Interdisciplinary Treatment Approach to Youth with Intellectual or Developmental Disabilities and Co-occurring Mental Health Conditions
Ashley Greenwald; Erika Ryst; Diane D. Thorkildson; and Lauren Brown
Greenwalk, A., Ryst, E., Thorkildson, D. D., & Lauren B. (2024). Interdisciplinary treatment approach to youth with intellectual or developmental disabilities and co-occurring mental health conditions. Developmental Disabilities Network Journal, 4(1), 92-116.
Plain Language Summary
People with developmental disabilities sometimes have mental health needs. When needs are not met, people struggle to live meaningfully in their homes and communities. This paper discusses the importance of having professionals, such as doctors and therapists, work together so that good plans can be made to support the person’s needs at one time. The importance of having the person with the disability and their family members at the table for all planning and goal setting is talked about.
The model that was built and covered in this paper is called the Intensive Team Consultation (ICT) model. The ICT process is explained and includes information about the team members who participated, how often the team would meet, what type of information the team would collect and review, how the team would come up with ideas for supporting the person with a disability, and how the team would make sure that the plan was working to help the person and their family meet their goals.
Several pages of this paper give an example of a person named Eric that the ICT helped. Eric was 15 years old and had a learning disability, attention-deficit/hyperactivity disorder, and he was anxious and depressed. Eric was hitting his mom and he hated going to school. The team worked together to help teach Eric’s mom how to be happy and positive with her son. The team also helped Eric learn new skills about how to calm down when he was upset and how to talk to other people to get what he needed. By the end of ICT, Eric was no longer hurting his mom, he was doing online school, and he even got a great job.
The last part of the paper shares some thoughts about why working together is important and what made ICT successful. The ICT model works best when the whole family is willing to participate, when the professionals on the ICT can work together, and when the goals and needs of the person with a disability are at the front of all plans being made.
Abstract
Many individuals with Intellectual and/or Developmental Disabilities (IDD) have co-occurring mental health needs, yet service delivery options often do not allow for the integrated delivery of mental health treatment and social behavioral support services. Siloed treatment approaches often result in lack of collaboration between providers, increasing the difficulty in accessing comprehensive and coordinated treatments and reducing treatment potential and effective outcomes. Additionally, many service providers in behavioral support services are not trained to address significant mental health needs. Similarly, providers of mental health services lack experience in modifying practices for differing cognitive needs. The lack of cross-training and cross-collaboration makes it difficult for an individual or family member to access appropriate treatment, sometimes resulting in crisis situations when coordinated, comprehensive interventions are absent. This paper discusses the need for delivering services in a coordinated model, presents a pilot program model in detail, highlights the relationships needed for collaboration, and addresses the importance of inclusion of the person with lived experience in overall treatment planning. Outcomes of the pilot model are presented, including description of a case study of a youth with both IDD and co-occurring mental health conditions who made functional improvements in response to an interdisciplinary, collaborative approach despite failure of multiple previous siloed interventions. Implications for policy development and community-based partnerships are discussed.
Introduction
Individuals with intellectual and/or developmental disabilities (IDD) have high rates of co-occurring mental health conditions (IDD-MH). While the heterogeneous methodology of prevalence studies makes it difficult to pinpoint definitive rates of IDD-MH in IDD, the current literature indicates that about 65-70% of individuals with autism and 35-50% of IDD meet criteria for at least one mental health condition (Bougeard et al., 2021; Khachadourian et al., 2023; Munir, 2017). The presence of IDD-MH in youth represents both a challenge and an opportunity—as many mental health conditions have robust interventions that can substantially improve quality of life and functional outcome. However, most youth with IDD-MH conditions do not access appropriate or effective mental health care.
Co-occurring mental health conditions considerably increase the challenge of both diagnosis and treatment. Mental health conditions are generally diagnosed through clinical interview and symptom presentation. The wide cognitive range and communication problems within IDD can make personal interviewing difficult and cause caregivers’ uncertainty when trying to describe the child’s mental state. Professionals within the field sometimes disagree as to whether behavioral and emotional conditions represent their own diagnostic categories or should be viewed instead as symptom clusters within the neurodevelopmental disability (for example, irritability could be viewed as a symptom secondary to autistic spectrum disorder, or as a symptom of an underlying mood disorder). Frequent overlap between psychiatric symptoms and possible IDD symptoms can create the possibility of misdiagnosis (for example misclassifying the negative symptoms of schizophrenia as belonging to an autism spectrum disorder). Conversely, “diagnostic overshadowing” of a primary IDD condition can cause clinicians to miss treatable, co-occurring mental health conditions. Psychiatric symptoms can also present differently in the neurodevelopmental disability population, making it hard for mental health clinicians without experience in IDD to identify them (Matson & Nebel-Schwalm, 2007; Ozonoff et al., 2003; Simonoff et al., 2008).
When mental health conditions in youth with IDD are left unaddressed, a plethora of potential negative outcomes occur. Individuals with IDD-MH experience longer emergency department wait times for placement in higher levels of care (Pinals et al., 2022); overrepresentation in carceral and forensic settings (Morris & Zisman-Ilani, 2022), and inappropriate placement in residential settings because of a lack of community supports (U.S. Department of Justice [U.S. D.O.J.], 2022). Aggressive behavior, which often results from unaddressed mental health conditions, is associated with fewer…
…social relationships, exhaustion of social support, placement in restrictive school or residential settings, physical intervention, increased risk of being bullied or victimized, increased stress levels in caregivers, and decreased quality of life in the affected individual and his/her family. (Constantino et al., 2020, p. 4)
The lack of early identification and intervention frequently leads to symptom exacerbations, crisis situations, and repeated psychiatric hospitalizations. When behavioral and psychosocial community interventions are unavailable, youth receive extensive polypharmacy (treatment with multiple psychotropic medications, frequently in nonevidence-based combinations) and often ultimately end up in highly restrictive and controlled residential treatment settings far from the individual’s natural community supports (Pinals et al., 2022).
There are several evidence-based interventions for mental health conditions and associated symptoms affecting the IDD population. For example, cognitive-behavioral approaches, motivational interviewing, dialectical behavioral therapy, supportive therapy, exposure therapy, imagery rehearsal therapy, and relaxation training all have evidence supporting their use in individuals with IDD (Gentile & Gillig, 2012; Singh, 2016). Positive behavior support strategies and applied behavior analysis provided by Board-Certified Behavior Analysts (BCBAs) also have a substantive literature supporting their use in reducing the problematic behaviors that frequently accompany developmental disabilities, and also emerging literature applying these techniques to mental health issues (Clark et al., 2020; Harvey et al., 2009; Summers et al., 2022); however, lack of knowledge about these modalities among traditional mental health treatment providers means that these types of interventions are frequently underutilized (Constantino et al., 2020). Pharmacological interventions also have their place as important tools in reduction of morbidity associated with IDD-MH (McDougle et al., 2005; West et al., 2009), but should only be used within a comprehensive, multi-modal, and integrated treatment plan (National Center for START Services, University of New Hampshire Institute on Disability, 2023).
Significant barriers to access of mental health services and supports for individuals with IDD-MH stem from a long-standing division between mental health and developmental disabilities service systems in most states (Pinals et al., 2022). Fragmentation of these services make it difficult for individuals with IDD and their families to navigate, particularly when eligibility criteria for each system often exclude individuals with “niche” conditions of IDD-MH. The resulting “pass the parcel” situation leaves individuals with IDD-MH shuttling back and forth between the mental health and developmental disabilities systems and receiving siloed care from professionals who lack the intersectional understanding required for optimal outcomes (Son et al., 2019).
In fact, one study indicates that less than half of families of individuals with IDD-MH report satisfaction with their mental health treatment services (Holingue et al., 2020). Problems and barriers reported by these families include lack of assistance during crises; lack of choice in services, poor communication and coordination between service providers, and a need for providers to have more specialized training. A scoping review on access to mental health care for individuals with IDD-MH found that organizational access barriers include siloing of service sectors, competing service models, failure of interagency communication, inconsistent eligibility criteria, conflict/competition between services, and unclear referral pathways (Whittle et al., 2018).
