School of Medicine
44 Planovalgus Deformities Aross Varying Body Mass Indexes: Two-Dimensional Analysis from WBCT
Megan Carter and Amy Lenz
Faculty Mentor: Amy Lenz (Orthopaedics, University of Utah)
Introduction
Progressive collapsing foot deformity (PCFD) is a complex foot and ankle condition characterized by peritalar subluxation [1]. Individuals with PCFD have unique and intricate morphologies with complex articular relationships, often causing pain, malalignment, and loss of function [2][3]. This foot deformity is more prevalent among high BMI patients, as their increased weight places higher stress on the medial longitudinal arch, causing it to flatten [4]. However, there is a scarcity of research investigating how BMI impacts the morphology of foot bones in PCFD patients. Typically, conditions of the foot and ankle, such as PCFD, are evaluated using x-rays and 2D measurements [5]. In this study, we aimed to observe several common 2D clinical measures of PCFD among groups of varying BMIs to check for statistical significance. We hypothesized that BMI would influence foot morphology and therefore, clinical measures would vary with BMI.
Methods
In this study, seventy-four patients (age: 44.4 ±18.4 years; 28 females, 98 feet) presenting with PCFD underwent WBCT scans (Planmed Verity; 0.4 x 0.4 x 0.4 mm voxels) with IRB approval. Using two-dimensional digitally reconstructed radiographs from DISIOR 2.1, comparisons were made across relevant clinical values determined from literature. Those chosen values were Talonavicular Coverage (TNC), Meary’s Angle (MA, sagittal), Calcaneal Inclination Angle (CIA), and Hindfoot Moment Arm (HMA). The data was then tested for normality using MATLAB. Parametric values (MA and CIA) were analyzed using a one-way ANOVA while non-parametric values (HMA and RNC) were analyzed using a Kruskal-Wallis test.
Results
The only statistically different clinical measure was HMA between BMI groups 2 and 3 (Group 2 = 25-29.99 BMI, Group 3 = 30-34.99 BMI). Comparisons of all other values among the varying BMI groups yielded no statistically significant p-values.
Discussion
The results from the 2D radiographs demonstrated a lack of significance among common 2D clinical measures, suggesting that BMI may not be a major factor in the morphology of PCFD. This information is important in understanding the etiology and treatment of PCFD. However, to further investigate these findings, the results from the 2D analyses should be compared with 3D measurements of the bones and joints. The bones of the foot have complex and unique orientations that are difficult to assess with conventional 2D radiographs.
Superimposition of these bones is often misrepresented in the conversion of 3D surfaces (bones) to 2D images (radiographs), leading to inaccurate measurements [6]. However, the development of weightbearing computed tomography (WBCT) has allowed accurate 3D visualization, comprehensive analyses, and a new grading system to report degenerative progression throughout the ankle joints [7]. This technology is a vital tool in the future of this study. Future work will include segmenting the WBCT scans of these PCFD patients and performing 3D evaluations of their bones. This data can then be compared to the 2D results, offering further insight into the role of BMI in PCFD. This study highlights the complexity of the foot and ankle complex as well as the need to consider complicated morphological variations of bones and joints when considering surgical intervention in PCFD.
