7 Parents of Children with Disabilities in the Early Months of COVID-19: Knowledge, Beliefs and Needs
Mary Beth Bruder PhD; Tara M. Lutz PhD; and Kelly E. Ferreira PhD
Bruder, M. B., Lutz, T. M., & Ferreira, K. E. (2020). Parents of Children with Disabilities in the Early Months of COVID-19: Knowledge, Beliefs and Needs. Developmental Disabilities Network Journal, 1(2), 21. https://doi.org/10.26077/E7D4-7C9B
Plain Language Summary
Families have many needs as a result of COVID-19. We wanted to find out about the needs of families with children with disabilities. We did a national survey and 457 families completed it. The families reported a decrease in the amount of services and supports they were receiving because of COVID-19. They reported being most concerned about their child’s education and health. Most families reported high anxiety.
COVID-19 pandemic is unprecedented, and the effects will be long lasting. Many have speculated as to the impact the illness, social isolation, and absence of community will have on all of society (Coyne et al., 2020; Galea et al., 2020), including those with disabilities (Aishworiya & Kang, 2020; Alexander et al., 2020; Boyle et al., 2020; Leocani et al., 2020; Sabatello et al., 2020). Compared to the general population, children, youth, and adults with disabilities have historically experienced disparities in access and participation in health care, inclusive schools and classrooms, postsecondary education and work training, community living options and autonomy, decision, making and self-determination (Wehmeyer et al., 2017). The pandemic has exacerbated these disparities (Ervin & Hobson-Garcia, 2020; Lund et al., 2020; Thompson & Nygren, 2020), creating the need to examine and reform the systems, practices and policies that were in place prior to the pandemic (Bradley, 2020).
COVID-19 has also negatively affected families as documented by studies conducted during the first few months of the pandemic (Coller & Webber, 2020). Parents have reported increased caregiver burden and subsequent stress as they tried to balance working from home while caring for children and supporting their learning needs when schools closed (Cluver et al., 2020; Weaver & Swank, 2020). These conditions resulted in increases in mental health needs, such as depression and anxiety as reported by families across a number of studies (Gassman-Pines et al., 2020; Patrick et al., 2020; Russell et al., 2020). These needs were exacerbated by worry about health, job loss, health insurance loss and food insecurity (Coller & Webber, 2020).
These stressors are increased for families of children with disabilities, many of whom have special health care needs. These conditions contribute to an increased stress burden for families, which has been recognized long before this current pandemic (Aldersey et al., 2017; Barroso et al., 2018; Hayes & Watson, 2013; Vanegas & Abdelrahim, 2016). This burden has been shown to increase a family’s anxiety and decrease their quality of life over the lifespan of the child (Williamson & Perkins, 2014; Woodman et al., 2015).
The severity and contagiousness of the COVID-19 virus has created more anxiety for these families, as youth with intellectual and developmental disabilities (IDD) experience fatalities from COVID-19 at a higher rate than those without IDD—1.6% compared to less than 0.1% for those without IDD ages 0-17 (Turk et al., 2020). Adding to this anxiety are the losses that many families are experiencing because of the pandemic. These include loss of work, income, food security, and access to community resources, each of which can threaten their sense of well-being (Brown et al., 2020; Prime et al., 2020). These threats add to the already high stress burden experienced by families with children with disabilities (Fontanesi et al., 2020).
Two studies have assessed the well-being of families of children with disabilities during the COVID-19 pandemic. Willner et al. (2020) focused on primary caregivers (mostly families) of children and adults with intellectual disabilities (ID) and families with children without ID living in Great Britain. The caregivers were recruited through email requests to disability organizations. Once the caregiver was determined to meet the inclusion criteria for the study, they were asked to complete several measures through the internet. These included a demographic questionnaire about their child and themselves and formal measures of coping strategies, social supports, anxiety, depression, and defeat and entrapment.
The group of participants included in the study consisted of caregivers of 107 adults over the age of 18 with ID, 100 caregivers of children under the age of 18 with ID, and 37 caregivers of children under 18 who did not have ID. Findings suggested that the caregivers of children and adults with ID had significantly higher levels of defeat and entrapment. Almost half (43%) reported moderate to severe levels of anxiety compared to 8% of caregivers of children without ID. Similarly, 45% of the caregivers of children with ID reported moderate to severe levels of depression compared to 11% of caregivers of children without ID. The caregivers of children with ID also received significantly less social support than caregivers of children without ID. Further, these caregivers received significantly more support from professionals and significantly less support from family members and friends than caregivers of children without ID.
Another study on the effects of COVID-19 on families of children with disabilities was conducted by Neece et al. (2020). Seventy-seven parents of young children with disabilities ages 2-5, including autism, were recruited from an ongoing intervention study and asked to participate in a telephone interview. The parents were ethnically, linguistically, and socioeconomically diverse and resided in California and Oregon. The interview consisted of five questions that assessed the challenges of COVID-19, the impact of COVID-19 on their child’s services, benefits because of COVID-19, their coping strategies, and the anticipated long-term impact of COVID-19 on their family.
The interviews were recorded and transcribed, and the responses to the questions were themed across the families. The biggest challenge from the pandemic reported by the families was being at home and unable to leave the house, followed by balancing work and caring for young children, and the lack of childcare. Most parents said that their child’s services had decreased, though a majority reported benefits of the pandemic such as spending more time as family. Parents identified economic concerns as the long-term impact of COVID-19. The concerns included employment, finances, and the emotional toll the pandemic was taking on themselves and their children.