The frequency of co-occurring mental health conditions within the IDD population and the potential benefits of treating these conditions demand new and innovative solutions to overcome these access barriers. Currently, there is only limited evidence within the literature regarding such solutions. However, the existing evidence and expert recommendations suggest that interdisciplinary, cross-system teamwork is essential to address these issues.
For example, Gathright et al. (2016) described an interdisciplinary model of care for inpatient child psychiatry that included collaborative, trauma-sensitive, child and family-centered care. This innovative program used a comprehensive assessment by an interdisciplinary team consisting of a child psychiatrist, child psychologist, speech and language pathologist, occupational therapist, social worker, nurses, milieu manager, and special education teacher to develop a detailed intervention plan. Medication wash-out for each child occurred at the beginning of the hospitalization to allow re-examination of the child’s functioning. Families were a critical part of the team and were invited to visit and participate at any time (“open hours”) instead of being limited to restricted visiting hours as is typical in most child psychiatry inpatient settings. Finally, a clinical case manager followed the patients for 90-days post-discharge to communicate with multiple systems (home, school, and community providers) and ensure that recommended treatment interventions were followed.
It should be noted that while the population served by this model was not exclusively an IDD population, the mean Full Scale Intelligence Quotient (FSIQ) in the study sample was 79.2 (with a range of 36 to 120 and mode of 73), and a significant portion of the children had diagnoses of intellectual disability (13.3%), borderline intellectual functioning (9.7%), communication disorders (37%), and autism spectrum disorder (17.1%; Gathright et al., 2016). The authors found that this model resulted in better outcomes such as reduced polypharmacy and antipsychotic use at discharge, reduced use of seclusion and restraint, and reduced readmission rates compared to usual inpatient psychiatric care.
Another example of an innovative psychiatric inpatient model to address problem behavior in youth with IDD also included close collaboration of multiple disciplines to provide optimum care (Romani et al., 2021). The primary team included a child and adolescent psychiatrist, a dual-certified psychologist and behavior analyst, a licensed clinical social worker, nurses, and direct care behavior specialists with consultation as needed from speech-language pathologists and occupational therapists. Caregivers, school staff and outpatient providers were invited to take part in training sessions on individualized interventions for the patients. Like the Gathright et al. model, this program showed superior results compared to usual treatment, with a greater than 90% reduction in problem behaviors 66.3% of the time.
Several outpatient models of comprehensive, integrated, interdisciplinary care for individuals with IDD-MH also exist. The START (Systemic, Therapeutic, Assessment, Resources and Treatment) program is perhaps the most widely disseminated such program in the United States (Kalb et al., 2019). Certified START model programs currently operate in eleven states across the United States (National Center for START Services, University of New Hampshire Institute on Disability, 2023). All START programs have an interdisciplinary Clinical Team that includes professionals with expertise in IDD-MH. Key principles of the START model include development of an integrated understanding of the individual and their needs through careful assessment, cross-system collaboration, and outreach to all the systems serving the individual, crisis prevention and intervention, and medical/psychiatric consultation services. A study examining outcomes of the START program found a 1-year pre-post improvement in caregiver service experiences and mental health symptoms of the service user, as well as a significant decrease in psychiatric hospitalizations and emergency department visits.
Another example of a child and adolescent mental health intellectual disability service is the Mental Health in Learning Disabilities (CAMHS) Team at the Maudsley Hospital in London, UK (Chilvers et al., 2013). This consultation service provides assessment and recommendations regarding diagnosis, medication, neuropsychological functioning, behavior management, educational placements, and risk assessment, as well as specialist treatment of mental health or behavior difficulties to children and adolescents with IDD-MH. An evaluation of this program in 2013 indicated both high levels of client satisfaction as well as fulfillment of criteria outlined for a “model service” such as inclusion of the family, consideration of cultural and social factors, individualized treatment planning, use of home and school visits, family support, and effective liaison with other services.
A final example of a comprehensive, integrated treatment program for adolescents with complex developmental and mental health needs is the CARTS program (Comprehensive Assessment and Response Training System) in Illinois (Naylor et al., 2003). While the CARTS program targets wards of the Illinois Department of Children and Family Services (DCFS) with severe emotional disturbance rather than those with IDD, the complexity of these children (which often includes IDD-MH) warrants examination of this program. Like the programs previously described, the CARTS program utilizes a multidisciplinary assessment system that evaluates not only the adolescent, but also the living environment (usually group home or residential placement) to identify treatment interventions that can stabilize and meet the needs of the adolescent in their current placement. A key part of the CARTS program is support of transition of the adolescent from the CARTS inpatient assessment unit back to the community. This is accomplished through Response Training System (RTS) consultants who train and work with adults in the adolescent’s home environment to incorporate successful interventions. The CARTS program has been found to be effective in stabilizing placements and reducing utilization of psychiatric hospital resources in this population.
Experts agree that key elements of care for the IDD-MH population, as illustrated in the examples above, include “treatments that cross traditional bureaucracies of care and integrate disparate intervention modalities (including positive behavior supports, pharmacotherapy, appropriately modified psychotherapy, and trauma-informed care)” (Constantino et al., 2020, p. 10). Such treatments are best developed within the context of an interdisciplinary team, in partnership with the individual and family, to transcend the barriers created by silos of developmental and mental health services (Davis et al., 2008; Pinals et al., 2022; Son et al., 2019). Ideally, this type of care occurs in the community, using the child’s natural supports, to prevent the need for placement in more restrictive settings. The current paper presents one such model of an innovative, interdisciplinary, intensive consultation team that uses best practice principles to overcome barriers and improve outcomes for IDD-MH youth. As will be shown, the model has the potential to preserve family relationships, keep individuals with IDD-MH in their home communities, and allow them to pursue an inclusive and meaningful life.
Background Information
Over recent years, the state of Nevada has experienced an alarming trend of placing children and adolescents with behavioral health disabilities in long-term, out-of-state, residential psychiatric treatment centers. As a result of this troubling trend, which separates youth from their families, isolates them from their communities, and frequently creates iatrogenic trauma, the U.S. D.O.J. opened an investigation that in 2022 resulted in the finding that
…there is reasonable cause to believe that the State of Nevada violates Title II of the Americans with Disabilities Act (ADA), by failing to provide services to children with behavioral health disabilities in the most integrated settings appropriate to their needs. (U.S. D.O.J., 2022)
Because of the lack of community interventions and support for Nevadan youth with IDD-MH, these children have been most at risk for experiencing the consequences of this failure.
The Intensive Consultation Team (ICT) was born out of a desire to reverse the trend of out-of-state residential psychiatric placement for youth with IDD-MH in Nevada. The goal of ICT is to provide interdisciplinary, expert consultation to systems serving individuals with IDD-MH (such as families, schools, and outpatient providers) to stabilize youth in their home communities and prevent institutionalization. In reviewing the existing models described above, ICT drew particularly from the CARTS program, as this program identifies an explicit goal of stabilizing youth in community settings and reducing residential psychiatric placements. Like the CARTS model, ICT uses an interdisciplinary approach to perform extensive assessment, with particular attention to the interaction between individual and environmental factors that may contribute to the individual’s emotional and/or behavioral instability. Also, like CARTS, ICT provides extensive behavioral intervention support to the key environments surrounding the individual. Unlike the CARTS model (and more like the START and CAMHS models), ICT does not utilize an inpatient hospital unit for initial assessment but seeks to provide assessment and consultation while the youth is still living at home. ICT shares similarities with all three models—CARTS, START, and CAMHS–in that an integrated, person- and family-centered understanding of the individual is developed through careful interdisciplinary assessment, interventions are designed to meet the needs and preferences of the individual and family, and cross-system collaboration is prioritized.
Methods
The ICT is an interdisciplinary team model that consists of doctoral- and master’s-level practitioners who provide coordinated assessment and treatment across a variety of domains, including psychiatry, behavioral intervention, mental health therapy, special education, and intensive care coordination. The project is a collaboration between a University Center for Excellence in Developmental Disabilities (UCEDD), a Leadership Education in Neuro-developmental and Related Disabilities (LEND) program, and several state and community partners, including the Division of Child and Family Services and the Aging and Disability Services Division within the state. The goal of the program is to provide youth with IDD-MH, specifically those who have not had their needs met by prior community interventions, an opportunity to receive intensive interdisciplinary outpatient treatment in their home communities instead of being placed in residential treatment (usually out-of-state). Services are delivered in an intensive but short-term format (approximately 6 months) with the intention of engaging the natural supports of the individual from the start and transitioning the full breadth of care back to a treatment team in the community following the intensive interdisciplinary assessment and treatment.
