Reflex Pathways
Caleb Bevan
Objective 12: State the anatomy and function of key reflex pathways.
A reflex arc consists of the following components:
- a sensory receptor which picks up information from the environment;
- a sensory neuron (which may or may not be the same as the receptor) to carry the information to the central nervous system);
- an integrating center (i.e., the CNS);
- a motor neuron to innervate the effector;
- an effector (generally, skeletal muscle, also called striated or voluntary muscle).
Although we often call things like braking for a small child or springing out of the blocks at the starting gun “reflexes,” technically, these are complex behaviors. Reflexes are hard-wired and require no conscious thought.
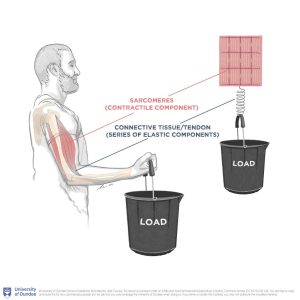 It is critically important for the muscles to detect passive stretch (for example, when a load suddenly increases in weight) in our muscles. This doesn’t seem important at first until we consider walking on uneven ground with (say) rocks shifting under our feet. In order to remain upright, we need to immediately recognize the muscle stretch that results and respond to it quickly.
It is critically important for the muscles to detect passive stretch (for example, when a load suddenly increases in weight) in our muscles. This doesn’t seem important at first until we consider walking on uneven ground with (say) rocks shifting under our feet. In order to remain upright, we need to immediately recognize the muscle stretch that results and respond to it quickly.
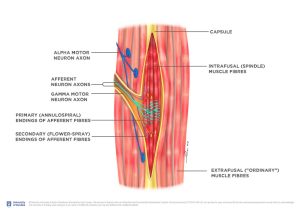
The myotatic reflex (also called the stretch reflex or monosynaptic reflex) is the fastest reflex in the human body. The various names sketch out the elements of the reflex. It starts with a stretch receptor, anatomically called the intrafusal muscle fiber or muscle spindle receptor. (Everything seems to have two or three names.)
There is exactly one synapse between the sensory receptor and motor neuron effector — hence the name “monosynaptic”. The effector is a lower motor neuron (α motor neuron) with its cell body in the anterior horn of the spinal cord. The α motor neuron axon terminals form neuromuscular junctions where acetylcholine (ACh) is released onto skeletal muscle cells.
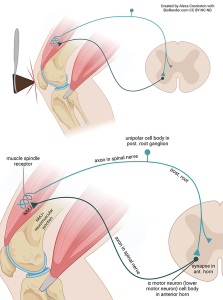
To review, then, there are two neurons and one synapse in the myotatic reflex.
The sensory arm (afferent limb) of the reflex is a muscle spindle receptor, with a modified dendrite in skeletal muscle, an axon which enters the spinal cord via the posterior root, and a cell body in the posterior root ganglion. This is a unipolar neuron.
There is a synapse between the muscle spindle receptor and the lower motor neuron (α motor neuron) in the anterior horn of the spinal cord.
The lower motor neuron sends an axon via the anterior root (efferent limb) to innervate the same muscle that originated the sensory signal.
Another way to break this down is to consider the functional steps in the reflex:
Some jerk hits your patellar tendon with a rubber hammer, stretching a muscle in quadriceps group and activating an intrafusal muscle fiber (stretch receptor; muscle spindle receptor).
The stretch receptor releases the excitatory neurotransmitter glutamate onto a lower motor neuron.
The lower motor neuron releases the excitatory neurotransmitter ACh to cause contraction of the quadriceps group muscle.
Synapses take time to operate, so reducing the processing to one synapse speeds this reflex considerably. It also utilizes the largest axons (large axons are faster) and the axons in this reflex are heavily myelinated (a myelin sheath, as we’ll see in Unit 13, increases the speed of conduction).

This infographic-style image breaks down the myotatic reflex into its steps. It also shows the inverse myotatic reflex, which strengthens the reflex action by relaxing the antagonist muscle (in this case, a muscle of the hamstring group) at the same time the agonist quadriceps is activated. This is accomplished with an inhibitory interneuron (purple) between the sensory receptor axon and the antagonist α motor neuron. This interneuron uses the amino acid glycine as an inhibitory neurotransmitter.
Almost every muscle has a stretch reflex and a way of testing it clinically, but that’s a long list and we won’t cover it here.