The purpose of the present study was to document the effects of the COVID-19 pandemic on families of children with disabilities across the U.S. As the sample was national, the population base from which information was gathered was more relevant to the U.S. than the Willner et al. (2020) study, and broader in geographic scope than the Neece et al. (2020) study. This study was also part of a larger effort by the Department of Public Health Sciences at a School of Medicine in the Northeast to document the knowledge, beliefs, and behaviors of specific audiences at the inception of the pandemic.
Method
Participants
A modified snowball sampling (Morgan, 2008) method was used to recruit the participants for this survey. Electronic invitations to participate in an online survey about the effects of COVID-19 on their family’s life was sent to parents of children with disabilities using state and national list serves, national disability organizations, and social media. The invitation provided a brief description of the nature of the study and details including the fact that participation was voluntary. The invitation also contained a link to the survey instrument. The email invitation gave permission to those who received it to share with others who may be interested and eligible to participate. The survey was open from April 2, 2020, until June 1, 2020.
Inclusion criteria for the survey analysis was being a parent of a child with a disability who qualified for and was receiving early intervention or special education as stated in the demographic section of the survey. The final sample consisted of 457 parents who self-identified as having at least one child with a disability from 47 U.S. states and territories.
Most of the sample (n = 335, 73%) indicated that they had a child receiving special education services through an IEP, with 38 (8%) reporting that they had a child who was receiving early intervention services, and 84 (18%) reporting that they had children in both early intervention and special education (with an IEP). The average age of the parent who completed the survey was 42.5 years old (SD = 8.7), with the average age of the child with a disability just under 11 years of age (M = 10.9, SD = 5.3). The sample was primarily White (69%), female (79%), and married or living with partner (68%). More than half the sample (56%) reported being employed either part-time or full-time, and 58% indicated they had completed a 4-year college degree. These data are presented in Table 1.
| Variable | n | % |
|---|---|---|
| Gender (n = 382) | ||
| Male | 15 | 3.3 |
| Female | 362 | 79.2 |
| Gender non-conforming | 1 | 0.2 |
| Prefer not to respond | 4 | 0.9 |
| Race/Ethnicity (n = 382) | ||
| African American | 17 | 3.7 |
| Black | 9 | 2.0 |
| LatinX/Hispanic | 31 | 6.8 |
| White | 313 | 68.5 |
| Indian | 1 | 0.2 |
| Asian/Pacific Islander | 14 | 3.1 |
| Native American/Indigenous | 9 | 2.0 |
| Other | 5 | 1.1 |
| Prefer not to answer | 9 | 2.0 |
| Marital status (n = 381) | ||
| Single | 32 | 7.0 |
| Married or living with partner | 309 | 67.6 |
| Divorced/separated | 32 | 7.0 |
| Widowed | 8 | 1.8 |
| Highest educational level (n = 380) | ||
| Less than high school | 1 | 0.2 |
| High school diploma/GED | 29 | 6.3 |
| Some college | 57 | 12.5 |
| 2-year college degree | 27 | 5.9 |
| 4-year college degree | 128 | 28.0 |
| Master’s degree | 102 | 22.3 |
| Professional degree (e.g., JD, MD, PhD) | 36 | 7.9 |
| Employment (n = 380) | ||
| Unemployed | 14 | 3.1 |
| >Employed part-time | 70 | 15.3 |
| Employed full-time | 187 | 40.9 |
| Laid off because of coronavirus (COVID-19) | 31 | 6.8 |
| Retired | 5 | 1.1 |
| Student | 4 | 0.9 |
| Stay-at-home parent | 69 | 15.1 |
| Number of children receiving early intervention services (n = 122) | ||
| 1 | 109 | 23.9 |
| 2 | 12 | 2.6 |
| 3 | 0 | 0.0 |
| 4 | 1 | 0.2 |
| Number of children receiving special education services through an IEP (n = 419) | ||
| 1 | 340 | 74.4 |
| 2 | 63 | 13.8 |
| 3 | 15 | 3.3 |
| 4 | 1 | 0.2 |
Survey
The survey instrument was an adaptation of a survey designed and distributed to multiple target audiences by during the first months of the pandemic. The original survey was designed to measure knowledge, attitudes, and resulting behavior changes in target populations in response to COVID-19. The adaptation was designed by the University Center for Excellence in Developmental Disabilities (UCEDD) that is affiliated with the same School of Medicine where the original survey originated. The adapted survey instrument differed from the original survey in two ways: (1) the addition of questions specific to for families with children with disabilities, and (2) the recruitment of a national audience as the sample.
The survey instrument consisted of 36 closed-ended and 1 open-ended question. The adapted instrument used in this study collected additional data specific to families with children with disabilities. In addition to demographic information, the survey included questions about (a) formal and informal supports before and during COVID-19, (b) sources of information about COVID-19, (c) knowledge about COVID-19, (d) behavioral changes due to COVID-19, (e) issues faced because of COVID-19, (f) current family needs, (g) beliefs about COVID-19, and (h) anxiety related to COVID-19. The instrument utilized skip logic to display questions based on a participant’s previous responses. The instrument was estimated to take up to 15 minutes to complete.