The eligibility criteria for ICT are youth (ages 6-18 years old) with a diagnosed intellectual or developmental disability and a co-occurring mental health diagnosis. Youth need to have behavioral concerns that put them at risk for disruption of their current placement or have previously been in an out-of-home placement and are transitioning back to their home community. Youth are also required to have the support of a community-based interdisciplinary or interagency team who can provide ongoing support once ICT services are completed. At the time of intake, youth who need acute crisis intervention are not eligible, as ICT is not designed to provide immediate crisis response.
The intake process for youth begins upon referral form completion. Primary sources of referrals are from the collaborating state agencies of this project, local human services agencies, or local juvenile justice services agencies. The youth are screened for eligibility and those who meet criteria advance to a process of parental consent, release of information, and initial conversation regarding treatment goals. All historical records for the youth are collected, including but not limited to any formal behavioral assessments, psychiatric assessments, neuropsychological testing, mental health diagnoses, mental health treatment plans, individualized education plans (IEPs), inpatient case notes, and/or psychological assessments. Once all records are collected, the case coordinator and project director review the records to determine if the youth is to be triaged to the Level 2 or Level 3 team based on history of past intervention, current needs, and level of risk for being removed from their home. Upon being established with a clinical team, the records are extensively reviewed by all team members prior to engaging with the youth or family.
ICT has two distinct levels of support ranging from comprehensive behavioral intervention with interdisciplinary consultation (Level 2) to full interdisciplinary team-based intervention (Level 3). Table 1 depicts the three levels of supports relevant to ICT. The two levels of support are offered to meet the ranging needs of the referrals received while conserving resources, as in many cases the individuals had not previously received any behavioral interventions. A Level 1 designation is not a service offered within the ICT model as existing community-based supports, services, and interventions are considered Level 1 within the model. At both Levels 2 and 3 of service within the ICT, each youth has a team formed around them that includes the individual with IDD themselves, relevant family members or guardians, school providers, mental health providers, social services representatives, any other case management coordinators involved, and designated members of the ICT team. The team engages in a model of person-centered planning in which the individual’s strengths and hopes are placed at the forefront of each planning session and the individual with IDD participates in the creation and approval of all aspects of their assessment, treatment planning, and selected supports.
| Level of support | Team composition and services offered |
|---|---|
| Level 3 | ICT services include multidisciplinary planning including psychiatric, educational, and behavior assessment and intervention. |
| Level 2 | ICT services include comprehensive behavior support planning and intervention with consultation as needed from other disciplines. |
| Level 1 | Referrals to community-based behavioral and mental health support services, social services, and/or wrap-around services. |
Individuals who receive interventions at Level 2 work with a master’s-level Licensed and Board-Certified Behavior Analyst (BCBA) and a master’s-level case coordinator. Following an intake process, complete with historical records review, the team meets to determine the priorities and goals of the individual with IDD. The individual is asked to share their desires and the parents/guardians are also asked to express their hopes for the child. A 4-week assessment phase is enacted after the team meeting and includes an environmental and functional behavior assessment (FBA) using direct observation in home, direct observation in the school, and indirect methodologies including the Functional Assessment Screening Tool-Revised (FAST-R), and the Questions About Behavior Function (QABF). Quality of life and caregiver strain measures are also administered to the parents/caregivers of each youth. A second team meeting is conducted after the assessment phase to review the results of the assessment and to discuss the plan, including getting input from the individual with IDD and the parents/caregivers. Once the plan is agreed upon, intervention begins, which lasts 8-12 weeks. The interventions are individualized based on the needs of the youth. Whereas some receive direct service intervention in a clinic-style setting, others receive in-home consultation only. In all cases, parents and caregivers receive training on the plan with the BCBA and data are collected and reviewed throughout. If needed, consultation from other disciplines (such as psychiatry or special education) from the Level 3 team helps to provide input on issues such as education plans or medication treatment. At the completion of intervention, a third team meeting is held to review progress and discuss a plan for transition back to community-based support.
Individuals who are referred and triaged to the interdisciplinary team (Level 3) receive the same support as individuals at Level 2. However, the team also includes a Board-Certified Child and Adolescent Psychiatrist, a doctoral-level special educator, and a licensed Marriage and Family Therapist (MFT). A doctoral-level BCBA (or BCBA-D) also participates in place of the master’s-level BCBA on the Tier 3 cases. Each participating member of the interdisciplinary team conducts their own individual assessments, resulting in an FBA, a psychiatric evaluation, educational evaluation, and mental health assessment. The FBA is the same as described above but conducted by a professional with advanced training and interdisciplinary knowledge. The psychiatric assessment includes a full review of pre-existing records, diagnostic interview with both client and parent, and mental status examination. This results in a diagnosis and recommended treatment plan, which could include individual or family therapy; allied health treatments such as occupational, physical, or speech and language therapy; educational interventions; and/or pharmacological treatment. Mental health assessment includes current psychosocial stressors and supports, evaluation of the family system, presence or absence of coping resources, and response to previous psychotherapeutic treatments. The educational assessment includes a review of academic progress, successes, barriers, educational diagnoses, educational placement, and IEP status to evaluate the efficacy of the client’s current educational environment.
Prior to implementation of the Level 3 plan, the interdisciplinary team meets to integrate their findings and treatment recommendations into one comprehensive assessment. A comprehensive, coordinated intervention plan consisting of recommendations for behavioral treatment, educational interventions, mental health supports for the youth and caregivers, and (if appropriate) medication management, is assembled by the ICT case coordinator. Consistent with teaming at Level 2, the integrated treatment plan is presented to the youth and family during the second team meeting to allow for discussion and feedback on the course of treatment, including placing the preferences of the youth at the forefront. During the discussion with the family and youth, a finalized intervention plan is designed, and interventions are provided over 8-12 weeks, with some youth receiving interventions in the clinic and others receiving interventions in the home. If treatment revisions are warranted mid-intervention, an additional team meeting is held. At the completion of the intervention phase, the team meets with the family and client to review progress, make final recommendations, and plan for transition of the youth back to community-based supports. Table 2 depicts the phases of the ICT model.
| Phase | Activity |
|---|---|
| Intake (4 weeks) |
|
| Assessment (4 weeks) |
|
| Intervention (8-12 weeks) |
|
| Transition (2 weeks) |
|
| Closure (1 week) |
|
In addition to the structure of the community-based team meetings, the internal clinicians from the ICT meet weekly to review the progress and outcomes of each case. During the internal meetings, team members provide status updates, discuss progress toward goals, review records and data, and make interdisciplinary decisions. This internal, ongoing collaboration amongst a team of interdisciplinary professionals is one of the key contributors to the success of this model as it allows ample time for each discipline to share their perspective on the case and talk freely to align thinking, perspective, and support ideas prior to presenting the interdisciplinary treatment approach to the individual, caregivers, and broader team. A person-centered case study with aligned assessment results and treatment recommendations is shared below to further enhance understanding of the provision of an interdisciplinary model of care, while also considering the preferences of the individual and their family members.
Case Example
At the time of intake, Eric was a 15-year-old male who had been previously diagnosed with a learning disability, autism spectrum disorder, attention deficit hyperactivity disorder (ADHD), disruptive mood dysregulation disorder, oppositional defiant disorder, and generalized anxiety disorder. He was referred to the ICT by his county probation office in hopes of reducing aggressive behavior in the home and community settings and increasing his ability to engage in prosocial skills, allowing him to participate meaningfully in his home and school environments. In the referral documentation, the officer expressed concerns about Eric’s behavior, especially his tendency to be aggressive, both verbally and physically, with his mother. Additionally, the officer indicated that Eric was struggling at school and had been expelled from his high school for fighting shortly before the ICT referral was submitted.