Living fully means we encounter painful stimuli from time to time. We protect ourselves from painful stimuli with the flexor (withdrawal) reflex. Say you reach for a rose but grab a thorn. A pain signal is sent to the cervical spinal cord, processed by one or several interneurons, which then activate the α motor neuron of a flexor muscle. Flexors reduce the angle of the elbow joint: the biceps, brachialis, and brachioradialis contract and remove the hand from the painful stimulus.
We protect ourselves from painful stimuli with the flexor (withdrawal) reflex. Say you reach for a rose but grab a thorn. A pain signal is sent to the cervical spinal cord, processed by one or several interneurons, which then activate the α motor neuron of a flexor muscle. Flexors reduce the angle of the elbow joint: the biceps, brachialis, and brachioradialis contract and remove the hand from the painful stimulus.
Most people are surprised to find out that this reflex is actually much slower than the stretch reflex. There are two main reasons for this. The afferent limb carrying the pain information into the CNS consists of unmyelinated or thinly myelinated axons that have a small caliber, among the smallest in a spinal nerve. Also, the information has to pass through several synapses and interneurons.
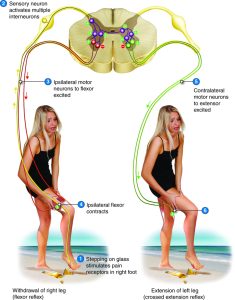
As for the myotatic reflex, this infographic shows the withdrawal reflex fully. We’ve already traced the flexor part of the reflex; now we add a crossed extensor reflex.
If we went around flexing our joints every time we stepped on something, we’d fall over a lot. For example, if you flex your left knee, you need to extend your right knee (try it and see). This is automagically taken care of by the crossed extensor reflex. The right knee is flexed by the flexor reflex; at the same time, interneurons send information to the contralateral side of the spinal cord and activate extensors (i.e. quads) and inhibits flexors (i.e. biceps femoris) on the left leg. The sensory information crosses the midline and causes the activation of an extensor muscle on the contralateral side, hence its name.

When we discussed the autonomic motor system, we saw how the pupil is controlled by the sympathetic and parasympathetic nervous system.
When the sympathetic response dilates or enlarges the pupil (mydriasis), norepinephrine is released onto the pupillary dilator muscle. This smooth muscle runs radially from the center of the pupil, so contraction of its fibers increases the diameter of the pupil.
When the parasympathetic response constricts or shrinks the pupil (miosis), acetylcholine is released onto muscarinic ACh receptors of the pupillary sphincter muscle. These muscle cells run in a band around the edge of the pupil, so contraction of its fibers decreases the diameter of the pupil. Belladonna or atropine, remember, are drugs that block these muscarinic ACh receptors and allow the dilator muscle to act unopposed.
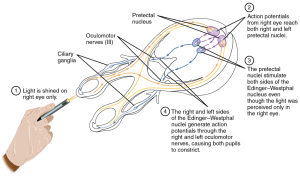
When we shine a light into the eye, the signal is carried by the optic nerve (CN II). Most of these ganglion cell axons end in the lateral geniculate nucleus of the thalamus but about 10% continue to the midbrain where they mediate visual reflexes like looking at a flash of light or the pupillary light reflex we’re discussing now. In this case, the axons end in the Edinger-Westphal nucleus, which is the name for the cluster of parasympathetic motor neuron cell bodies which lie deep in the midbrain. These preganglionic axons extend out to the ciliary ganglion where they synapse onto postganglionic neurons that travel a short distance into the iris itself. There, their axon terminals release acetylcholine onto muscarinic receptors, causing the pupil to shrink (miosis).
In this way we can quickly test the function of the midbrain. Extensive brain damage can affect the midbrain, so the absence of a normal pupillary light reflex is a very grave clinical sign.
Damage to this pathway causes nystagmus, a flickering of the eyes from one side to another. This is a pretty strong clinical sign of damage to the vestibular apparatus, or vestibular nerve, or medulla (rarely), or flocculonodular lobe (commonly, especially with excessive ethanol consumption which slows and disrupts the calculation).

Earlier, we discussed the clinical distinction between damage to an upper motor neuron and a lower motor neuron.
Damage to an upper motor neuron causes hyperreflexia (increased speed of reflexes, such as the myotatic reflex) and spastic (rigid) paralysis.
Damage to a lower motor neuron causes hyporeflexia (slow or absent reflexes) and flaccid (floppy, weak) paralysis.
One way to assess upper motor neuron damage is through a test called the Babinski reflex or Babinski sign. Unlike the normal reflexes we’ve been studying, this is an abnormal reflex.
In a normal adult, if the clinician strokes the bottom (plantar)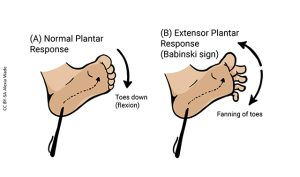 surface of the foot with the spoon-shaped handle of a reflex hammer, or with a key, the patient’s toes will flex as if to grasp the object.
surface of the foot with the spoon-shaped handle of a reflex hammer, or with a key, the patient’s toes will flex as if to grasp the object.
In babies, and adults with damage to the corticospinal tract, the Babinski sign is present, the toes extend and fan out. In babies this is because the necessary pathways for the plantar flexor response have not yet been fully myelinated. In adults, this is because of a spinal cord injury or other condition causing damage to the upper motor neurons of the lateral corticospinal tract.
Media Attributions
- Load reflex © Cowley, Lissie / University of Dundee is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- Intrafusal fiber anatomy © Cowley, Lissie / University of Dundee is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- Knee © Alexa Crookston is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- Reflex myotatic nerve © Cenveo / Carnegie Mellon University / Open Learning Initiative is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Withdrawal Reflex © Alexa Crookston is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- Bronte quote © Jim Hutchins is licensed under a Public Domain license
- Reflex withdrawal nerve © Cenveo / Carnegie Mellon University / Open Learning Initiative is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Reflex pupil © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- Pupil reflex pathway © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- Upper and lower neurons and pathways © Alexa Crookston is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- Babinski Sign © Alexia Wade is licensed under a CC BY-SA (Attribution ShareAlike) license