Procedure
The web-based survey was administered through Qualtrics, a third-party online survey company. After receiving IRB approval, recruitment of families of children with disabilities occurred from the beginning of April 2020 through the beginning of June 2020 (2-month period). An online invitation was distributed that contained a link to the Qualtrics survey.
The first page of the survey was an information sheet that provided information about the purpose of the study, study procedures, potential risks, benefits, protection and rights of the participant if they chose to complete the survey, contact information regarding study content, and how to contact the PI of the survey. Respondents were given the option to “accept” or “decline” participation before completing the survey, and this served as the consent to participate.
Once the survey was complete, the family member clicked “submit” and the survey was submitted through Qualtrics to the study team.
Analysis
All data that were collected through Qualtrics were downloaded into both Excel and SPSS version 25 (IBM Corp, 2017) to be cleaned for analysis. Data cleaning for the analysis reported herein involved the removal of surveys from parents who (a) did not report having a child in the home, and (b) did not report having a child who was receiving either early intervention services or special education through an IEP. Families who reported their child as having a special health care need and/or a diagnosed disability but did not report the child receiving services through early intervention or an IEP, were also removed from this analysis. Descriptive statistics, including frequencies, means, and standard deviations, were used to analyze the data from this survey. Qualitative responses from the open-ended item were thematically coded and reported in the results as quantitative data.
Results
Information Sources about COVID-19
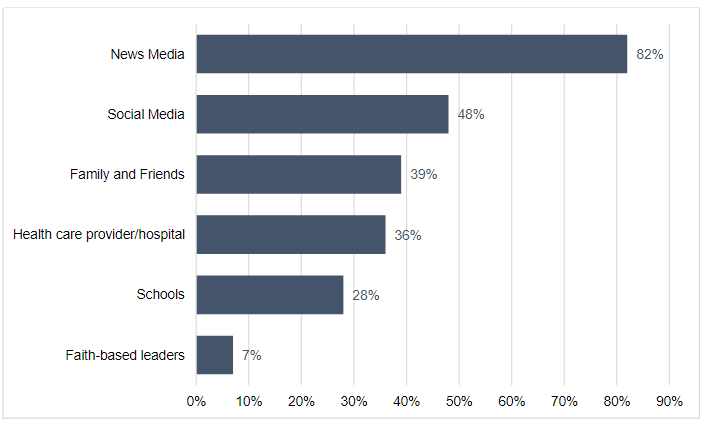
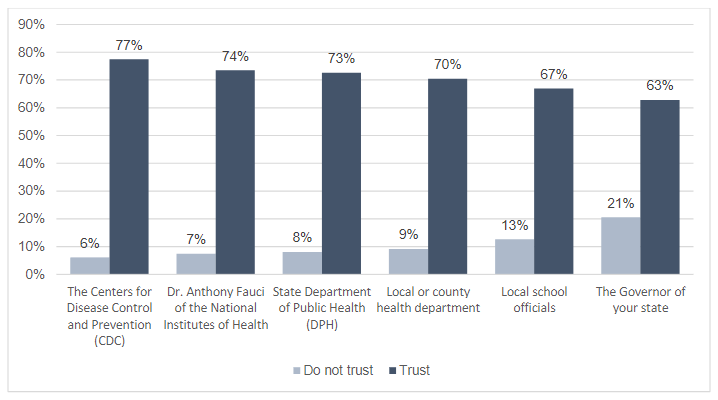
The most frequently reported sources of information about COVID-19 were news media (82%), which included television and newspapers, followed by social media (47%), such as Facebook, Twitter, and Instagram. The least frequently reported sources included schools (28%) and faith-based leaders (7%) (see Figure 1). The average number of sources of information used was 4.3 (SD = 2.2). Respondents were also asked how much they trusted their sources of information (see Figure 2). Respondents reported high levels of trust in both scientific informants and their governments, with most families trusting the Centers for Disease Control and Prevention (CDC; 77%), Dr. Anthony Fauci (74%), and their state department of public health (73%).
Knowledge about COVID-19
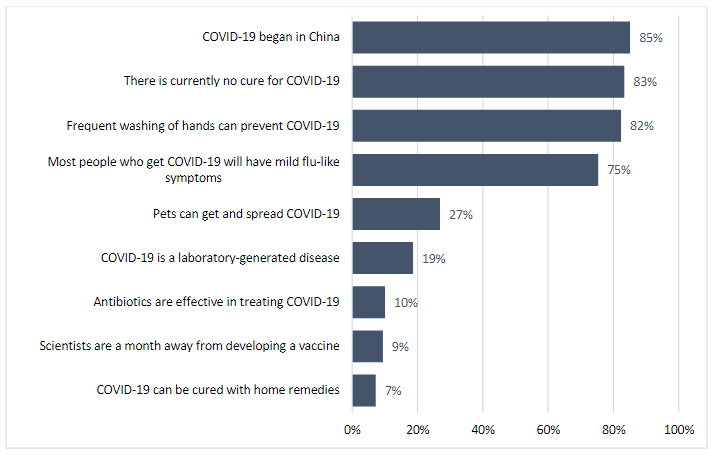
Respondents were asked about their knowledge of COVID-19, including where the virus began, how the virus is transmitted, and how it could be prevented. Most of the sample answered correctly for each knowledge item (see Figure 3 for percent of respondents who said the statement was true/correct on each item). Respondents were also asked about their knowledge of COVID-19 symptoms. Most families (86%) reported that fever was one of the earliest symptoms, followed by a dry cough (80%), shortness of breath (71%), fatigue (63%), and body aches (52%).