ICT assessments were conducted simultaneously by the team’s doctoral-level clinicians, which included a psychiatrist, behavior analyst, and special educator. In conducting the assessments at the same time, and meeting together weekly to compare notes and discuss findings, the three professionals were able to develop a comprehensive assessment profile that resulted in an interdisciplinary treatment plan. During the first interview with Eric and his mom, conducted by the behavior analyst and psychiatrist together, the team discovered that Eric presented many strengths, including the fact that when he was in a relaxed, familiar environment with trusted adults and peers, he was engaging, funny, and curious. He had the capacity to be persistent and put forth significant effort when working on preferred tasks. He was particularly interested in getting a job and expressed a desire to become a barber after completing high school. Eric mostly enjoyed spending time alone in his room, using his cell phone, and playing video games. He also reported a desire to spend more time with his family, many of whom lived in a different state. Eric enjoyed eating Mexican food and shopping for shoes. Eric’s personal goals included successfully completing probation, getting a job, and saving money to buy himself things he wanted.
Historical records were reviewed by all team members and indicated that Eric had difficulties with frequent illnesses as a child, and experienced separation anxiety when he first attended kindergarten. During his elementary school years, he exhibited learning challenges and was first placed on an IEP in 2016, when he was found eligible for special education services under the category of Specific Learning Disability. Eric’s mother was unable to pinpoint exactly when Eric developed emotional and behavioral symptoms; however, reports indicate that a psychiatrist first evaluated him at age 9, suggests that his emotional and behavioral challenges likely started around that time. Since early adolescence, Eric had displayed increasing problems with intense, aggressive anger outbursts, low frustration tolerance, moodiness and irritability, boredom, and school failure. At the time of the ICT’s initial assessment, the school district had just decided to place Eric in a self-contained school for students with severe emotional and behavioral health issues.
The psychiatric assessment determined that Eric met criteria for a Major Depressive Episode, as he had persistently irritable mood with superimposed explosive anger episodes, anhedonia and boredom, guilt, poor energy, poor concentration, and intermittent passive suicidal ideation in response to stress. Significant stressors contributing to his depression included social isolation, removal to a restrictive school setting, the move of close family members to another state, and ongoing conflict with his mother, who was his primary support. He also met criteria for Disruptive Mood Dysregulation Disorder, which pre-dated the development of his depressive symptoms. Records also strongly supported previous diagnoses of ADHD, Specific Learning Disorder with an Impairment in Reading, and Borderline Intellectual Functioning (with a Full-Scale IQ of 73). Eric had been diagnosed with Autism Spectrum Disorder by two previous psychologists; however, as he lacked perseverative interests and stereotyped behaviors, and as he demonstrated many strengths not usually seen in autism (such as empathy, perspective-taking, and reciprocity), the psychiatrist concluded that both assessments likely incorrectly labelled him with autism as they occurred over a short period of time in office settings where he tended to shut down and become uncooperative. Finally, the psychiatrist strongly suspected an underlying anxiety disorder and/or post-traumatic stress disorder (PTSD) due to classic symptoms of need for repeated reassurance, frequent gastrointestinal symptoms, hypervigilance, and misperceptions that people were out to get him following exposure to several possible trauma-inducing events.
In addition to the psychiatric diagnostic assessment, Eric received a functional behavior assessment, an environmental assessment, and an educational assessment. The functional behavior assessment indicated that Eric’s verbal and physical aggression belonged to the same response class, meaning they occurred together and for the same function, and were multiply maintained by access to attention, access to preferred items/activities, and escape from non-preferred tasks/activities. Conditions under which aggression was most likely to occur and conditions under which aggression was least likely to occur were identified as well as precursory behaviors. The environmental assessment indicated that the school environment was very chaotic and triggered his behaviors, while at the same time his mother used punishment and criticism to manage his behaviors at home, with Eric ultimately receiving little positive social attention in either the home or school environments. The educational assessment indicated that Eric had academic deficits and would benefit from a comprehensive speech-language evaluation to determine the appropriate learning supports for his abilities.
During early assessments of his challenges by both the behavior analyst and the psychiatrist, Eric reported that he did not “need any help.” Therefore, much of his history of challenging behaviors was reported by Eric’s mother, who said that he was almost always irritable, angry, and verbally and physically aggressive. She said, “He’s always threatening me” and calling her profane names. Triggers for his agitated behavior included not being able to go to activities with friends and not being able to have what he wants. His mother reported that, “one minute he’s fine, and the next he’s flipping out.” He could attack his mother to the point that she needed to restrain him for her own safety or call the police. If she tried to ignore his behavior, it angered him more and he would physically attack her further. Even when not agitated, Eric seemed unhappy. He complained frequently of being “bored.” When his mother was at work, Eric would call her repeatedly to ask what time she would be coming home. Eric engaged in negative self-talk about himself, slept most of the day, and had poor concentration. He did at times say that he wanted to kill himself when angry but had not made any suicide attempts nor did he engage in self-harm.
Per the ICT model, the first team meeting was held to identify Eric’s goals and strengths and he was able to share his desires for his treatment, although at the time, given his experience with mental health treatment, he was mostly resistant to more professionals working with him. His broader team included Eric, his mother, his uncle, the ICT members, his case worker from the Aging and Disability Services Division, his probation officer, his assigned wraparound caseworker from Division of Child and Family Services, and his school counselor and school psychologist. By the end of the first meeting, Eric was able to understand the ICT process, and he expressed a willingness to try something different for a short while. He identified his personal goals as desiring to have a relationship with his family (mom), to learn the necessary skills to get a job, and to work towards getting off probation. Based on previous negative experiences with both psychiatric medication and talk therapy, Eric was very adamant that he did not want either intervention, and only agreed to participate in ICT if these wishes were respected. Eric’s mother was also committed to working with the team. Her desires for his treatment included having Eric attend school without a fight, gain control over his anger, and reduce incidents of aggression towards her.
Based on the above findings, and in consideration of Eric’s strengths and preferences, an interdisciplinary treatment plan was created. The second team meeting was held to review the assessment findings and propose treatment recommendations for revisions and approval by Eric and his family. Eric was present and attentive during the entire meeting but minimally participated. While the team felt that individual psychotherapy and medication management would have been helpful to directly target Eric’s Major Depression and ADHD symptoms, they honored his choice and “met him where he was at” by focusing on interventions targeting his and his mother’s specific goals. Eric’s mother agreed to a support plan with the following terms: (1) she would bring Eric to the ICT for twice-weekly social skills intervention, an intervention that he agreed to try; (2) she would receive 1:1 coaching support to improve her relationship with her son; (3) she would engage in daily positive activities with her son; and (4) she would collect daily data for team-based decision making. Upon discussing returning to school with an adequate behavior support plan, Eric became visibly upset and announced that he would prefer to do school online, something the team was willing to consider. An emergency crisis plan with de-escalation strategies was also developed and agreed to for consistency in responding to aggressive behavior.
Interventions were designed with Eric’s preferences, goals, and strengths in mind as well as his cognitive and psychological needs that were identified in the psychiatric and behavioral assessments. Baseline data were collected in July and intervention began in August. Prevention consisted of indirect intervention with Eric by working exclusively with his mother on increasing her positive engagements and positive activities with him. These two interventions were selected specifically based on Eric’s trauma history and PTSD responses, with the intention of building in some additional protective factors in the prevention of triggering trauma response. Having a more positive environment at home, fewer punitive or corrective interactions, and rebuilding a healthy relationship with mom were identified as key areas of focus for mental health prevention. His mother received weekly coaching sessions with the ICT team to work on her own behavior in interacting with Eric, including how to recognize appropriate behavior, use praise, and respond to challenges. She collected daily data on positive interactions and his engagement in leisure activities. During this time, home environment expectations were created and attempted; however, Eric was unwilling to participate in any type of home expectations, even when offered incentives or identified reinforcers to participate. To honor his preferences, this intervention was removed.
Teaching interventions were designed with Eric’s strengths of humor and 1:1 preferred adult engagement and adapted to meet his educational and cognitive needs. Eric participated in once to twice weekly social skills lessons that were implemented with a Registered Behavior Technician (RBT) from the ICT. An evidence-based curriculum, Skillstreaming, was selected for its use of role play and instructions were modified slightly to provide mostly verbal or visual cues during intervention as opposed to the use of any written worksheet formats. In line with Eric’s goals to close his probation case, the probation officer supported the use of this intervention by agreeing to give Eric community service credit hours towards his probation plan for participating in these sessions.
