14 Increasing Access to Augmentative and Alternative Communication Services for People with Complex Communication Needs During COVID-19 and Beyond
Cristina L. Pujol; Anamaria Nevares; and Michelle Schladant
Pujol, C. L., Nevares, A., & Schladant, M. (2021). Increasing Access to Augmentative and Alternative Communication Services for People with Complex Communication Needs During COVID-19 and Beyond. Developmental Disabilities Network Journal, (2), 170–191. https://doi.org/10.26077/4345-8A31
Plain Language Summary
COVID-19 has affected the disability network across the world. There are millions of people who cannot use their natural speech. Augmentative and alternative communication (AAC) tools help these people to communicate. Examples of AAC include printed pictures and speech-generating devices. Professionals work with the person and their family to choose the right AAC. Often, people who use AAC need ongoing support. During COVID-19, many AAC services stopped to keep people safe. This paper describes how one center adapted AAC services. First, we outline the use of tele-AAC services. Then, we discuss how we used state AAC resources. Last, we highlight how we used tele-coaching to support caregivers. We conclude with suggestions for providing tele-AAC during COVID-19 and beyond.
The COVID-19 global pandemic has affected the disability network across the world (World Health Organization [WHO], 2020). Approximately 4 million Americans with complex communication needs (CCNs) cannot use their natural speech to communicate (Beukelman & Mirenda, 2013). Augmentative and alternative communication (AAC), a form of assistive technology (AT), is an evidence-based approach to help people with CCNs communicate (Morin et al., 2018). AAC consists of AT tools such as printed pictures and symbols displayed on manual boards and speech-generating devices (American Speech-Language-Hearing Association [ASHA], n.d.a.). People with CCNs who may have a temporary or permanent need for AAC include individuals with developmental disabilities such as autism spectrum disorders (ASD), cerebral palsy (CP), intellectual disabilities (ID), and genetic disorders (ASHA, n.d.a.; Morin et al. 2018). Furthermore, people with acquired conditions such as traumatic brain injuries, cerebral vascular accidents, brainstem strokes, and amyotrophic lateral sclerosis (ALS) may also require AAC services (Rehabilitation Engineering Research Center on AAC, 2019).
To assess a person’s need for AAC, a team of professionals work together with the person and their caregivers to determine the appropriate AAC system (Schladant et al., in press). Often, people with CCNs require face-to-face and ongoing AAC support to promote communicative competence (ASHA, n.d.a.). However, with school closures and stay-at-home orders resulting from the COVID-19 pandemic, many services for people with disabilities abruptly stopped worldwide (Fong et al., 2020; Salas-Provance et al., 2020). Service providers needed to swiftly adapt speech and language services to ensure people’s safety (Fong et al., 2020). This paper describes how one AT Program at a University Center for Excellence in Developmental Disabilities (UCEDD) adapted AAC services and increased access to support using (a) tele-AAC assessment practices, (b) services through a partnership with our state AT Act program, and (c) tele-coaching strategies to help providers and caregivers in their facilitation and implementation of AAC services. We will present a case example highlighting how we used these innovative approaches and discuss key considerations in tele-AAC practices to help people with CCNs and their caregivers during COVID-19 and beyond.
Findings from over three decades of research demonstrate that AAC improves outcomes for children and adults with CCNs. These outcomes include enhancing their ability to be understood, assisting with conversation maintenance, and increasing social interactions (Beukelman & Mirenda, 2013; McNaughton & Light, 2015). A meta-analysis conducted by Ganz et al. (2012) revealed AAC interventions effectively promoted academic performance and reduced challenging behaviors for children with CCNs. In a systematic review across 17 studies on AAC service delivery, Morin et al. (2018) found that high-tech AAC improved communication outcomes for people with CCNs. Researchers in the study also found that people using high-tech AAC did not perform significantly better than those using other low-tech forms of AAC, such as manual communication boards. This finding suggests that a range of high- and low-tech AAC modalities are effective in improving communication skills for people with CCNs (Morin et al., 2018).
Furthermore, researchers have shown that AAC benefits not only people with CCNs but also benefits their caregivers. For example, Aydin and Diken (2020) surveyed families of children using high-tech AAC and found that caregivers reported that their children’s independence and communicative competence improved at school and in the community. In a study conducted by Schladant and Dowling (2020), mothers of children with fragile X syndrome found various low- and high-tech AAC tools useful in addressing their children’s communication needs at home. In a study conducted by Richardson et al. (2019), adults with ASD who used AAC in their employment reported success in using AAC with appropriate support from their employers. Although there are proven benefits to AAC use for people with CCNs, there are many challenges (Light et al., 2019; Schladant & Dowling, 2020).
One of the biggest challenges for AAC users and their caregivers is access to AAC support (Baxter et al., 2012). Smith and Connelly (as cited by Baxter et al., 2012) found that few people with CP had ongoing support for programming and maintenance once provided with their AAC devices. In another study, parents described difficulties finding AAC specialists or professionals with sufficient AAC expertise (McNaughton et al., 2015). In a similar study, the lack of local AAC support was one of the major obstacles impacting successful AAC integration in the home (Schladant & Dowling, 2020). Last, when working with children from linguistically diverse backgrounds, Soto and Yu (2014) described difficulties finding professionals with in-depth knowledge about bilingualism related to AAC and language development.
To address these challenges in AAC implementation and reduce the risk of device abandonment, persons with CCNs and their caregivers often require face-to-face and ongoing support by a team of professionals working together (Jackson & Schladant, 2017). Effective AAC service delivery plays a critical role in determining whether people with CCNs will be successful AAC users in everyday life (Steel et al., 2012). Although federal laws mandate AAC service delivery in the community, educational, and vocational settings, service providers also face many challenges in effectively implementing AAC services (Schladant & Dowling 2020). First, AAC service delivery often requires multiple perspectives by an interdisciplinary team with AAC knowledge and expertise (Jackson & Schladant, 2017). Second, AAC service delivery is a collaborative, decision-making process that includes numerous steps and the involvement of key stakeholders (Binger et al., 2012). Last, when considering AAC for people with CCNs, merely providing a person with access to the device is not enough (Schladant & Dowling, 2020). To optimize the integration of AAC in everyday life, the AAC users and their caregivers and providers may require ongoing services to learn the selected system (Schladant et al., in press).
AAC services are most effective when provided by an interdisciplinary team (Jackson & Schladant, 2017). These team members often include the person with CCNs, caregivers, speech-language pathologists (SLPs), assistive technology professionals (ATPs), educational/vocational specialists, occupational therapists (OTs), physical therapists (PTs), vendors, and other medical professionals as needed (ASHA, n.d.a., Binger et al., 2012). Central to the team is the person with CCNs and their caregivers (Schladant et al., in press). A person- and family-centered approach provides a process for identifying strengths and resources and ensures shared goals and decision-making for AAC use (Mandak et al., 2017). Each individual lends a unique perspective and area of expertise to make recommendations about the most appropriate AAC system to promote functional communication across partners and settings (Jackson & Schladant, 2017). The interdisciplinary team works together to gather and synthesize information and collaborate to develop coordinated AAC recommendations for the person with CCNs (Schladant et al., in press).