Behaviors as a Result of COVID-19
When asked to report changes made to reduce the chances that they (respondent) and their child would get COVID-19, the most frequently reported changes were: (a) stay home as much as possible (87%), (b) wash hands frequently (86%), and (c) avoid physical contact (85%). Among the least frequently reported changes were to wear a mask when going out (63%) and wear sanitary gloves when outside the home (30%) (Table 2). The average number of changes made by respondents was 10.3.
| Changes made by families | n | % |
|---|---|---|
| Stay home as much as possible | 397 | 86.9 |
| Wash hands frequently | 394 | 86.2 |
| Avoid physical contact with people (e.g., no hugs and handshaking) | 388 | 84.9 |
| Avoid sick people | 371 | 81.2 |
| Keep physical distance between people | 369 | 86.7 |
| Do not gather with more than 5 people | 369 | 80.7 |
| Cough and sneeze into the crook of my elbow | 353 | 77.2 |
| Avoid public transportation | 338 | 74.0 |
| Clean frequently touched surfaces with products such as sanitizers that have at least 60% alcohol by volume (120 proof) | 337 | 73.7 |
| Avoid touching my face (eyes, nose, mouth, ears) | 330 | 72.2 |
| Wear a mask when going out | 288 | 63.0 |
| Wear sanitary gloves when out of the home | 139 | 30.4 |
Respondents were also asked what they would do if they thought that they or their child had symptoms of COVID-19. Most of the sample (87%) reported that they would monitor their symptoms and seek care if necessary (e.g., call their health care provider, stay at home to rest, monitor symptoms, stay in touch with their primary care provider, and seek a COVID-19 test). Most respondents (86%) also reported that they would engage in quarantining/social distancing measures and quarantine from other family members and visitors, minimize contact from the rest of the family, and receive no visitors. Additional measures respondents reported were cleaning or increased hygienic practices (82%), such as washing their hands frequently, cleaning all high-touch surfaces, and not sharing dishes, utensils, towels.
Access to Formal and Informal Support as a Result of COVID-19
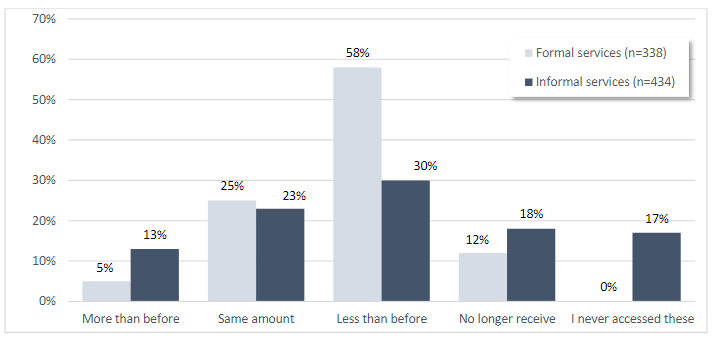
Results indicated that most respondents (78%) received formal supports such as a service coordinator, case manager or care coordinator, health services, early intervention, or special education prior to COVID-19 pandemic. When asked if they were receiving these services after the pandemic began, almost two thirds of the sample (60%) reported they were receiving less than before the pandemic or not receiving them at all. Respondents were also asked if prior to the pandemic they used informal supports such as disability support groups, family support groups, faith-based groups, social media groups, friends, and neighbors. Most (75%) indicated accessing informal supports before the pandemic, and almost half (48%) indicated they accessed less or no informal supports after the pandemic began (Figure 4).
Concerns as a Result of COVID-19
Participants were asked to respond to a list of concerns and identify which, if any, they were experiencing because of COVID-19 (see Table 3). They reported concerns about the physical health (74%), mental health (75%), well-being (80%), and safety (68%) of family members. Participants also reported concerns about their own physical health (59%), mental health (61%), well-being (63%), and safety (37%). A quarter (26%) reported concerns about the loss of a job while 39% reported concerns about the loss of income. Delays in education for their children were reported by 71% of respondents, and 77% reported concerns with changes in special education services. A quarter (23%) had concerns about meals (lack of) because of the move to online/remote learning. This move also concerned 25% of respondents because of a lack of access to technology (i.e., devices and internet/Wi-Fi). Another 38% reported concerns about using technology for virtual meetings, school, and work. Almost half of families reported boredom (46%) and loneliness (43%). Only 5% reported issues accessing transportation (as most reported staying at home).