The final intervention that was put into place was a shift from attending in-person school to online school. Eric had been attending school within the most restrictive school district placement for youth with mental health diagnoses—a self-contained program located on its own campus. Eric became very dysregulated in this environment, as many fights broke out on campus on a regular basis, there was a very punitive behavioral points system in place, and there was a lack of mutual respect between Eric and the administration of the school. The team, in consideration of Eric’s preferences, did not make the decision to recommend this change in his educational placement lightly—three separate team meetings with school staff, observation of the school environment, and behavioral data demonstrating correlation of irritability and aggression with school attendance made it clear that the high level of chaos within that environment triggered his PTSD symptoms and made it impossible for him to learn. More importantly, Eric himself vehemently requested that he be withdrawn from the school environment that he found aversive. After working closely with the school and providing a formal written recommendation from our team’s psychiatrist, Eric was offered an opportunity to participate in a home-hospital placement for education that allowed him to make academic progress in the environment where he felt safe.
Data was collected by Eric’s mother daily using an online submission form. Data were graphed and reported to the team weekly for review. School data was not provided on a consistent basis, so all data aggregated for decision making came from the home. Anecdotal reports from the school were considered as part of the broader picture of Eric’s well-being. Data on Eric’s verbal and physical aggression and mom’s self-reflection of positive interactions are discussed below.
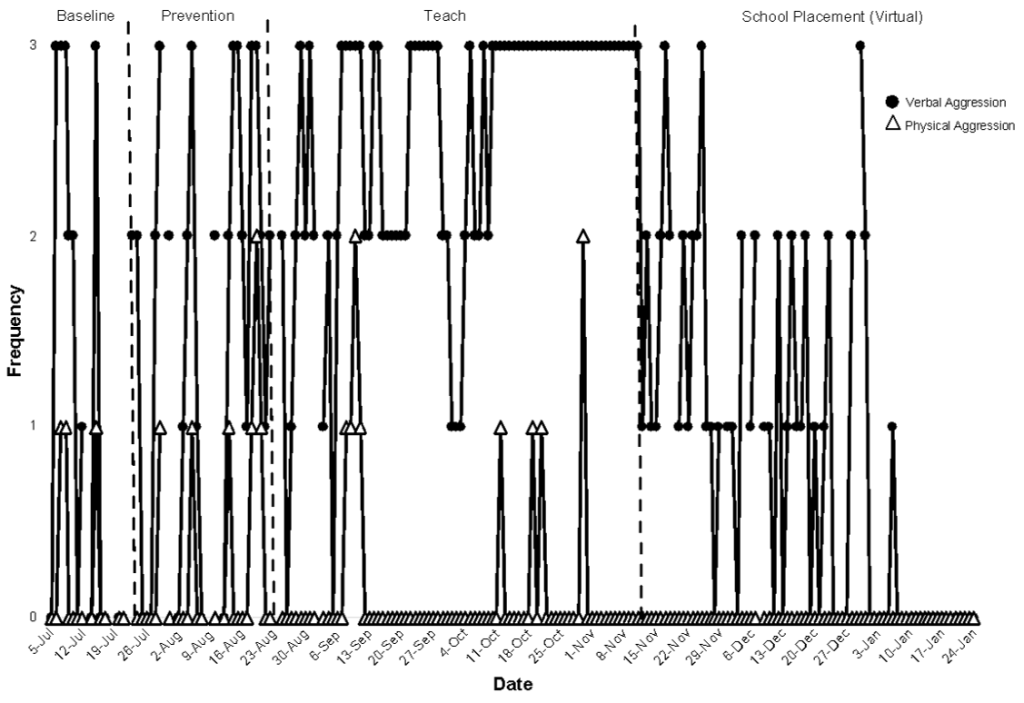
Verbal aggression was defined as Eric cursing, screaming, or making threats toward his mother. Physical aggression was defined as hitting, kicking, punching, grabbing, or pulling hair (primarily directed towards mom). Instances of physical aggression would often result in the police being called to intervene. Data presented in Figure 1 show an improvement in verbal aggression and a decrease to zero levels of physical aggression over the course of intervention. During the baseline condition, verbal aggression occurred multiple times per week and sometimes even multiple times per day, while physical aggression occurred about once per week. During the prevention intervention phase, the team did not observe significant changes in verbal or physical aggression, indicating that prevention efforts were not an effective intervention for Eric’s aggressive behaviors. During the teaching intervention, an increase in verbal aggression was observed; however, a decrease in physical aggression was also observed. It is assumed that as Eric learned more strategies to manage conflict and anger during the teaching interventions, his need to use physical aggression lessened, while verbal aggression remained high. Given the topography and severity of physical aggression as compared to verbal aggression, this observed change in behavior was seen as a very beneficial outcome. The increase in verbal aggression was also attributed to the increased stress and frustration that Eric was simultaneously experiencing at school. At the point in which the team, including Eric, decided to try online learning, an immediate decrease in verbal aggression was observed and physical aggression remained at zero rates following the teaching intervention phase and the move to online learning. As social skills instruction continued, coupled with online schooling, both verbal and physical aggression were reduced to zero rates and maintained as such for over a month.
Note. Baseline, prevention, teach, and online school placement interventions are separated by the dashed vertical lines.
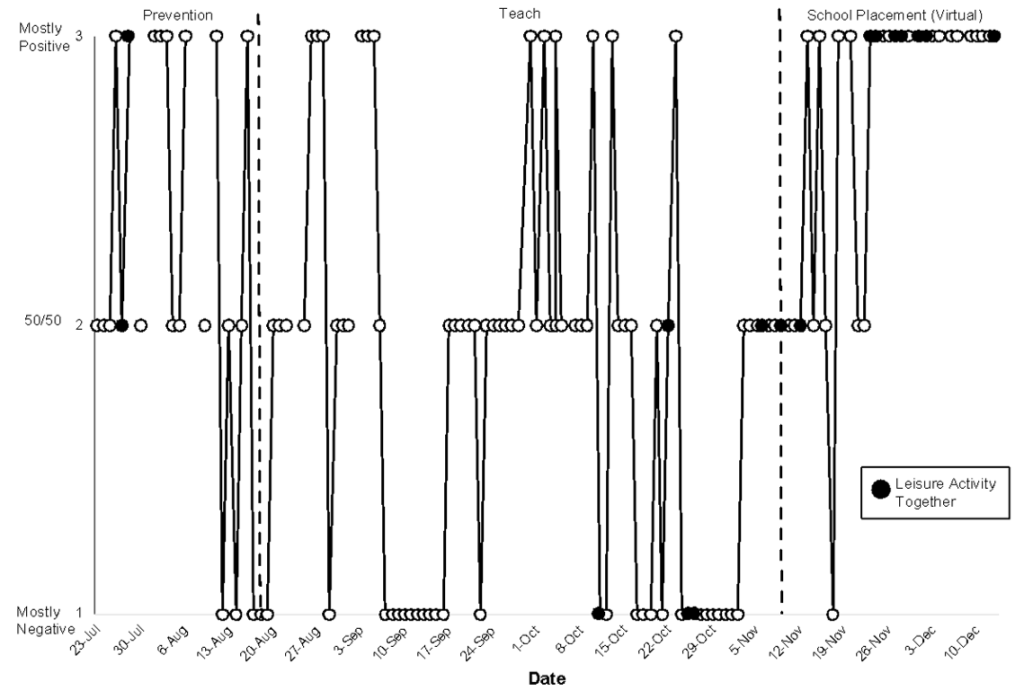
Positive interactions between Eric and his mom were coached and monitored to enhance the relationship between Eric and his mom and to provide Eric with more positive than negative feedback. These data for the intervention are relevant as close relationships and positive interactions are both trauma-informed protective factors for mental health. Positive interactions were defined as mom’s use of praise or pleasant statements directed towards Eric. Data on positive interactions are presented in Figure 2 and the phase changes are mapped onto the phase changes for the interventions that Eric was receiving. These data do not include a baseline component; however, positive interactions demonstrate an increasing trend over time during both the teaching phases for Eric’s behavior and the school placement phase. Data indicates that at the beginning of the intervention, there may have been a focus or strong emphasis on positive interactions, likely due to the novel instruction and support being provided. However, as the intervention continued, Eric’s mother may have defaulted to more negative interactions, which was typical within the history of their relationship. Weekly coaching sessions on engaging in positively stated phrases, praise, and recognizing appropriate behavior provided additional ideas for pleasant interaction opportunities. Data indicates that by the end of the intervention, Eric’s mother was consistently reporting that she engaged in mostly positive interactions with Eric throughout the day. Anecdotally, she also had shared that as his behavior towards her improved, she found it easier to engage with him in a positive manner. Data were also collected on leisure activity engagement between Eric and his mother, another trauma-informed protective factor that the team wanted to establish as a mental health prevention intervention. The two were able to engage in more leisure activities together, as indicated also in Figure 2. Ability to engage in leisure activities appears to be correlated with days that Eric’s mother reported she was able to engage in mostly positive interactions. It should also be noted that Behavioral Activation, characterized by increasing amounts and frequency of pleasurable activity, is an evidence-based treatment for Major Depression; so, though Eric was not participating in formal mental health treatment for his depression, the family work with his mother incorporated elements of mental health treatment that undoubtedly contributed to Eric’s mood improvement.