The AAC assessment process involves several necessary steps, with key stakeholders being instrumental to this process. First, it is imperative to consider the various contexts in which the AAC system will be used, including the community and educational settings and communication partners (Beukelman & Mirenda, 2013). Second, collaborating with key stakeholders, such as the caregivers, school district, and other allied health professionals, is critical for successfully implementing the AAC system into the natural environment (Binger et al., 2012). Third, access to devices to trial during the assessment process, knowledge of various funding sources, and documentation required for AAC system acquisition are necessary (Baxter et al., 2012; Beukelman & Mirenda, 2013; Jackson & Schladant, 2017). Effective communication and ongoing support among the AAC user, their caregivers, and other key stakeholders are essential to ensure the appropriate AAC selection and reduce device abandonment risk (Schladant et al., in press). In the section that follows, we highlight how one AT program at a UCEDD swiftly modified services to increase access to AAC support to address past, present, and future challenges in AAC service delivery.
AAC Service Delivery: Past, Present, and Future Directions
Setting
The AT program described in this paper is in the southeastern U.S. and is one of the 67 designated UCEDD in the U.S. and territories. As a UCEDD, our center employs an interdisciplinary faculty representing over 15 disciplines to provide: preservice training to 80 pediatric interdisciplinary graduate and post-graduate students; direct services to more than 14,000 children and young adults; community outreach to over 3,000 consumers and professionals; and research activities, technical assistance, and information dissemination reaching thousands each year. Our AT program provides AT and AAC services to children and adults with disabilities and their caregivers. Our AAC interdisciplinary team consists of two bilingual SLPs, an OT, a PT, and two ATPs. AAC evaluations emphasize family involvement to determine an appropriate AAC plan specific to the person’s needs. The center’s AT program also offers information and referrals, device demonstrations, AT training and outreach, and a device-lending library through a 20-year partnership with our state AT Act program.
Previous AAC Service Delivery Model
Our AT program is one of the few facilities in the region that offers AAC assessment and intervention services. Before the COVID-19 pandemic, we provided all AAC services face-to-face at our center. As shown in Table 1, the essential steps in our interdisciplinary AAC process included: (a) gathering background information; (b) conducting the initial assessment; (c) implementing a device trial; (d) obtaining the device and assisting with device programming and maintenance.
| Key components | Steps | Primary team member(s) responsible |
|---|---|---|
| Gather background information about the person with CCNs from the primary caregiver(s) |
|
Primary caregiver(s), the person with CCNs |
| The interdisciplinary team conducts an initial assessment |
|
The person with CCNs, primary caregiver(s), assistive technology specialist (ATP), speech language pathologist (SLP), the person with CCNs’ SLP, OT, PT |
| Conduct device trial with the person with CCNs and primary caregiver |
|
SLP, OT, ATP, the person with CCNs, and primary caregiver(s) |
| Apply for device funding |
|
ATP, SLP, primary caregiver(s) |
| Device training after the device is obtained |
|
ATP, primary caregiver(s), the person with CCNs |
Gather Background Information
Before the face-to-face appointment at our center, the person’s primary caregiver completed a comprehensive background form and provided the team with previous reports and short videos to determine their current communication abilities. Next, our team reviewed the background information, videos, and prior reports to develop an AAC assessment plan. Using a feature match approach based on the person’s communication needs (Beukelman & Mirenda, 2013), our team selected a minimum of three AAC devices with a range of vocabulary displays, access methods, and activities to use during the assessment. When choosing the devices, vocabulary, and activities, our team also considered each person’s linguistic and cultural diversity.
The Initial AAC Assessment
On the day of the face-to-face assessment, one of our SLPs led the interaction with the child or adult and was assisted by one of our ATPs and OT or PT if needed. During the appointment, the caregiver(s) observed the assessment through a one-way mirror. Our ATP accompanied the caregiver(s), who explained the strategies and the methods used by our SLP and collected more background information from the caregiver(s). After our SLP completed the AAC assessment, the caregiver(s) met with our team to discuss preliminary recommendations and planned for the AAC device trial period.
The AAC Device Trial Period
Based on feedback from the caregiver(s) and our team’s recommendations, the person and their caregiver(s) participated in three to four face-to-face device trial sessions over a 4- to 6-week period to collect data and determine the most appropriate AAC system. During this time, we leveraged our partnership with our state AT Act program to provide the person and their caregivers with a device loan to use at home during the device trial period. Our SLP trained the caregiver to use, program, and maintain the device, as well as provided caregivers with information on essential AAC strategies to support the person’s communication. Our team also invited caregivers to bring the person’s service providers (e.g., SLP, OT, PT) to participate in the device trial training and share their input.
Obtain AAC Device and Training
After the device trial period, our SLP finalized the AAC written report. Our ATP then worked with the caregiver and AAC vendor’s funding department to complete the paperwork to obtain the device through insurance. In addition to the written AAC report, the funding packet included a Certificate of Medical Necessity completed by the person’s primary care physician, an Assignment of Benefits to allow the AAC vendor’s funding department to communicate with the insurance on behalf of the person, and a Device Selection sheet specifying device features. After the person received their funded device, our team connected the family with our state AT Act program for further training and resources to support device programming and maintenance.
Partnership with Our State AT Act Program
As previously mentioned, one way we leveraged support to offer AAC services was through a partnership with our state AT Act program, funded through the Assistive Technology Act of 2004 (The AT Act, 2004). Every U.S. state and territory is supported by the AT Act, which provides funding to states to assist individuals with disabilities to obtain AT devices and services (The AT Act, 2004). The purpose of state AT Act programs is to increase access to and acquisition of AT devices and services to people with disabilities (AT Act, 2004). These state AT Act programs offer three core services relevant to AAC. These services include: (a) information and assistance on AAC devices and support, including finding local AAC service providers, vendors and securing AAC funding; (b) AAC device demonstrations; and (c) free short-term AAC device loans (Binger et al., 2012). State AT Act programs are required to serve all people with all types of disabilities and in all environments (e.g., early intervention, K-12 education, post-secondary, vocational rehabilitation, community living, aging services). These programs address all types of AT along with mainstream accessible information and communication technologies.
Before the onset of COVID-19, our team supplemented the AAC assessment with services from our state AT regional office, housed at our center. Caregivers borrowed a range of AAC devices, including switches and mounts, during the device trial period. In-person AAC demonstrations during the trial and acquisition phase provided the opportunity for people with CCNs and their caregiver(s) to become familiar with different types of AAC by comparing and contrasting each device’s functions and features through hands-on exploration. Last, after the caregiver acquired the device, our state AT Act program offered caregivers and providers additional training and resources in programming and maintaining the device.