| Concerns of families | n | % |
|---|---|---|
| Concern about the well-being of family members | 364 | 79.6 |
| Changes in education going online affecting services (special education) | 352 | 77.0 |
| Concern about the mental health of family members | 344 | 75.3 |
| Concern about the physical health of family members | 338 | 74.0 |
| Delays in educational services | 326 | 71.3 |
| Not able to visit or support older relatives and friends | 325 | 71.1 |
| Concern about the safety of family members | 310 | 67.8 |
| Concern about my own well-being | 289 | 63.2 |
| Concern about my own mental health | 278 | 60.8 |
| Concern about my own physical health | 269 | 58.9 |
| Concern about accessing the health care system | 257 | 56.2 |
| Boredom | 208 | 45.5 |
| Loneliness | 197 | 43.1 |
| No one to take care of children | 184 | 40.3 |
| Loss of income | 180 | 39.4 |
| Concern related to using technology (virtual meetings, school, work, etc.) | 173 | 37.9 |
| Concern about my own safety | 168 | 36.8 |
| Unable to get enough food, medications, and supplies in the home | 145 | 31.7 |
| Loss of job | 117 | 25.6 |
| Concern related to accessing technology (devices, internet) | 116 | 25.4 |
| Changes in education going online affecting services (meals) | 105 | 23.0 |
| Access to transportation | 24 | 5.3 |
Needs as a Result of COVID-19
Respondents were asked to report two current needs of their family. A total of 388 respondents (85%) entered needs, with 355 listing two separate needs, resulting in 743 separate needs being reported. Using thematic analysis (Gavin, 2008), needs were coded into eight main categories. The most reported needs were educational (38%), followed by family support (16%) and financial (15%) needs. Additional needs were health and safety (7%), respite (5%), stability (4%), medical (3%), and access to information and resources (2%). The other category (10%) included responses such as “N/A,” “I don’t know,” and various other responses such as sleep and patience (see Figure 5).
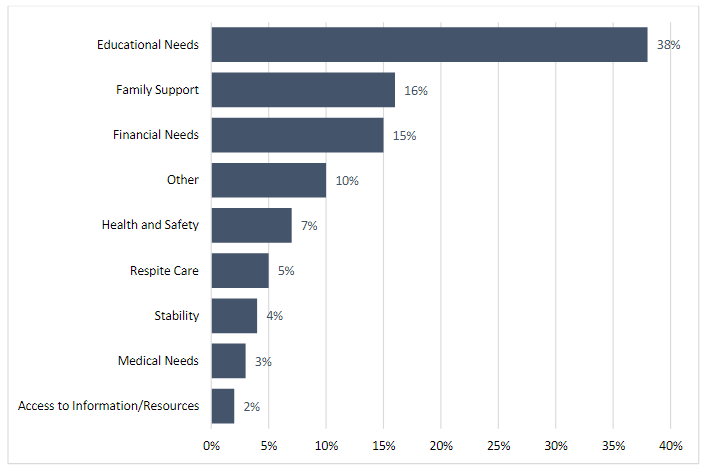
The category of educational need for their child included three sub themes: (1) therapeutic services and support, (2) educational services and support, and (3) special education services and support. Therapeutic services and support, which comprised 40% of this category, included needs such “mental health services;” “physical therapy, occupational therapy, and speech-language services;” and “crisis support.” Educational services and support (37% of the category) included items such as “academic assistance/support,” “access to learning tools,” “educational instruction,” “assistance with online/home schooling.” Last, 23% of respondents reported needs for special education services and supports, such as “IEP supports at home,” “developing an IFSP,” “get special education services,” “in-home support to implement special education services through virtual resources,” and “access to special education services.”
The category of family support was comprised of four subcategories. The most reported need was social support (41%), followed by childcare (22%), general support (20%), and child activities (17%). Examples of social support needs included “social interaction opportunities,” “lunch with friends,” “getting back into the community,” and “daily social interaction with non-family members.” Examples of childcare included “childcare supervision,” “support for kids so I can work,” “daycare,” and “childcare for children with complex health needs.” Reported needs surrounding general support included “support,” “consistency in support,” and “continued support.” Last, examples of child engagement include “activities for my special needs child,” “engaging activities for child to understand the current situation,” and “ways to fight boredom.”
Beliefs about the Effects of COVID-19
Respondents were asked how serious COVID-19 was for different population groups. The majority (98%) indicated the virus was somewhat or very serious for the U.S. and for their state or territory (97%). Eighty-seven percent indicated the virus was somewhat or very serious for their family.
Respondents were also asked how long they thought the COVID-19 crisis would continue, and whether they thought that life would go back to the way it was before COVID-19. Approximately 22% reported that they thought the crisis would last until the end of the school year, 31% reported that they thought it would continue through the beginning of the next school year (fall 2020), and 33% reported that they believed the crisis would last longer. The majority (74%) of families reported that they did not think that life would go back to the way it was before the pandemic. More specifically, when asked what they thought would change, 59% of the families reported that they expected closer connections within families, 53% reported increased community or neighborhood support, and 44% reported an increased sense of social connectedness. Regarding schools and special services, 40% of the families reported expecting permanent changes in schools for children ages 5-21, 38% reported expecting changes in special services, 23% reported expecting changes in early intervention services and preschool special education, and 36% reported expecting changes in higher education.
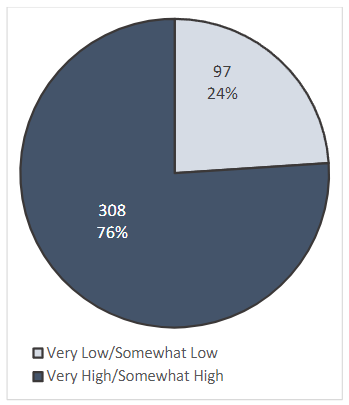
Anxiety as a Result of COVID-19
Respondents were asked to indicate their current anxiety level from very low to very high. Of those who responded to this question, most families (76%) reported their current anxiety as somewhat or very high, as presented in Figure 6.