Note. Prevention, teach, and online school placement interventions are separated by the dashed vertical lines.
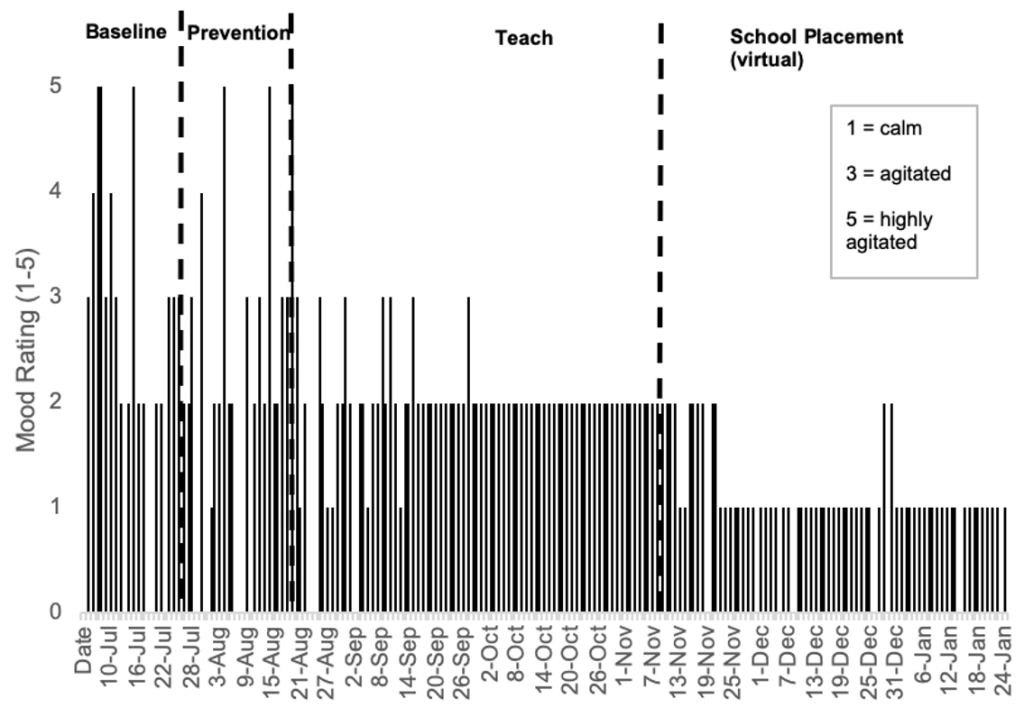
Data was also collected on Eric’s daily mood. While Eric was unwilling to collect his own self-monitoring data, his mother provided a self-report of his general mood stability during each day. Mood data were collected on a 5-point scale with a rating of 1 suggesting a calm mood, 2 suggesting minor agitation, 3 suggesting agitation, 4 suggesting moderate agitation, and a 5 suggesting high levels of agitation throughout the day. Data suggest that Eric displayed minor to high levels of agitation during all days of the baseline phase (see Figure 3). During the prevention phase, the same trends in agitation were observed except for 1 day where Eric was reported to be calm. During the teaching phase of the intervention, Eric’s agitation levels began to decrease, and more calm days were observed, and agitation levels never rose above a rating of 3. Towards the end of the teaching intervention, and when online school was introduced, Eric’s agitation levels remained low, with most days reported as calm and few days reported as mild agitation. In addition, data were collected on Eric’s nightly sleep throughout the baseline and intervention conditions. Eric slept approximately 8 hours per night with little variability. Because of the consistency in his sleep pattern and adequate duration of sleep, it was concluded that Eric’s sleep was not a factor in his mood or behavior.
Note. Baseline, prevention, teach, and online school placement interventions are separated by the dashed vertical lines.
After 6 months in services with ICT, the broader team met for a final time to review the progress Eric had made and created plans for transition of his treatment back to the natural community support. According to Eric’s identified treatment goals and preferences, he was ready to successfully discharge from probation. With ICT’s support, he had secured a job in the community and was engaging successfully in online school from his home. Eric’s mother’s goals of reduced aggression and increased engagement with school had also been met. The interdisciplinary treatment modality was significantly more successful compared to numerous previously attempted interventions, and Eric was no longer at risk of being removed from his home community to residential treatment. Many of the stressors that had contributed to Eric’s Major Depression had lessened or resolved. His experience of learning practical social skills was much more enjoyable to him than his previous experience of being “talked at” during traditional psychotherapy. Additionally, he had developed positive relationships with multiple members of ICT, which allowed them to talk with him about the pros and cons of medication treatment and provide psychoeducation regarding risks and benefits. During his transition meeting, Eric was encouraged to keep an open mind about medication in the future should his symptoms of depression become worse.
When Eric was asked about his satisfaction with the services he received, he shared that he really enjoyed the social skills classes and had come to look forward to them each week. He was also very relieved to finally be off probation because of his participation in ICT and was happy to have his first real job. He remained adamant that he did not want to return to school and preferred his home-hospital placement with online learning. He reported a better relationship with his mom and said he enjoyed going out into the community with her and that they were also getting along better at home. Eric’s mother felt similarly; she and Eric had a better relationship, and they were communicating better because of the skills that she and Eric had learned. Eric’s mother was thrilled to report that she had not been physically assaulted by Eric in many months and that she was not having to call emergency services for support anymore. The mental health of both mom and Eric had improved because of a calmer home environment and receiving the appropriate support that matched his unique needs.
At a 6-week follow-up, Eric had lost his first job because of a poor fit but had found another job that felt more comfortable for him and his interests. His mother reported that Eric’s verbal and physical aggression within the home remained extremely low and that they were enjoying many new activities together including cooking dinner and watching movies. Approximately 1 year after delivery of services, Eric’s mother reached out to ICT members and shared that Eric was on track to graduate from high school within the year and that he had decided that he would like to try psychotropic medications. While Eric was no longer in the care of the ICT, a referral to a community-based clinician was made with a “warm hand-off” and a personal introduction to the new psychiatrist by ICT members.
Discussion
As described throughout this paper, the use of interdisciplinary teams has become increasingly popular in various fields and is, perhaps, most prevalent in healthcare settings. Research indicates that interdisciplinary teams often result in myriad benefits, including enhanced problem-solving, innovation, and holistic approaches to complex problems, making the interdisciplinary approach particularly powerful when attempting to address the complex needs faced by youth and families affected by IDD-MH (Dinh et al., 2020). However, interdisciplinary teams are not without their challenges, and successful deployment of such teams requires considerable initial investment in the development of the team’s infrastructure, especially the thoughtful design of leadership and communication models. Failure to adequately plan can result in team malfunctions that hinder effectiveness. ICT personnel spent 3 years working through many challenges to reach the point of effective interdisciplinary teaming. The discussion below outlines many of the “lessons learned” by ICT, which will be beneficial to readers wishing to implement similar interdisciplinary practices.