Challenges
Although our team used a systematic process for face-to-face services and leveraged our partnership with our state AT Act program, some caregivers faced challenges in obtaining AAC services. As one of the only AAC programs in our region, one barrier to receiving services was our center’s location in a large metropolitan city. Therefore, families residing in other cities or the counties’ extreme ends found it difficult to attend face-to-face sessions because of traffic and distance. Some of our clients with significant motor or medical issues found leaving their homes a burden. Some caregivers of children with ASD also reported problems with their child’s adaptability to new environments. They were worried about their child’s ability to feel comfortable in a clinical setting. When COVID-19 hit in March 2020, the pandemic provided our team with an opportunity to address past and current challenges in AAC service delivery.
AAC Service Delivery During COVID-19: A Shift to Tele-AAC Practice
While we typically conducted AAC service delivery face-to-face, this was not possible due to the COVID-19 pandemic and federal and state mandates to socially distance and stay-at-home orders (Centers for Disease Control and Prevention [CDC], 2020). It is unclear how long these guidelines will be in place. Many people with CCNs also have underlying medical conditions placing them at higher risk for contracting COVID-19. Therefore, we needed to adapt our AAC services to increase access and continue providing support to people with CCNs and their caregivers. While most service delivery systems have made some pivot to telehealth, the implications of these changes for AAC users have not been adequately explored. In the section that follows, we discuss key considerations in tele-AAC assessment practices and present a case example illustrating how we shifted our AAC services to a tele-AAC model.
Tele-AAC Assessment Practices
Telehealth, also known as telepractice, is defined by ASHA as
…the application of telecommunications technology to the delivery of speech-language pathology and audiology professional services at a distance by linking clinician to client/patient or clinician to clinician for assessment, intervention, and/or consultation. (ASHA, n.d.b.)
In a systematic review on telehealth in ASD, Knutsen et al. (2016) found that telepractice increased access to services and specialists, provided opportunities for caregiver coaching, and supported service providers and educators. The researchers also found consistent patterns of high acceptance by caregivers and efficacy across various settings, caregivers, and formats. Furthermore, Snodgrass et al. (2016) highlighted the benefits of implementing telepractice in speech and language therapy service delivery, such as reduced travel time and increased access to services for people in rural areas or neighborhoods. Researchers in other studies also found no difference in speech and language intervention outcomes between the use of telepractice services and traditional on-site services (Grogan-Johnson et al., 2013, Hall et al, 2014).
Tele-AAC is a unique type of telepractice in the field of speech and language pathology that requires technical expertise in both telepractice and AAC systems (Anderson et al., 2012). Tele-AAC services range from direct services (where an AAC user receives real-time feedback on their device from an experienced clinician) to more indirect services (where novice practitioners and family members receive feedback to support the AAC user; Hall & Boisvert, 2014). The real-time feedback from an expert in AAC in both direct and indirect tele-AAC practice is crucial to successfully help the AAC user (Hall & Boisvert, 2014). In a series of case studies, Curtis (2014) found that tele-AAC provided access to skilled AAC clinicians not otherwise available in the community because of geographic constraints, travel issues, and time. Also, tele-AAC services made it easier for AAC users and families to obtain ongoing services in the home and fostered collaboration with home health therapists.
As a result of the global pandemic, our center shifted our AAC service delivery model from clinician-led face-to-face sessions to a caregiver-led tele-AAC approach. To conduct tele-AAC assessments, we followed the ASHA Code of Ethics (ASHA, 1970) and used our center’s enterprise license, Zoom for Healthcare,™ a HIPAA-compliant video conferencing platform. The Health Insurance Portability and Accountability Act and supplemental legislation (collectively referred to as HIPAA) lays out privacy and security standards that protect the person’s health information (CDC, 2018). As shown in Table 2, the key steps and technology considerations in our tele-AAC service delivery model included: (a) conducting a technology-based assessment to prepare the caregiver for the tele-AAC process, (b) conducting a tele-AAC assessment guided by the interdisciplinary team and facilitated by the caregiver, (c) coaching the caregiver during tele-AAC device trial period, (d) providing ongoing support to the AAC user and caregivers to obtain, program and maintain the AAC device through our partnership with our state AT Act program.
| Key Components | Tele-AAC Steps | Communication Methods/Technology Needs |
|---|---|---|
| Conduct a technology-based assessment to prepare the family for the tele-AAC assessment |
|
Phone, email, Computer/ tablet, video conferencing/ Zoom,™ U.S.P.S, FedEx, UPS |
| Conduct tele-AAC assessment guided by the interdisciplinary team and facilitated by the caregiver. |
|
Computer/tablet, Zoom,™ smartphone/tablet, mount, Bluetooth headphones, pre-programmed AAC device(s), Screen Mirroring app, screen sharing |
| Coach caregiver during tele-AAC device trial. |
|
Computer/tablet, Zoom™,
pre-programmed AAC device, Bluetooth headphones, Screen Mirroring app, screen sharing |
| Provide ongoing support to the AAC user and caregiver(s) during acquisition, programming, and maintenance of the AAC device. |
|
Phone or computer/tablet, Zoom™ |
Conduct Technology-Based Assessment
Before meeting the caregivers for the tele-AAC appointment, one of our ATPs contacted the caregiver via telephone or Zoom™ to explain the tele-AAC assessment process and procedures. This call included (a) explaining how to set up their profiles on the electronic medical record system and downloading the Zoom™ software to their device, (b) obtaining consent to record the sessions, (c) explaining the tele-AAC procedures, and (d) confirming the time and date of the tele-appointment. After this phone call, one of our SLPs and ATPs scheduled the initial consult with caregiver(s) to (a) review the person’s current communication abilities, developmental and medical history, (b) discuss environmental considerations and technology set-up, and (c) determine preferred activities to motivate and engage the AAC user during the assessment.
To prepare the caregiver(s) for the tele-AAC services, we conducted a technology needs assessment to evaluate the home environment. Technology concerns included the caregiver’s access to appropriate technology such as reliable Internet connection, smartphone, computer or tablet with webcam, mount, and Bluetooth™ headphones. Caregivers provided our SLP with preferred activities to have prepared for the day of the assessment. We also encouraged caregivers to invite any other service providers to attend the assessment either in the caregiver’s home or to join the session remotely via Zoom.™ Before the tele-AAC assessment, our SLP borrowed device(s) from our state AT Act program’s lending library and programmed the devices with target vocabulary before shipping the device to the caregiver. If the caregiver had questions regarding the device set-up, our ATP scheduled a videoconference or phone call to answer their questions.
Conduct Tele-AAC Assessment
On the tele-AAC assessment day, our SLP coached the caregivers throughout the session using Bluetooth™ headphones. Using parent-coaching techniques (Roberts & Kaiser, 2011), our SLP directed the caregiver on specific AAC strategies (e.g., modeling, least to most prompting) to facilitate the person’s use of the device. Our SLP used an iPad™ with various communication apps and downloaded the screen mirroring app, Smart Mirror – TV & Device on her iPhone™ to project the AAC device screen on her laptop. She then used screen sharing via Zoom™ to show the caregiver how to program words on the device. After we gathered the necessary data and clinical observations during the assessment, we met with the caregiver(s) to discuss preliminary findings and recommendations for the subsequent device trial period.