Significance
These findings help surgeons to better understand the underlining mechanism of PCFD, while also suggesting that the selection of surgical procedures and treatments for PCFD may not need to be adapted for BMI. This information contributes to the growing database of information regarding PCFD, offering valuable insight that could be used to improve the diagnosis and treatment of pathological feet.
Acknowledgements: Funding was provided by the National Institutes of Health for the Medical Student Research Program. Additional funding was provided by the University of Utah for the Summer Program for Undergraduate Research
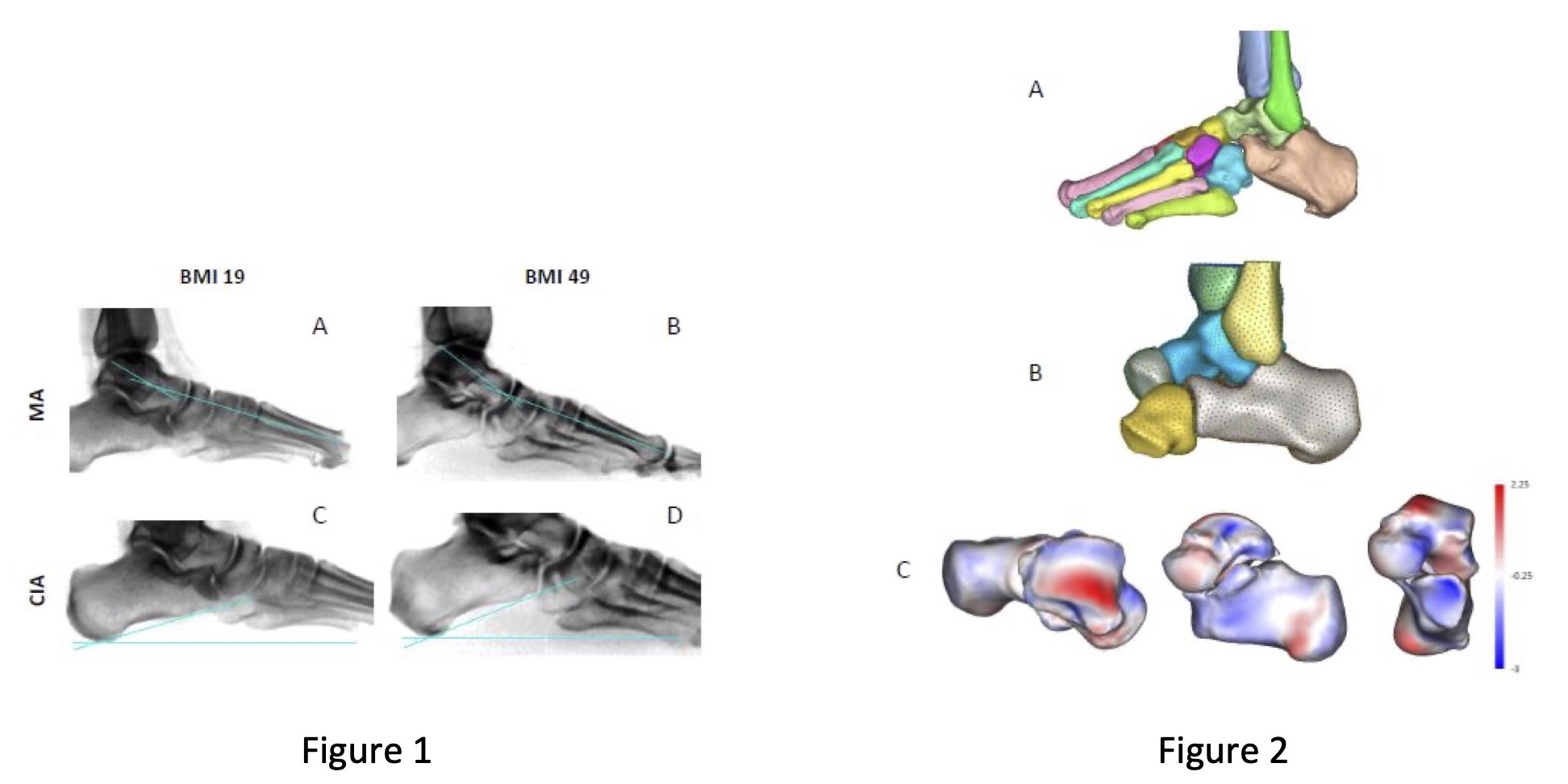
Figure 1: DISIOR digitally reconstructed radiographs. (A) Patient of BMI 19 with MA of -13.45°, (B) Patient of BMI 49 with MA of -16.46°, (C) Patient of BMI 19 with CIA of 16.05°, (D) Patient of BMI 49 with CIA of 21.72°
Figure 2: Future work with 3D modeling. (A) Segmented bones from Mimics Innovative Suite, (B) Multi-domain shape modeling, (C) Joint measurement analysis performed on segmented bones
References
[1] Godoy-Santos AL, Schmidt EL, Chaparro What Are the Updates on Epidemiology of Progressive Collapsing Foot Deformity? Foot Ankle Clin. 2021 Sep;26(3):407-415. doi: 10.1016/j.fcl.2021.05.006. Epub 2021 Jun 27. PMID: 34332726.
[2] Toullec Adult flatfoot. Orthop Traumatol Surg Res. 2015 Feb;101(1 Suppl):S11-7. doi: 10.1016/j.otsr.2014.07.030. Epub 2015 Jan 13. PMID: 25595429.
[3] Flores DV, Mejía Gómez C, Fernández Hernando M, Davis MA, Pathria MN. Adult Acquired Flatfoot Deformity: Anatomy, Biomechanics, Staging, and Imaging Findings. Radiographics. 2019 Sep-Oct;39(5):1437-1460. doi: 1148/rg.2019190046. PMID: 31498747.
[4] Rosende-Bautista C, Munuera-Martínez PV, Seoane-Pillado T, Reina-Bueno M, Alonso- Tajes F, Pérez-García S, Domínguez-Maldonado G. Relationship of Body Mass Index and Footprint Morphology to the Actual Height of the Medial Longitudinal Arch of the Int J Environ Res Public Health. 2021 Sep 17;18(18):9815. doi: 10.3390/ijerph18189815. PMID: 34574735; PMCID: PMC8465021.
[5] Perry MD, Mont MA, Einhorn TA, Waller The validity of measurements made on standard foot orthoroentgenograms. Foot Ankle. 1992 Nov-Dec;13(9):502-7. doi: 10.1177/107110079201300902. PMID: 1478578.
[6] Richter M, de Cesar Netto C, Lintz F, Barg A, Burssens A, Ellis The Assessment of Ankle Osteoarthritis with Weight-Bearing Computed Tomography. Foot Ankle Clin. 2022 Mar;27(1):13-36. doi: 10.1016/j.fcl.2021.11.001. Epub 2022 Jan 31. PMID: 35219362.
[7] Conti MS, Ellis SJ. Weight-bearing CT Scans in Foot and Ankle Surgery. J Am Acad Orthop Surg. 2020 Jul 15;28(14):e595-e603. doi: 10.5435/JAAOS-D-19-00700. PMID