Discussion
The purpose of this study was to describe the knowledge, beliefs, and needs of parents of children with disabilities during the beginning months of COVID-19. The participants in the study responded to online invitations from multiple solicitations and invitations to parents of children with disabilities, thus prohibiting the calculation of a response rate. The respondents were also skewed to those who have access to the internet and had the skills to complete the online questionnaire. As a result, the sample who completed the survey were homogeneous: highly educated, employed, the majority reported their race/ethnicity as White, their sex as female, and their role as a parent with a child with disabilities.
It is no surprise that the parent respondents to this survey reported getting their information from credible sources such as news media and having a high trust in government sources of information. Of those who reported their education level (83% of the sample), 18% reported having at least some college or a 2-year degree, 28% had a bachelor’s degree, and 30% reported having graduate degrees. The parents also demonstrated correct knowledge of COVID-19 and its symptoms and were accurate in changes they should make in response to the virus. Using a mask was one of the lowest ranked behaviors at 63%, but it should be noted that this survey was conducted before the recommendations for wearing a mask was widespread. The parents also responded accurately about what they would do if they or their child contracted the virus. Last, the parents described accurate beliefs about COVID-19, as almost 100% described it as being serious for the U.S. Only 33% projected that the pandemic would last beyond September 2020, which was not accurate, but reflects the thinking at the time of the survey.
Parent respondents reported a marked decrease in the amount of formal support and informal services they were receiving because of the pandemic. This is reflected in the many concerns they identified in the survey. Their primary concern was the well-being of their family members (80%), including their mental and physical well-being (75% and 74%, respectively). Concern for their own well-being, both physical and mental, and safety of their family followed as concerns for most parent respondents. Also of concern was education, with 77% of parents identifying it as a concern, followed by delays in education (71%).
The current needs identified by parents also followed this pattern. Over 85% of parents identified two separate current needs. Qualitative theming of all needs resulted in the most reported need of parents being educational services and supports for their children followed by family support. Educational needs included special education, therapeutic education (e.g., therapies), and general educational needs.
Children with disabilities receive education through early intervention (usually delivered in the home) or special education (usually delivered in public schools). These options changed when the U.S. shut down home visits and schools during the spring of 2020 to stop the spread of the virus. Families with children who could no longer attend school or have a home visitor were thrust into the role of special educator (Hughes & Anderson, 2020). Those who had access to technology were able to participate in some type of online/remote learning, though for fewer hours than their child had been in school. In addition to losing the individualized and specialized supports and services provided by early intervention and special education, online/remote learning also eliminated access to peers without disabilities in an environment to learn and socialize together (Leocani et al., 2020). As a result, it has been suggested that students with disabilities have lost critical educational time (e.g., Masonbrink & Hurley, 2020; Neece et al., 2020), as documented by the Tulsa Seed Study (2020). The data collected in this study indicated that parents of children with special needs were more likely to report challenges with distance learning compared to parents of children without special needs. The findings were consistent with evidence about the impact of COVID-19 on families who have children with educational or social needs are great than the general population (Brown et al. 2020; Coyne et al., 2020, Fontanesi et al., 2020).
The educational challenges experienced under the pandemic have been exacerbated by parental concerns about managing their own daily work needs as well as their child’s learning needs (e.g., Fontanesi et al., 2020; Neece et al., 2020). It comes as no surprise that the second highest need area reported by parents in this survey was family support. This area included social support, childcare, general support, and child activities. Parents reported a decrease in both formal supports as well and informal supports since the pandemic began. A conclusion being that this lack of family support contributed to the finding that over three-fourths of the parent respondents reported their current anxiety as somewhat or very high because of the COVID-19 pandemic. This finding is consistent with Willner et al. (2020) who reported extremely high levels of unmet mental health needs among caregivers for children and adults with ID because of the pandemic.
Family support has been found to be significantly related to positive family outcomes in families with children with disabilities (Kyzar et al., 2012). These outcomes include increased family functioning, increased family quality of life, and decreased family stress (Boehm & Carter, 2019). Thus, the provision of family support has been recommended for many years as a mediator to the family burden and stress reported by families with children with disabilities, and a facilitator of positive adaptation and outcomes (Patton et al., 2018; Vanegas & Abdelrahim, 2016). The decrease in formal support services and informal support networks is of most concern as most families would be at an additional risk for an increased stress burden and decreased quality of life.
Limitations
There are several limitations to this study. The sample who completed the survey was highly educated, employed, and had access to technology. Families who live in poverty or are struggling to meet basic needs such as food, housing, and/or electricity, are not likely to be represented in our data. Nor are families of diverse backgrounds. The survey collected data in real time and only provides a brief snapshot of the knowledge, beliefs, and needs of families during 2 months in 2020, at the beginning of the pandemic.
Conclusion
The present research contributes to a growing body of evidence of the challenges families of children with disabilities have faced during the COVID-19 pandemic. As stated by Willner et al. (2020), the
pandemic has demonstrated how families provide the safety net when the systems around them shut down, highlighting the need to ensure they are adequately informed, supported, valued, and prioritized. (p. 8)
Moving forward, families of children with disabilities must be at the center of all planning for emergencies that result in societal shutdowns and closures or changes in service systems. Inequity of resources must also be addressed to help all families adapt to short- and long-term changes in type, frequency, and location of critical services such as early intervention, special education, and therapeutic services. While this is an example of only one critical support for families and their children, the changes in practice and policy around schooling was reported to be a major concern and need of parents at the beginning of the pandemic. Other infrastructure supports, both formal and informal, were also identified as needed by families. Concerns included the well-being of their family members and themselves, which is understandable in times of a public health crises. These findings support the continuance of formal and informal family support services and strategies during times of crisis, as a decrease or removal of them may result in increases in anxiety and decreases in quality of life. The infrastructure that families rely on to maintain equilibrium must be supported and strengthened. Their experiences during this pandemic, as reported in this survey and others, should provide ample direction on what should happen to avoid some of the stress they have endured during future emergencies. (Neece et al., 2020; Willner et al., 2020). Last, as the data reported in this study were collected at the beginning of the pandemic, it is imperative that there continues to be examination of the impact of the pandemic on family functioning and well-being over time.