Coach Caregiver During Tele-AAC Device Trial
If there was a need for a dedicated high-tech AAC, we collaborated with one of our local AAC vendor representatives to obtain the device loan directly from the company. The AAC device trial period focused on the implementation of one to two AAC systems. Caregivers were asked to invite the AAC client’s service providers to participate in the device trials and provide additional feedback.
As our service delivery model shifted from face-to-face sessions to telepractice, our team also shifted from a clinician-led approach to a caregiver-led process. A meta-analysis conducted by Roberts and Kaiser (2011) found that caregiver-implemented language interventions effectively promoted language development in young children with disabilities. Snodgrass et al. (2016) implemented a telepractice framework incorporating caregiver training and coaching to aid SLPs in providing remote early intervention services to children with communication disorders and found that parents were able to effectively learn strategies (e.g., modeling, mand-model, and time delay) to improve their child’s communication skills.
Furthermore, in a technical report by Hall and Boisvert (2014), the authors discussed clinical aspects for supporting caregivers and providers to implement tele-AAC services. They highlighted indirect AAC services, such as Active Consultation and e-Supervision, to coach caregivers on using the AAC device with the client. The authors emphasized that when working with caregivers and professionals who are less familiar with AAC, the immediacy of the feedback offered via Active Consultation is essential to successfully support caregivers and AAC users (Hall & Boisvert, 2014).
Provide Ongoing Remote Support
The challenges faced with COVID-19 allowed our team to think more creatively about leveraging our partnership with our state’s AT Act program to deliver synchronous and asynchronous AAC support. Synchronous support occurred in real-time. One of our ATPs, who coordinates the regional office for our state AT Act program, provided device loans and training to the caregiver(s) and providers on how to program and maintain the device. Once caregivers obtained their device through funding, the ATP scheduled a remote meeting to discuss the device’s features and provided technical support, as necessary.
In addition to synchronous support, we collaborated with our state AT Act program to provide asynchronous support by creating YouTube video demonstrations and curating a collection of online resources. This type of asynchronous support allowed caregivers the opportunity to view video demonstrations and resources at their own time and pace. Hence, we developed an online library of video tutorials and device demonstrations that could be accessed “anytime, anywhere.” We archived and posted these videos on our center’s YouTube channel, a platform familiar to the public. We also made these videos available on our state AT Act program website. In the next section, we present a case example to illustrate how we used these tele-AAC practices.
Case Example
Erica and David
Erica is the mother of David, a 4-year-old boy with ASD. He is an emerging communicator with limited verbal speech. Although David had been receiving speech therapy interventions and applied behavior analysis (ABA) services for the past 2½ years, he did not have a reliable means to communicate with his family members, peers, and other communication partners. His previous AAC experience included some low-tech forms such as picture symbols and single message voice output devices that he used in school and therapies. Because of COVID-19, David no longer attended school in person and received all educational services at home through remote learning. He also received OT and ABA therapies at home. His SLP temporarily suspended services because she was not able to provide telepractice services at the time. Erica contacted our AAC team in the summer of 2020 to help David find a reliable way to express his immediate needs and make choices effectively and efficiently. His complex communication needs limited his interactions with others and increased his frustration when he could not meet his needs.
Preparing for the Tele-AAC Process
Before the tele-AAC assessment, we conducted a video consultation with Erica to explain the tele-AAC process and how to log in to the electronic medical record to access Zoom™. We also determined her technology needs and the computer equipment needed to complete the assessment. We decided that based on her previous experience with using technology for David’s remote learning and videoconferencing, she would be comfortable using Zoom™ for the upcoming session. We also problem-solved what device she would use to view the AAC device screen and where to set up the device’s camera. We determined that Erica would use her smartphone camera to view the AAC screen via Zoom™. David’s OT would be part of the assessment to hold the smartphone and help engage David during the session. To interact with our team via Zoom™, Erica decided to use her laptop. She used her Bluetooth™ headphones via her computer to communicate with our team discreetly. We planned a few of David’s preferred activities, such as bubbles, a favorite pop-up toy, snack, and balloons. Last, we explored potential AAC systems based on David’s communication needs and feature-matching.
After the video consultation, we coordinated a device loan through our state AT Act program to obtain an iPad™ with several communication apps. We pre-programmed each communication app with specific vocabulary related to David’s preferred activities. As shown in Figure 1, we programmed LAMP Words for Life™, a core word-based system with the following words: “want,” “go,” “stop,” “help,” and “turn.” We programmed the TouchChat™ app, a category word-based system with various words, including pronouns, verbs, and activity-specific words (see Figure 2). Finally, we programmed an activity-based communication app called the Go Talk Now™ with four symbols, which included “want,” “more,” “bubbles,” and a picture of a preferred toy (see Figure 3). We planned to use these pre-selected words and vocabulary during David’s favorite activities. After programming the communication apps, we shipped the iPad™ to Erica’s home.
