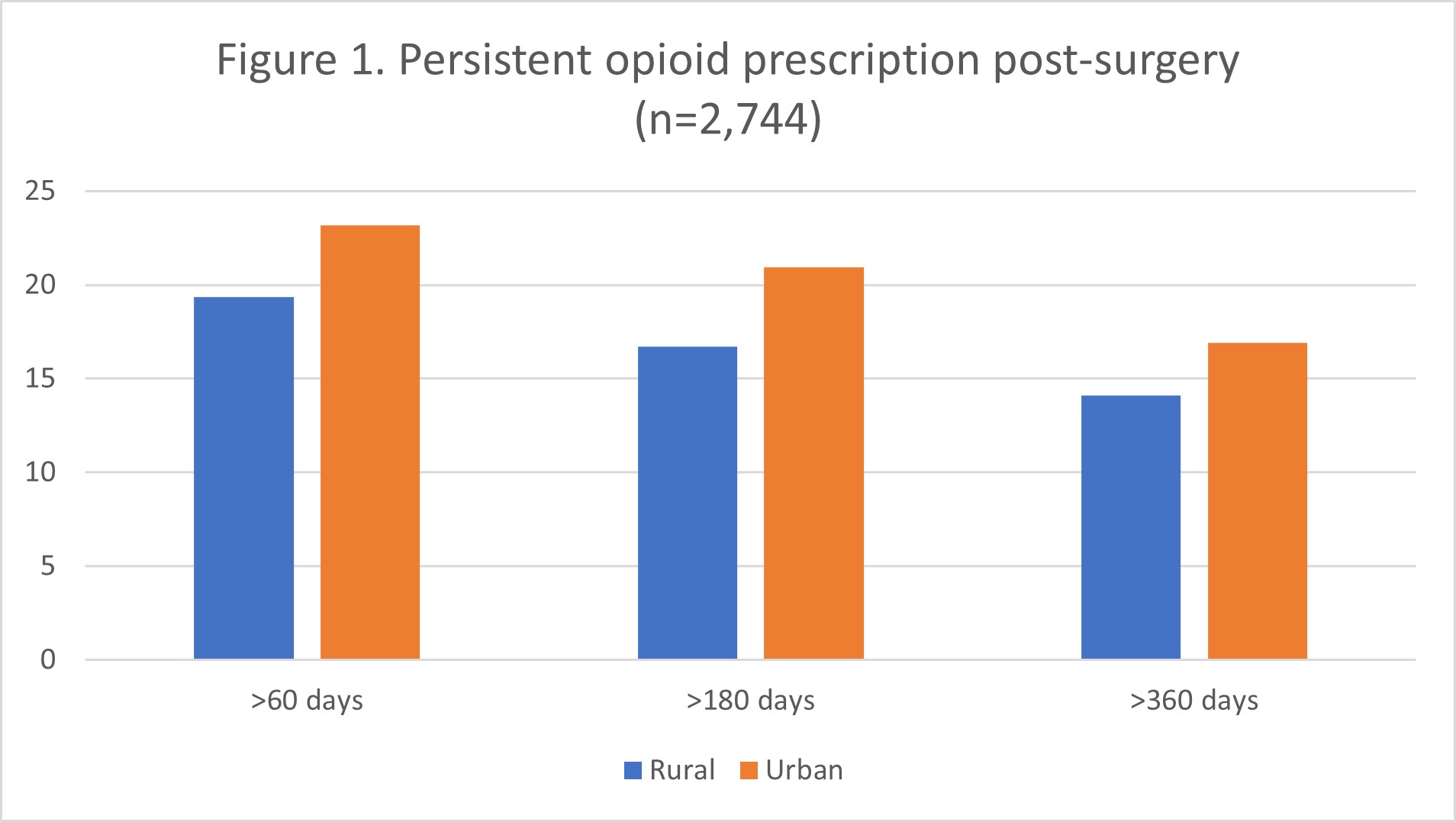
Figure 1. Persistent opioid prescription post-surgery
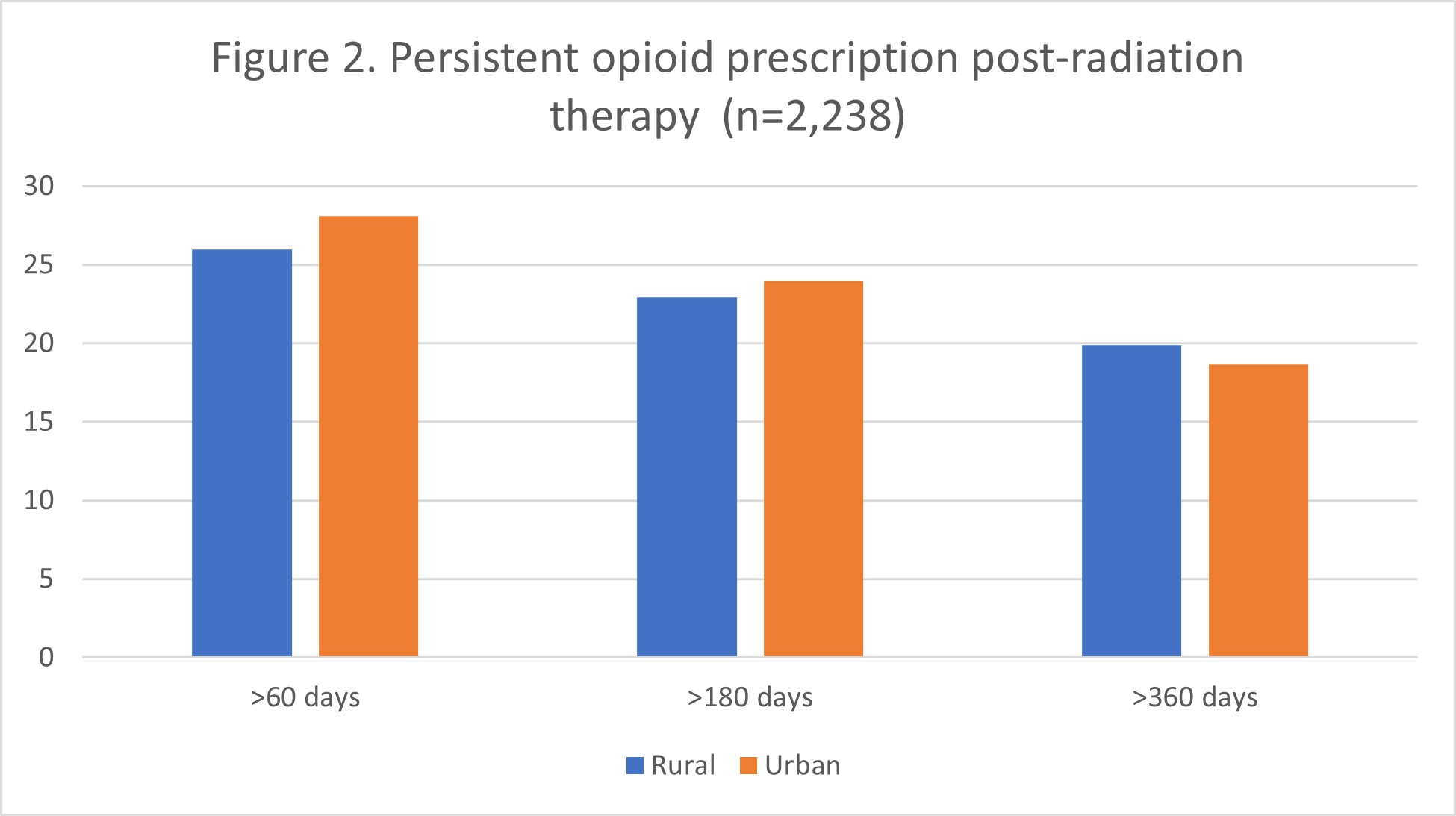 Figure 2. Persistent opioid prescription post radiation therapy
Figure 2. Persistent opioid prescription post radiation therapy