Team Membership
The most successful interdisciplinary teams are composed of people who can simultaneously represent their individual discipline while remaining open to diverse perspectives and solutions (Brown et al., 2023). Because individual member flexibility is paramount to overall team effectiveness, newly forming interdisciplinary teams would be wise to invite members who readily demonstrate the capacity to navigate the myriad ambiguities associated with interdisciplinary care. Although professional credentials are important, ICT learned that interpersonal effectiveness is far more critical to overall team wellbeing and functionality. If a newly forming team is unable to identify a specifically credentialed professional who also demonstrates the interpersonal qualities necessary for interdisciplinary work, ICT recommends that the team refrain from involving someone simply because they possess the correct credential; instead, consider using the person in a consultative role until a more appropriate permanent team member can be found.
Leadership, Expectations, and Communication
ICT decided to forego the traditional hierarchical forms of leadership and, instead, embraced a culture of shared leadership. Leadership was shared equally among team members regardless of credential, allowing each individual team member to contribute his/her own unique talents to the betterment of ICT. Such a diffuse leadership model requires a significant level of trust among team members. ICT cultivated such trust by developing communication, decision making, conflict resolution practices, and team expectations prior to serving any families. All team members committed to abiding by the expectations, which were codified in an ICT policy and procedure manual. The manual served as a guidepost and was repeatedly used to re-orient team members to the group’s original vision and intentions during times of disagreement.
Despite the commitment to shared leadership, ICT members acknowledged that someone needed to be responsible for ensuring the daily functioning of the team. As a result, one of the first decisions made by ICT was to create a team coordinator position. The ICT Coordinator functioned as the team hub, responsible for organizing team efforts, ensuring accurate and timely communication, liaising with the family, facilitating team meetings, and assisting team members in the completion of team-related tasks. ICT learned that, in addition to being highly organized, a successful coordinator needed to be flexible, possess excellent communication skills, provide exceptional customer service, be adept at conflict resolution, and have a solid understanding of local resources. ICT decided to select someone with a social work/case management background to fill this role.
In addition, ICT designed an intentional communication plan, which required that ICT members commit to consulting with others before making any decisions that might impact the trajectory of the case. Decisions were usually made during weekly case conference meetings; however, the fluid nature of the challenges faced by ICT families often required that team members be available outside of traditional work hours to consult with their fellow team members. Decisions made outside of the traditional case conference setting involved the entire core intervention team and were immediately communicated to the remaining team members and documented in the case file.
In the rare moments when team members failed to abide by the communication commitment, the team functionality suffered. Immediately following each instance of communication failure, ICT members engaged in a post-mortem analysis of the situation and developed plans for avoiding similar future failures. These critical conversations were difficult; however, team cohesion survived the conflict because ICT members were able to employ the pre-established team conflict resolution expectations. Every successful conflict resolution experience served to further the sense of trust among ICT members.
Commitment to Person-Centered Care
ICT remained steadfast in its commitment to placing the youth and the family/caregiver at the center of all ICT services and activities. Youth and family priorities were used to establish all behavior goals and intervention recommendations. The priorities were revisited at every team meeting and services and interventions were amended as appropriate. Additionally, youth and family were given equal voice with the professionals at the decision-making table. For example, in the case described above, Eric’s preferences regarding treatment choice (he was willing to engage in practical, skills-based coaching sessions, but not traditional “talk therapy” or medications) and school placement (he preferred online schooling to his district school placement) were prioritized over professional recommendations. This person-centered treatment planning approach likely contributed significantly to the success of Eric’s ICT experience, as it valued his wisdom about what would work for him and engaged him in a way that previous treatment attempts had not. The experience also reduced his distrust of providers and opened up more willingness for him to consider future mental health treatment.
ICT learned that the commitment to person-centered care did not always align with the priorities of other stakeholder agencies/community partners. To circumvent potential team conflict about intervention goals, ICT required that team consensus about goals be achieved at the first team meeting. Publication of the primary goals of each youth and family at the top of each meeting agenda assisted in keeping team members focused on person-centered outcomes. Additionally, data related to the primary goals were then reported at each subsequent meeting.
Family Commitment to Change
The families served by ICT were profoundly affected by their experiences of trying to access services for their loved one in a fractured system of youth behavioral healthcare. All the families reported significant levels of trauma for both individual family members and the family system. Most of the families had been contending with their challenges for years and were exhausted by their efforts and the lack of systemic support. The exhaustion and trauma rendered many of the caregivers somewhat ambivalent about their capacity to continue to provide in-home care for their child. ICT learned quickly that helping caregivers move through their ambivalence and toward willingness for change was vital to the success of their loved one. This level of readiness is needed to include all caregivers in the home, not just primary caregivers. One of ICT’s earliest cases involved a family with numerous extended family member caregivers. ICT considered only the primary caregiver’s readiness for change and failed to understand the influence that the extended family members had on the primary caregiver’s ability to engage in the intervention process. This failure to address the extended family’s readiness resulted in the primary caregiver eventually acquiescing to family pressure and surrendering her custodial rights.
As previously mentioned, ICT centered all intervention goals on the priorities of the youth and the family. Additionally, youth and family were given equal access to the decision-making process. These two approaches alone served to increase youth and family willingness to engage with ICT. ICT also considered the influence of factors such as family ethnicity and culture, socioeconomic status, trauma history, and past mental health treatment experiences when developing treatment recommendations. Finally, ICT relied heavily on providing caregiver education and support to increase caregiver capacity to use appropriate in-home positive behavior interventions.
Behavior Analysis and Mental Health
One of the most influential and effective components of ICT was the collaboration between board-certified behavior analysts and traditional mental health practitioners. A prominent schism has long existed between behavior analysis, with its emphasis on observable behavior and empirical data, and traditional mental health interventions, which tend to focus inwardly on thoughts and emotions. ICT decided to challenge the notion that behavior analysis and psychotherapy are incompatible by including both behavior analysts and mental health therapists on ICT. From the combination of these diverse perspectives emerged powerful and effective interventions. ICT’s behavior analysts developed robust positive behavior support plans that addressed, through practical means, the challenging behavior that was putting each youth’s current placement at risk for disruption. The behavior analysts also provided caregiver training and education services that increased caregiver capacity to effectively intervene with their loved one, thereby decreasing caregiver stress. At the same time, the mental health practitioners defined the influence of other issues, especially trauma, on the family system and individual family members. This allowed ICT to craft trauma-informed interventions and recommendations that fully honored the family’s experiences. The therapist also provided opportunities for the youth and caregivers to process their own thoughts, feelings, and experiences throughout the program. Finally, the ICT psychiatrist was available to provide medication management when needed, while at the same time utilizing all the behavior data regarding environmental context to avoid misguided biological intervention (medication) if an environmental intervention was more appropriate. Such a holistic provision of services is rarely offered to families, especially those affected by IDD-MH. ICT provided the inclusive and interdisciplinary approach necessary to create the comprehensive toolkit required to meet the complex and varied needs of families affected by IDD-MH.
Overall Program Outcomes
Outcomes associated with ICT demonstrate the capacity of interdisciplinary care to substantially enhance the quality of life of youth affected by IDD-MH. Between April 2020 and October 2023, ICT provided care for 24 youth and their families. Of those youth and families, 17 (71%) successfully completed ICT services, as defined by meeting or exceeding the intervention goals established by the team at the beginning of care. Of the remaining seven youth and families, three (12.5%) experienced the need for higher levels of care and were transitioned to appropriate providers, two (8%) were closed because of an unanticipated out-of-state foster placement, one (4%) eloped from her placement, and one (4%) family decided that they were unable to make the accommodations in their schedules necessary to engage with ICT.