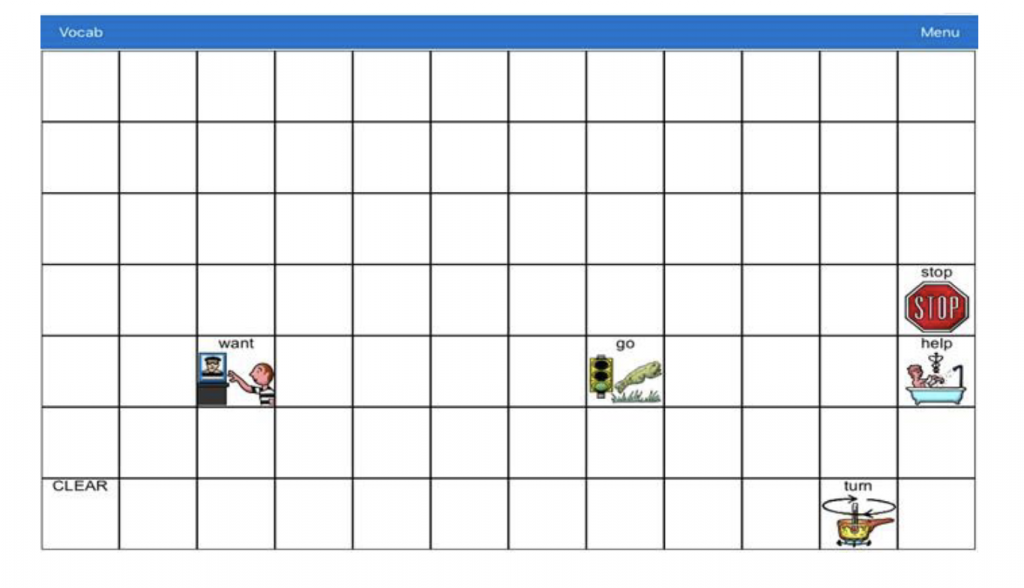
Pre-Programmed LAMP Words for LifeTM Vocabulary
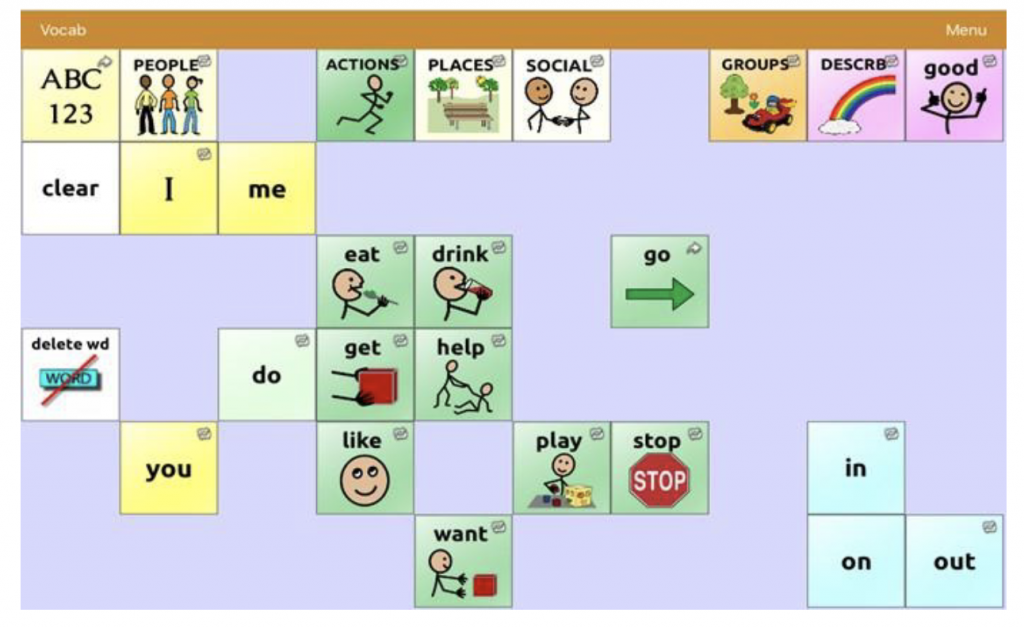
Pre-Programmed AAC Device TouchChatTM Software
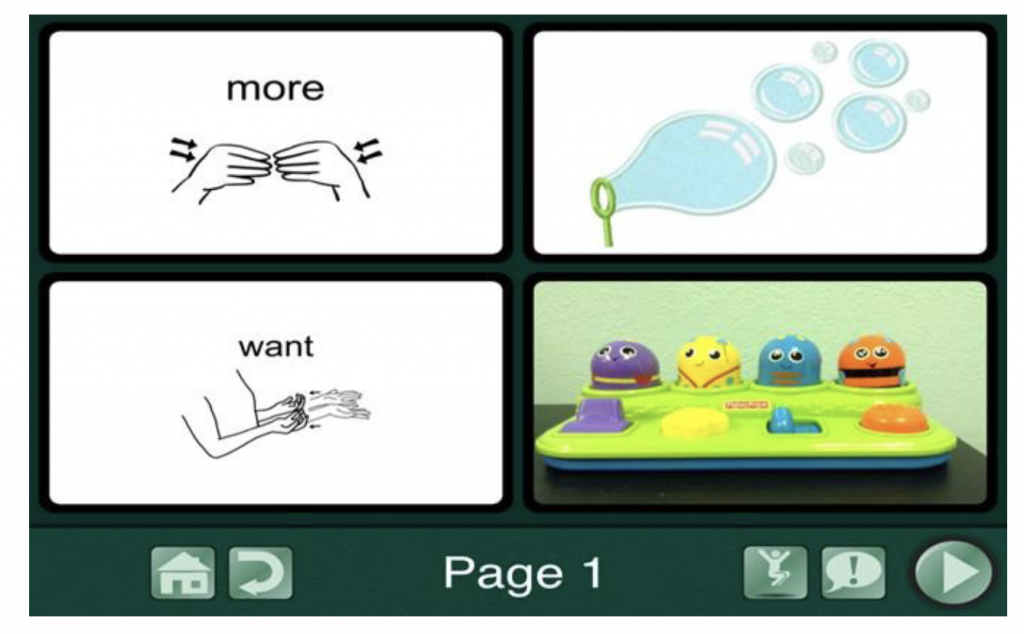
Pre-Programmed AAC Device Go Talk NowTM
Conducting the Tele-AAC Assessment
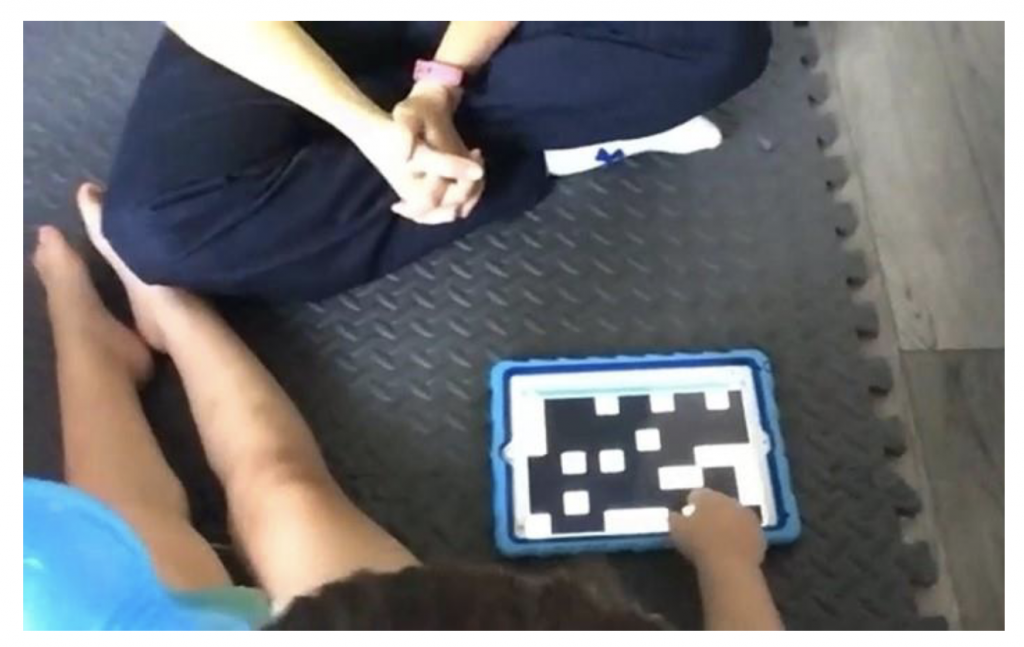
On the day of the tele-AAC assessment, our team met with Erica, David, and his OT via Zoom™ (see Figure 4). As shown in Figure 5, Erica logged into Zoom™ on her smartphone, and David’s OT held it so our team could view David’s AAC screen. Erica also logged into Zoom™ on her laptop to see our SLP and ATP, who participated remotely. Using her Bluetooth™ headphones, Erica could hear our SLP, who guided her on eliciting David’s use of the device to communicate, responding to his communication attempts, and navigating the pages on the AAC devices. David’s OT held the smartphone’s camera to ensure we could see the AAC screen. The OT also assisted Erica with behavior support to maintain David’s engagement during the assessment. Our SLP utilized a screen mirroring app on her smartphone and screen sharing on Zoom™ to guide Erica on programming more words on-the-spot. Once the team gathered sufficient information, we discussed each communication apps’ features with Erica and David’s OT to decide which AAC system to use during the trial period. Using the input provided by Erica and David’s OT, our team discussed how to proceed for the trials. We found the Go Talk Now™ app was too limiting for David’s communication needs, although there were some features of this app Erica found helpful. We also thought navigating the TouchChat™ app required longer periods of sustained attention, which was too difficult for David at the time. Therefore, we decided to trial LAMP Words for Life™ as this vocabulary system provided David with immediate feedback and an efficient way to communicate his needs and wants.