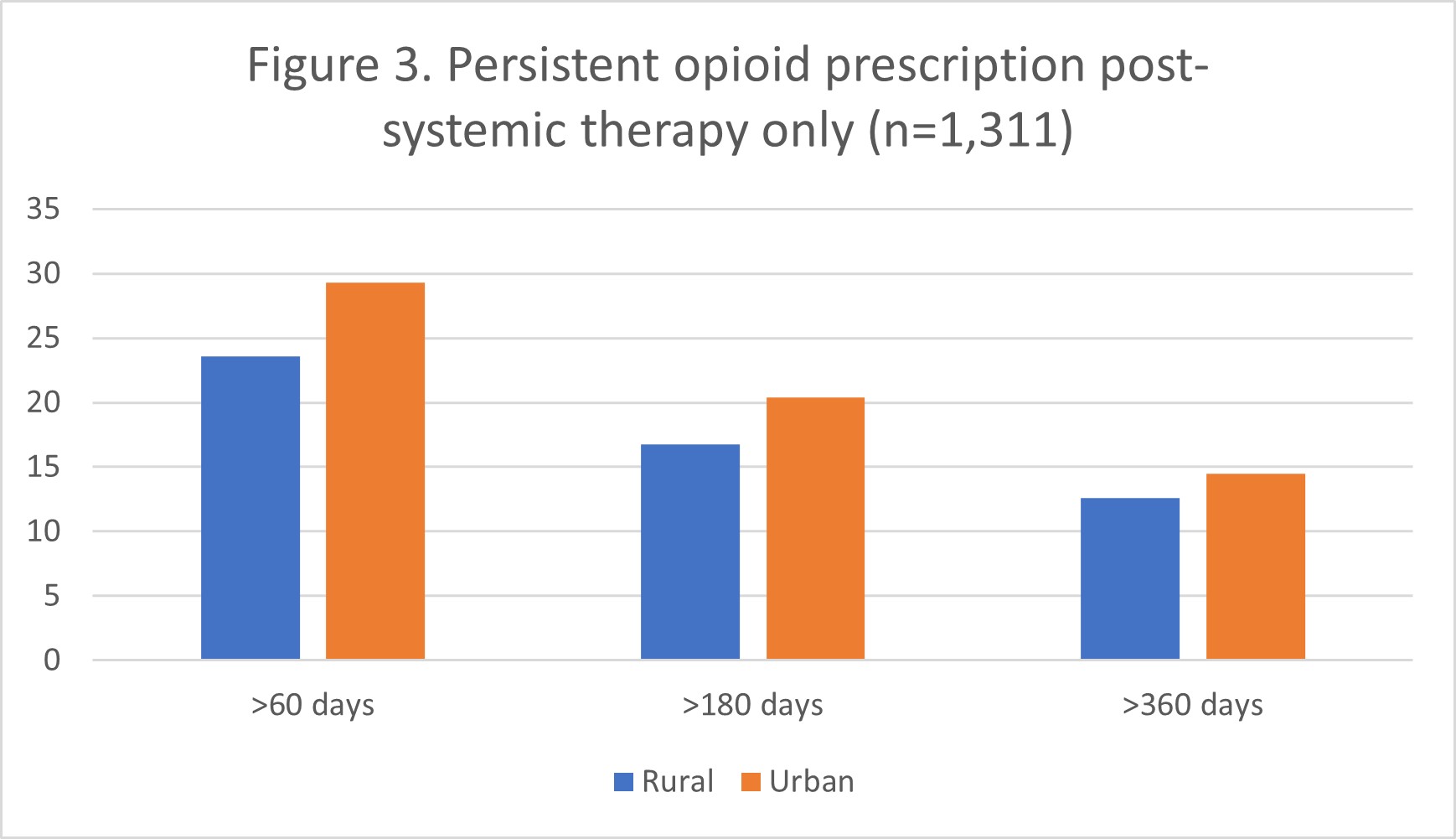
Figure 3. Persistent opioid prescription Post systemic therapy only
Bibliography
Centers for Disease Control and Prevention. (2017, August 29). Prescription opioids. Centers for Disease Control and Prevention. https://www.cdc.gov/opioids/basics/prescribed.html
Sullivan, M. D., & Howe, C. Q. (2013, December). Opioid therapy for chronic pain in the United States: Promises and perils. Pain. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4204477/