References
Aishworiya, R., & Kang, Y. Q. (2020). Including children with developmental disabilities in the equation during this COVID-19 pandemic. Journal of Autism and Developmental Disorders, 1-4. https://doi.org/10.1007/s10803-020-04670-6
Aldersey, H., Turnbull, A., & Minnes, P. (2017). Providing support that enhances a family’s quality of life. In M. L. Wehmeyer, I. Brown, M. Percy, K. A. Shogren, & W. L. A. Fung (Eds.), A comprehensive guide to intellectual and developmental disabilities (pp. 527-540). Brookes.
Alexander, R., Ravi, A., Barclay, H., Sawhney, I., Chester, V., Malcolm, V., Brolly, K., Kamalika, M., Zia, A., Tharian, R., Howell, A., Lane, T., Cooper, V., & Langdon, P. E. (2020). Guidance for the treatment and management of COVID-19 among people with intellectual disabilities. Journal of Policy and Practice in Intellectual Disabilities, 17, 256–269. https://doi.org/10.1111/jppi.12352
Barroso N. E., Mendez L., Graziano P. A., & Bagner D. M. (2018) Parenting stress through the lens of different clinical groups: A systematic review and meta‐analysis. Journal of Abnormal Child Psychology, 46, 449–461. https://doi.org/10.1007/s10802-017-0313-6
Boehm, T. L., & Carter, E. W. (2019). Family quality of life and its correlates among parents of children and adults with intellectual disability. American Journal on Intellectual and Developmental Disabilities, 124(2), 99-115. https://doi.org/10.1352/1944-7558-124.2.99
Boyle, C. A., Fox, M. H., Havercamp, S. M., & Zubler, J. (2020). The public health response to the COVID-19 pandemic for people with disabilities. Disability and Health Journal, 13(3). https://doi.org/10.1016/j.dhjo.2020.100943
Bradley, V. J. (2020). How COVID-19 may change the world of services to people with intellectual and developmental disabilities. Intellectual and Developmental Disabilities, 58(5), 355-360. https://doi.org/10.1352/1934-9556-58.5.355
Brown, S. M., Doom, J. R., Lechuga-Peña, S., Watamura, S. E., & Koppels, T. (2020). Stress and parenting during the global COVID-19 pandemic. Child Abuse & Neglect, (110). https://doi.org/10.1016/j.chiabu.2020.104699
Cluver, L., Lachman, J. M., Sherr, L., Wessels, I., Krug, E., Takotomalala, Blight, S., Hillis, G., Green, O., Butchart, A., Tomlinson, M., Ward, C. L., Doubt, J., & McDonald, K. (2020). Parenting in a time of COVID-19. The Lancet, 395(10231), 11-17. https://doi.org/10.1016/S0140-6736(20)30736-4
Coller, R. J., & Webber, S. (2020). COVID-19 and the well-being of children and families. Pediatrics, 146(4). https://doi.org/10.1542/peds.2020-022079
Coyne, L. W., Gould, E. R., Grimaldi, M., Wilson, K. G., Baffuto, G., & Biglan, A. (2020). First things first: Parent psychological flexibility and self-compassion during COVID-19. Behavior Analysis in Practice. https://doi.org/10.1007/s40617-020-00435-w
Ervin, D. A., & Hobson-Garcia, D. (2020). Community supports and COVID-19: Self-determination in a pandemic. Intellectual and Developmental Disabilities, 58(6), 453-457. https://doi.org/10.1352/1934-9556-58.6.453
Fontanesi, L., Marchetti, D., Mazza, C., Di Giandomenico, S., Roma, P., & Verrocchio, M. C. (2020). The effect of the COVID-19 lockdown on parents: A call to adopt urgent measures. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S79–S81. http://dx.doi.org/10.1037/tra0000672
Galea, S., Merchant, R. M., & Lurie, N. (2020). The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. Journal of the American Medical Association Internal Medicine, 180, 817–818. https://doi.org/10.1001/jamainternmed.2020.1562
Gassman-Pines, A., Ananat, E. O., & Fitz-Henley II, J. (2020). COVID-19 and parent-child psychological well-being. Pediatrics, 146(4), e2020007294. https://doi.org/10.1542/peds.2020-007294
Gavin, H. (2008). Understanding research methods and statistics in psychology. Sage.
Hayes, S. A., & Watson, S. L. (2013). The impact of parenting stress: A meta‐analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. Journal of Autism and Developmental Disorders, 43, 629–642. https://doi.org/10.1007/s10803-012-1604-y
Hughes, N., & Anderson, G. (2020). The experience of the COVID-19 pandemic in a UK learning disability service: Lost in a sea of ever-changing variables—A perspective. International Journal of Developmental Disabilities, 1–4. https://doi.org/10.1080/20473869.2020.1773711
IBM Corp. (2017). IBM SPSS statistics for windows (version 25.0). Author.