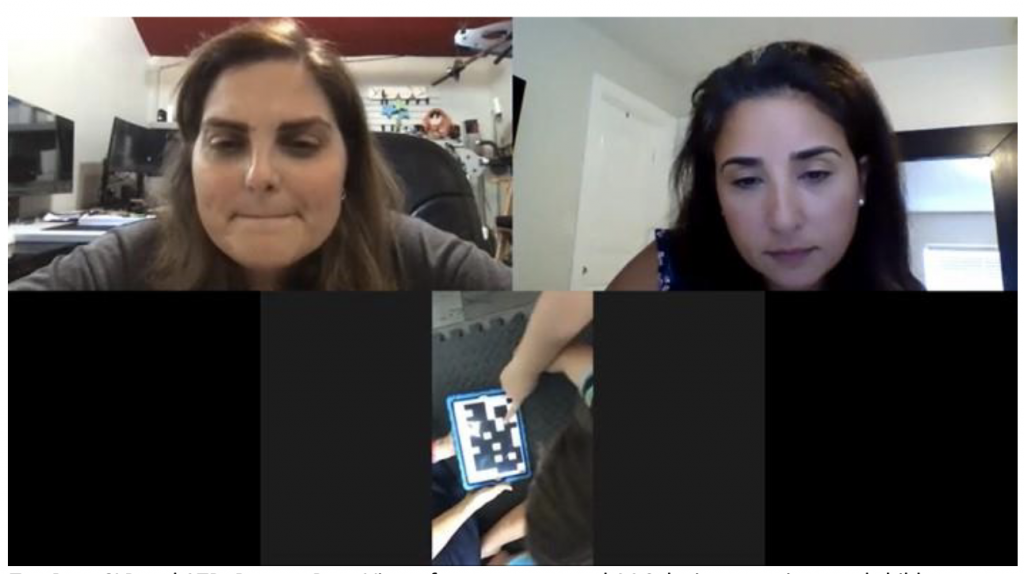
Tele-AAC Assessment.
Top Row: SLP and ATP. Bottom Row: View of pre-programmed AAC device, caregiver, and child
Coaching Erica During the AAC Device Trial
Following the tele-AAC assessment, our SLP conducted a 4-week trial with Erica and David. During this time, we helped Erica obtain the Via Pro™ device with LAMP Words for Life™ from our local AAC vendor representative, who also provided Erica with device training and technical support. This type of support offered Erica, David, and his therapists the opportunity to try out the AAC device for 4 weeks. During this trial period, Erica and David’s therapists explored the software features before we made a final decision.
Additionally, during this time, we provided Erica with targeted AAC strategies using parent-implemented techniques (Roberts & Kaiser, 2011) to support effective AAC implementation in David’s natural environment. Following the principles of aided language stimulation (Biggs et al, 2019), we guided Erica on how to model language by pointing to the symbol on David’s device and repeating the word at the same time the device speaks. We focused on coaching Erica and his therapists to engage with David in various communication acts such as requesting, making comments, and directing actions throughout a particular activity. The coaching also included training in the prompt hierarchy using least-to-most prompts (e.g., when to offer a gesture, verbal, or physical cue to elicit a response) to maximize David’s intentional use of the device (Finke et al, 2017). Between trial sessions, Erica used natural routines to teach David how to communicate with his AAC device. At the beginning of each trial session, our SLP helped Erica reflect on successes and challenges she faced during the week and collaborated with her to solve any obstacles she encountered.
Providing Continued Support
Once we completed the trial and gathered enough information, we finalized the written AAC report. We then proceeded with helping Erica apply for funding to obtain David’s device through private insurance. After receiving his device, we connected Erica and his team with our ATP, who coordinates services for our state AT Act Program to support Erica and David’s team in programming and maintaining his device. We leveraged our partnership with our state AT program to support their ongoing AAC implementation and maintenance.
By shifting our AAC service delivery from a clinician-implemented to a caregiver-implemented approach, Erica and David’s team played a more active role in the assessment process. As a result, they received more hands-on practice and direct guidance to support David’s AAC use in the natural environment. Ultimately, the tele-AAC model offered our team the opportunity to serve in a supportive role, providing targeted feedback, and allowing the space for Erica and David’s team to reflect and determine the strategies that could support David’s continued AAC use.
Tele-AAC Service Delivery: Future Directions
The COVID-19 pandemic has brought about dramatic changes to many aspects of our lives (WHO, 2020) and significantly impacted AAC service delivery. The COVID-19 global pandemic has accelerated the use of telepractice in SLP globally as an alternative service delivery during stay-at-home orders (Fong et al., 2020). There are many challenges in implementing AAC service delivery, such as geographic constraints, access to skilled AAC clinicians, and ongoing support to integrate AAC in the natural environment (Curtis, 2014; Light et al., 2019). There is emerging evidence to support the implementation of tele-AAC, a newer subset of telepractice in the field of SLP (Hall & Boisvert, 2014). The shift to tele-AAC practices as a result of the global pandemic offers a unique opportunity to address past, current, and future challenges in AAC service delivery. Competent tele-AAC implementation is contingent upon adequate technological infrastructure such as hardware/software, internet, telecommunications, and trained personnel in both AAC and telepractice (Anderson et al., 2012). The tele-AAC practices and technological infrastructure described in this paper resulted in innovative and feasible solutions to AAC service delivery during the COVID-19 pandemic that has future implications for providing effective AAC intervention.