References
Bougeard, C., Picarel-Blanchot, F., Schmid, R., Campbell, R., & Buitelaar, J. (2021). Prevalence of autism spectrum disorder and co-morbidities in children and adolescents: A systematic literature review. Front Psychiatry, 12, 744-709. https://doi.org/10.3389/fpsyt.2021.744709
Brown, S. A., Sparapani, R., Osinkski, K., Zhang, J., Blessing, J., Cheng, R., Hamid, A., Begheri MohamadiPour, M., Castrillon Lal, J., Kothari, A. N., Caraballo, P., Noseworthy, P., Johnson, R. H., Hansen, K., Sun, L. Y., Crotty, B., Chung Cheng, Y., Echefu, G., Doshi, K., & Olson, J. (2023). Team principles for successful interdisciplinary research teams. American Heart Journal Plus: Cardiology Research and Practice, 32, 1-7. https://doi.org/10.1016/j.ahjo.2023.100306
Chilvers, R., Gratton, S., & Bernard, S. H. (2013). Satisfaction with a child and adolescent mental health services (CAMHS) intellectual disability service. Advances in Mental Health and Intellectual Disabilities, 7(1), 49–58. https://doi.org/10.1108/20441281311294701
Clark, L. L., Lekkai, F., Murphy, A., Perrino, L., Bapir‐Tardy, S., & Barley, E. A. (2020). The use of positive behaviour support plans in mental health inpatient care: A mixed methods study. Journal of Psychiatric and Mental Health Nursing, 27(2), 140–150. https://doi.org/10.1111/jpm.12566
Constantino, J. N., Strom, S., Bunis, M., Nadler, C., Rodgers, T., LePage, J., Cahalan, C., Stockreef, A., Evans, L., Jones, R., & Wilson, A. (2020). Toward actionable practice parameters for “dual diagnosis”: Principles of assessment and management for co-occurring psychiatric and intellectual/ developmental disability. Current Psychiatry Reports, 22(9), 1-13. https://doi.org/10.1007/ s11920-020-1127-8
Davis, E., Barnhill, L. J., & Saeed, S. A. (2008). Treatment models for treating patients with combined mental illness and developmental disability. Psychiatry Quarterly, 79, 205-223. https://doi.org/ 10.1007/s11126-008-9082-2
Dinh, J. V., Traylor, A. M., Kilcullen, M. P., Perez, J. A., Schweissing, E. J., Venkatesh, A., & Salas, E. (2020). Cross-disciplinary care: A systematic review on teamwork processes in healthcare. Small Group Research, 51(1), 125-166. https://doi.org/10.1177/1046496419872002
Gathright, M. M., Holmes, K. J., Morris, E. M., & Gatlin, D. (2016). An innovative, interdisciplinary model of care for inpatient child psychiatry: An overview. The Journal of Behavioral Health Services & Research, 43(4), 648-660. https://doi.org/10.1007/s11414-015-9484-5
Gentile, J. P. & Gillig, P. M. (2012). Psychiatry of intellectual disability a practical manual. Wiley-Blackwell.
Harvey, M. T., Luiselli, J. K., & Wong, S. E. (2009). Application of applied behavior analysis to mental health issues. Psychological Services, 6(3), 212–222. https://doi.org/10.1037/a0016495
Holingue, C., Kalb, L. G., Klein, A., & Beasley, J. B. (2020). Experiences with the mental health service system of family caregivers of individuals with an intellectual/developmental disability referred to START. Intellectual and Developmental Disabilities, 58(5), 379–392. https://doi.org/10.1352/ 1934-9556-58.5.379
Kalb, L. G., Beasley, J., Caoili, A., & Klein, A. (2019). Improvement in mental health outcomes and caregiver service experiences associated with the START Program. American Journal on Intellectual and Developmental Disabilities, 124(1), 25–34. https://doi.org/10.1352/1944-7558-124.1.25
Khachadourian, V., Mahjani, B., Sandin, S., Kolevzon, A., Buxbaum, J. D., Reichenberg, A., & Janecka, M. (2023). Comorbidities in autism spectrum disorder and their etiologies. Translational Psychiatry, 13(1), 71–71. https://doi.org/10.1038/s41398-023-02374-w
Matson, J. L. & Nebel-Schwalm, M. S. (2007). Comorbid psychopathology with autism spectrum disorder in children: An overview. Research in Developmental Disabilities, 28(4), 341–352. https://doi.org/ 10.1016/j.ridd.2005.12.004
McDougle, C., Scahill, L., Aman, M. G., McCracken, J. T., Tierney, E., Davies, M., Arnold, L. E., Posey, D. J., Martin, A., Ghuman, J. K., Shah, B., Chuang, S. Z., Swiezy, N. B., Gonzalez, N. M., Hollway, J., Koenig, K., McGough, J. J., Ritz, L., & Vitiello, B. (2005). Risperidone for the core symptom domains of autism: Results from the study by the autism network of the research units on pediatric psychopharmacology. The American Journal of Psychiatry, 162(6), 1142–1148. https://doi.org/ 10.1176/appi.ajp.162.6.1142
Morris, N., & Zisman-Ilani, Y. (2022). Communication over incarceration: Improving care coordination between correctional and community mental health services. Psychiatric Services 73(12), 1409-1411. https://doi.org/10.1176/appi. ps.202200041
Munir, J. M. (2017). Diagnosing co-occurring mental disorders in children and adolescents with intellectual disability/intellectual developmental disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 56(10), S148–S148. https://doi.org/10.1016/j.jaac.2017.07.560
National Center for START Services, University of New Hampshire Institute on Disability (2023). Integrated mental health treatment guidelines for prescribers in intellectual and developmental disabilities. https://centerforstartservices.org/IDD-MH-Prescribing-Guidelines
Naylor, M. W., Anderson, T. R., & Morris, A. (2003). Child psychiatry and child welfare: A collaboration for change. Residential Treatment for Children & Youth, 21(1), 33–50. https://doi.org/10.1300/J007 v21n01_03
Ozonoff, S., Rogers, S. J., & Hendren, R. L. (2003). Autism spectrum disorders: A research review for practitioners (1st ed.). American Psychiatric Pub.
Pinals, D. A., Hovermale, L., Mauch, D., & Anacker, L. (2022). Persons with intellectual and developmental disabilities in the mental health system: Part 2. Policy and systems considerations. Psychiatric Services, 73(3), 321-8. https://doi.org/10.1176/appi.ps.201900505
Romani, P. W., Banks, T., Barnes, J. C., Murphy, J., Sannar, E. M., & Anderson T. (2021). Use of a short-term psychiatric inpatient model to address problem behavior exhibited by youth with intellectual or developmental disabilities. Evidence-based Practice in Child and Adolescent Mental Health, 6(4), 447-458. https://doi.org/10.1080/23794925.2021.1975517
Simonoff, E., Pickles, A., Charman, T., Chandler, S., Loucas, T., & Baird, G. (2008). Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry, 47(8), 921–929. https://doi.org/10.1097/CHI.0b013e318179964f
Singh, N. N. (Ed.). (2016). Handbook of evidence-based practices in intellectual and developmental disabilities. Springer International Publishing. https://doi.org/10.1007/978-3-319-26583-4
Son, J., Debono, D., Leitner, R., Lenroot, R., & Johnson, J. (2019). Pass the parcel: Service provider views on bridging gaps for youth with dual diagnosis of intellectual disability and mental health disorders in regional areas. Journal of Paediatrics and Child Health, 55, 666-672. https://doi.org/10.1111/ jpc.14266
Summers, J., Busch, L., Kako, M., & Lau, C. (2022). The role of the behavior analyst on interprofessional mental health teams: opportunities for collaboration and enhancing patient care. Journal of Interprofessional Care, 36(3), 434–440. https://doi.org/10.1080/13561820.2021.1969345
U.S. Department of Justice, Civil Rights Division. (2022). Investigation of Nevada’s use of institutions to serve children with behavioral health disabilities. https://www.justice.gov/usdoj-media/crt/ media/1249631/dl?inline
West, L., Waldrop, J., & Brunssen, S. (2009). Pharmacologic treatment for the core deficits and associated symptoms of autism in children. Journal of Pediatric Health Care, 23(2), 75–89. https://doi.org/ 10.1016/j.pedhc.2008.12.001
Whittle, E., L., Fisher, K. R., Reppermund, S., Lenroot, R., & Trollor, J. (2018). Barriers and enablers to accessing mental health services for people with intellectual disability: A scoping review. Journal of Mental Health Research in Intellectual Disabilities, 11(1), 69–102. https://doi.org/10.1080/ 19315864.2017.1408724