Kyzar, K. B., Turnbull, A. P., Summers, J. A., & Gómez, V. A. (2012). The relationship of family support to family outcomes: A synthesis of key findings from research on severe disability. Research and Practice for Persons with Severe Disabilities, 37(1), 31-44. https://doi.org/10.1007/s10803-012-1604-y
Leocani, L., Diserens, K., Moccia, M., & Caltagirone, C. (2020). Disability through COVID-19 pandemic: Neurorehabilitation cannot wait. European Journal of Neurology, e50-e51. https://doi.org/10.1111/ene.14320
Lund, E. M., Forber-Pratt, A. J., Wilson, C., & Mona, L. R. (2020). The COVID-19 pandemic, stress, and trauma in the disability community: A call to action. Rehabilitation Psychology, 65(4), 313-322. http://dx.doi.org/10.1037/rep0000368
Masonbrink, A. R., & Hurley, E. (2020). Advocating for children during the COVID-19 school closures. Pediatrics, 146(3). https://doi.org/10.1542/peds.2020-1440
Morgan, D. L. (2008). Snowball sampling. In L. Given (Ed.), The SAGE encyclopedia of qualitative research methods (pp. 816-817). SAGE.
Neece, C., McIntyre, L. L., & Fenning, R. (2020). Examining the impact of COVID-19 in ethnically diverse families with young children with intellectual and developmental disabilities. Journal of Intellectual Disability Research, 64(10), 739-749. https://doi.org/10.1111/jir.12769
Patrick, S. W., Henkhaus, L. E., Zickafoose, J. S., Lovell, K., Havorson, A., Loch, S., Letterie, M., & Davis, M. M. (2020). Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics, 146(4), e2020016824. https://doi.org/10.1542/peds.2020-016824
Patton, K. A., Ware, R., McPherson, L., Emerson, E., & Lennox, N. (2018). Parent‐related stress of male and female carers of adolescents with intellectual disabilities and carers of children within the general population: A cross‐sectional comparison. Journal of Applied Research in Intellectual Disabilities, 31(1), 51-61. https://doi.org/10.1111/jar.12292
Prime, H., Wade, M., & Browne, D. T. (2020). Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist, 75(5), 631-643. https://doi.org/10.1037/amp0000660
Russell, B. S., Hutchinson, M., Tambling, R., Tomkunas, A. J., & Horton, A. L. (2020). Initial challenges of caregiving during COVID-19: Caregiver burden, mental health, and the parent-child relationship. Child Psychiatry & Human Development, 51, 671-682. https://doi.org/10.1007/s10578-020-01037-x
Sabatello, M., Landes, S. D., & McDonald, K. E. (2020). People with disabilities in COVID-19: Fixing our priorities. The American Journal of Bioethics, 20(7), 187-190. https://doi.org/10.1080/15265161.2020.1779396
Thompson, J. R., & Nygren, M. A. (2020). COVID-19 and the field of intellectual and developmental disabilities: Where have we been? Where are we? Where do we go? Intellectual and Developmental Disabilities, 58(4), 257-261. https://doi.org/10.1352/1934-9556-58.4.257
Tulsa SEED Study Team. (2020). Parents, teachers, and distance learning during the COVID-19 pandemic: A snapshot from Tulsa, OK. https://medium.com/@TulsaSEED/parents-teachers-and-distance-learning-during-the-covid-19-pandemic-a-snapshot-from-tulsa-ok-5b5fdb54ea18
Turk, M. A., Landes, S. D., Formica, M. K., & Goss, K. D. (2020). Intellectual and developmental disability and COVID-19 case-fatality trends: TriNetX analysis. Disability and Health Journal, 13. https://doi.org/10.1016/j.dhjo.2020.100942
Vanegas, S. B., & Abdelrahim, R. (2016). Characterizing the systems of support for families of children with disabilities: A review of the literature. Journal of Family Social Work, 19(4), 286-327. https://doi.org/10.1080/10522158.2016.1218399
Weaver, J. L. & Swank, J. M. (2020). Parents’ lived experiences with the COVID-19 pandemic. The Family Journal: Counseling and Therapy for Couples and Families, 1-7. https://doi.org/10.1177/1066480720969194
Wehmeyer, M. L., Brown, I., Percy, M. E., Shogren, K. A., & Fung, W. L. A. (Eds.). (2017). A comprehensive guide to intellectual and developmental disabilities. Brookes.
Williamson, H. J., & Perkins, E. A. (2014). Family caregivers of adults with intellectual and developmental disabilities: Outcomes associated with US services and supports. Mental Retardation, 52(2), 147-159. https://doi.org/10.1352/1934-9556-52.2.147
Willner, P., Rose, J., Kroese, B. S., Murphy, G. H., Langdon, P. E., Clifford C., Hutchings, H., Watkins, A., Hiles, S., & Cooper, V. (2020). Effect of COVID-19 pandemic on the mental health of caregivers of people with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities, 33(6), 1523-1533. https://doi.org/10.1111/jar.12811
Woodman, A. C., Mawdsley, H. P., & Hauser‐Cram, P. (2015). Parenting stress and child behavior problems within families of children with developmental disabilities: Transactional relations across 15 years. Research in Developmental Disabilities, 36C, 264–276. https://doi.org/10.1016/j.ridd.2014.10.011