One of the biggest obstacles we faced in our tele-AAC assessment process was the additional technology needed to view the client’s AAC device screen and for the caregivers to view our AAC screen for modeling how to program the device on-the-spot. During the tele-AAC assessment, the remote AAC clinician must be able to view vocabulary displayed on the device’s screen, the message generated, and the caregiver and person interacting with the AAC device (Hall & Boisvert, 2014). The caregiver must also be able to view the remote AAC clinician’s screen to allow for shared and concurrent interaction between the caregiver, clinician, and shared content on the screen (Hall & Boisvert, 2014). There are several ways to address the challenge of AAC screen sharing. With Erica and David (as shown in Figure 5), we used a no-tech method where Erica logged into Zoom™ on her smartphone, and David’s OT held it so the team could view David’s AAC screen. Although not ideal, a no-tech option for caregivers without a way to mount the webcam could be to have an additional person in the client’s setting hold the smartphone or tablet to view the AAC screen. Another option that we have used with other AAC clients is to mount the smartphone or tablet with a flexible, gooseneck smartphone holder mounted to a table and position it above the AAC device screen. A more sophisticated option would be to use a specialized device called the Adjustable J-Mount. The Adjustable J-Mount is a flexible mount with a webcam that runs from a second computer and is attached to the AAC device mounting plate (Hall & Boisvert, 2014).
Pre-Programmed AAC Device Used During Tele-AAC Assessment
The Adjustable J-Mount also allows the AAC clinician to share their AAC screen. In Erica’s case, we used the Smart Mirror-TV & Device™ app on the iPhone™ (Zengapp Company, 2020) as a document camera (i.e., screen projector) using a desktop mount to view the SLP’s AAC device. When used as a document camera, the Smart Mirror-TV & Device™ app allowed our SLP to project the screen on her laptop and then screen share the AAC device via Zoom™. The additional equipment to view the AAC screen via Zoom™ or other video conferencing platform was critical to the tele-AAC assessment process for both AAC clinicians and caregivers.
The second consideration in tele-AAC service delivery was tele-coaching caregivers and service providers who may be inexperienced in AAC implementation. Our AAC service delivery model shifted from a clinician-led to a caregiver-led approach where our team provided real-time tele-coaching via bug-in-the-ear (BITE) technology to caregivers supporting their child’s communication needs at home. During the tele-AAC assessment process, it was essential for caregivers and service providers to receive coaching and training to facilitate AAC use with the client and provide aided language input and modeling (Hall & Boisvert, 2014). Researchers have demonstrated that parents can learn new AAC strategies and implement them with fidelity (Mandak et al, 2017). Tele-coaching via BITE technology (Ottley, 2016; Snodgrass et al., 2016) is one way to guide caregivers and other service providers in AAC implementation. Through BITE, the caregiver wears Bluetooth™ headphones connected to a smartphone or laptop’s audio allowing our team to provide immediate feedback was necessary to support the caregivers during the assessment successfully (Hall & Boisvert, 2014). We found that implementing AAC in the natural environment (i.e., in the home) increased caregiver engagement and provided a more accessible way for providers to be involved in the AAC process (Biggs et al., 2019).
The third consideration in tele-AAC practices is capitalizing on resources to provide ongoing training support for caregivers and providers. The use of asynchronous supports (e.g., video demonstrations) is a cost-effective way to give caregivers and service providers access to support “anytime, anywhere” (Hall & Boisvert, 2014; Snodgrass et al., 2016). Another option for ongoing training is to leverage support from state AT Act programs funded through the AT Act of 2004. Our partnership with our state AT Act program provided device loans and asynchronous supports for caregivers and providers. We leveraged this partnership to give caregivers access to devices from the state AT program’s lending library. The power of leveraging partnerships through state AT Act programs is an untapped resource available in every single state and territory in the U.S. To find your state or territory AT Act program, visit the National AT Act Technical Assistance and Training (AT3) Center’s website at https://www.at3center.net/stateprogram. Providers seeking to deliver AAC services are encouraged to seek out opportunities to collaborate with their state AT Act programs for device loans, outreach services, and demonstrations. These services are free and offer services to people with disabilities, caregivers, as well as providers.
Anecdotal accounts from caregivers who participated in our tele-AAC model reported having more confidence in device programming and implementing AAC strategies to teach their child how to use the selected AAC system. It is important to note that tele-AAC practices are not a “one size fits all,” and this form of service delivery should be carefully considered if it is appropriate for each individual client (Hall & Boisvert, 2014). In some cases, persons with CNNs and their caregivers may prefer or require face-to-face support. AAC clinicians should consider a hybrid approach that incorporates both face-to-face and tele-AAC services based on the person and caregiver’s preferences and needs (Anderson et al., 2012). Telepractice is already an established practice in many areas of speech and language pathology, and there is strong evidence to support its efficacy. However, more research is needed to evaluate the effectiveness of tele-AAC services.
Conclusion
This paper highlighted how one AT program at a UCEDD swiftly pivoted AAC services to a completely virtual format using HIPAA-compliant video conferencing software, screen sharing options, and tele-coaching via BITE technology. We also leveraged support from our state AT Act program to provide asynchronous supports and resources and ongoing training for caregivers and AAC users. These technology-based solutions and our strategic partnership with our state AT Act program were viable methods for conducting tele-AAC assessment practices in our clinic. These innovative approaches have the potential to revolutionize AAC service delivery and increase access for all. It is important to note, while tele-AAC can be an invaluable resource, some individuals with CCNs and their families may need face-to-face services. Tele-AAC practices have the potential to overcome challenges in AAC service delivery and provide people with CCNs, their caregivers, and the providers that serve them access to expert AAC specialists, real-time feedback, and ongoing support in the natural environment during COVID-19 and beyond.
References
American Speech-Language-Hearing Association. (n.d.a). Augmentative and alternative communication https://www.asha.org/Practice-Portal/Professional-Issues/Augmentative-and-Alternative-Communication/
American Speech-Language-Hearing Association (n.d.b). Telepractice. https://www.asha.org/Practice-Portal/Professional-Issues/Telepractice/
American Speech-Language-Hearing Association. (1970). Code of ethics. https://www.asha.org/policy/ET2016-00342/
Anderson, K., Boisvert, M. K., Doneski-Nicol, J., Gutmann, M. L., Hall, N. C., Morelock, C., Steele, R., & Cohn, E. R. (2012). Tele-AAC resolution. International Journal of Telerehabilitation, 4(2). https://doi.org/10.5195/ijt.2012.6106
Assistive Technology Act of 2004, Pub. L. 108-364.118 Stat. 1707 (2020, November 25). GPO Access database. http://www.gpo.gov/fdsys/pkg/PLAW108publ364/pdf/PLAW-108publ364.pdf
Aydin, O., & Diken, I. H. (2020). Studies comparing augmentative and alternative communication systems (AAC) applications for individuals with autism spectrum disorder: A systematic review and meta-analysis. Education and Training in Autism and Developmental Disabilities, 55(2), 119–144. http://www.daddcec.com/uploads/2/5/2/0/2520220/etadd_june_55_2_2020.pdf#page=6
Baxter, S., Enderby, P., Evans, P., & Judge, S. (2012). Barriers and facilitators to the use of high-technology augmentative and alternative communication devices: A systematic review and qualitative synthesis. International Journal of Language & Communication Disorders, 47(2), 115–129. https://doi.org/10.1111/j.1460-6984.2011.00090.x
Beukelman, D. R., & Mirenda, P. (2013). Augmentative and alternative communication: Supporting children and adults with complex communication needs. Brookes.
Biggs, E. E., Carter, E. W., & Gilson, C. B. (2019). A scoping review of the involvement of children’s communication partners in aided augmentative and alternative communication modeling interventions. American Journal of Speech-Language Pathology, 28(2), 743–758. https://doi.org/10.1044/2018_ajslp-18-0024
Binger, C., Ball, L., Dietz, A., Kent-Walsh, J., Lasker, J., Lund, S., McKelvey, M., & Quach, W. (2012). Personnel roles in the AAC assessment process. Augmentative and Alternative Communication, 28(4), 278-288.
Centers for Disease Control and Prevention. (2018, September 14). Health Insurance Portability and Accountability Act of 1996 (HIPAA). https://www.cdc.gov/phlp/publications/topic/hipaa.html.
Centers for Disease Control and Prevention. (2020, November 29) Coronavirus: COVID-19. https://www.cdc.gov/corona_virus/2019-nCoV/index.html
Curtis, T. R. (2014). Case studies for telepractice in AAC. Perspectives on Augmentative and Alternative Communication, 23(1), 42–54. https://doi.org/10.1044/aac23.1.42
Finke, E. H., Davis, J. M., Benedict, M., Goga, L., Kelly, J., Palumbo, L., Peart, T., & Waters, S. (2017). Effects of a least-to-most prompting procedure on multisymbol message production in children with autism spectrum disorder who use augmentative and alternative communication. American Journal of Speech-Language Pathology, 26(1), 81–98. https://doi.org/10.1044/2016_ajslp-14-0187
Fong, R., Tsai, C. F., & Yiu, O. Y. (2020). The implementation of telepractice in speech language pathology in Hong Kong during the COVID-19 pandemic. Telemedicine and e-Health, 27(1). https://doi.org/10.1089/tmj.2020.0223
Ganz, J. B., Earles-Vollrath, T. L., Heath, A. K., Parker, R. I., Rispoli, M. J., & Duran, J. B. (2012). A meta-analysis of single case research studies on aided augmentative and alternative communication systems with individuals with autism spectrum disorders. Journal of Autism and Developmental Disorders, 42(1), 60–74. https://doi.org/10.1007/s10803-011-1212-2
Grogan-Johnson, S., Schmidt, A. M., Schenker, J., Alvares, R., Rowan, L. E., & Taylor, J. (2013). A comparison of speech sound intervention delivered by telepractice and side-by-side service delivery models. Communication Disorders Quarterly, 34(4), 210–220. https://doi.org/10.1177/1525740113484965
Hall, N., & Boisvert, M. (2014). Clinical aspects related to tele-AAC: A technical report. Perspectives on Augmentative and Alternative Communication, 23(1), 18–33. https://doi.org/10.1044/aac23.1.18
Hall, N., Boisvert, M., Jellison, H., & Andrianopoulos, M. (2014). Language intervention via text-based tele-AAC: A case study comparing on-site and telepractice services. Perspectives on Telepractice, 4(2), 61–70. https://doi.org/10.1044/teles4.2.61
Jackson, D., & Schladant, M. (2017, January). Interdisciplinary assessment and intervention for aided augmentative and alternative communication. Paper presented at the Assistive Technology Industry Association, Orlando, Fl.
Knutsen, J., Wolfe, A., Burke, B. L., Hepburn, S., Lindgren, S., & Coury, D. (2016). A systematic review of telemedicine in autism spectrum disorders. Review Journal of Autism and Developmental Disorders, 3(4), 330–344. https://doi.org/10.1007/s40489-016-0086-9
Light, J., Mcnaughton, D., Beukelman, D., Fager, S. K., Fried-Oken, M., Jakobs, T., & Jakobs, E. (2019). Challenges and opportunities in augmentative and alternative communication: Research and technology development to enhance communication and participation for individuals with complex communication needs. Augmentative and Alternative Communication, 35(1), 1–12. https://doi.org/10.1080/07434618.2018.1556732
Mandak, K., O’Neill, T., Light, J., & Fosco, G. M. (2017). Bridging the gap from values to actions: A family systems framework for family-centered AAC services. Augmentative and Alternative Communication, 33(1), 32–41. https://doi.org/10.1080/07434618.2016.1271453
McNaughton, D., & Light, J. (2015). What we write about when we write about AAC: The past 30 years of research and future directions. Augmentative and Alternative Communication, 31(4), 261–270. https://doi.org/10.3109/07434618.2015.1099736
Morin, K. L., Ganz, J. B., Gregori, E. V., Foster, M. J., Gerow, S. L., Genç-Tosun, D., & Hong, E. R. (2018). A systematic quality review of high-tech AAC interventions as an evidence-based practice. Augmentative and Alternative Communication, 34(2), 104–117. https://doi.org/10.1080/07434618.2018.1458900
Ottley, J. R. (2016). Real-time coaching with bug-in-ear technology: A practical approach to support families in their child’s development. Young Exceptional Children, 19(3), 32-46.
Rehabilitation Engineering Research Center on Augmentative and Alternative Communication, The. (2019). The urgent need for augmentative and alternative communication research, technology development, training, and services to support individuals with complex communication needs: RERC on AAC white paper. https://rerc-aac.psu.edu/wp-content/uploads/2015/08/RERC-on-AAC-2019-White-paper-on-AAC-needs.pdf
Richardson, L., Mccoy, A., & Mcnaughton, D. (2019). “He’s worth the extra work”: The employment experiences of adults with ASD who use augmentative and alternative communication (AAC) as reported by adults with ASD, family members, and employers. Work, 62(2), 205–219. https://doi.org/10.3233/wor-192856
Roberts, M. Y., & Kaiser, A. P. (2011). The effectiveness of parent-implemented language interventions: A meta-analysis. American Journal of Speech-Language Pathology, 20(3), 180–199. https://doi.org/10.1044/1058-0360(2011/10-0055)
Salas-Provance, M. B., Arriola, M. E., & Arrunátegui, P. M. T. (2020). Managing in a crisis: American and Peruvian professionals’ experiences during COVID-19. Perspectives of the ASHA Special Interest Groups, 5(6), 1785-1788. https://doi.org/10.1044/2020_persp-20-00153
Schladant, M., Dowling, M. (2020). Parent perspectives on augmentative and alternative communication in children with fragile x syndrome: It starts in the home. Intellectual and Developmental Disabilities, 58(5), 409-421. https://doi.org/10.1352/1934-9556-58.5.409
Schladant, M., Vega-Velazquez, S., Nevares, A. (in press). The role of the physical therapist in assistive technology service delivery. In C. Miles, M. H. Bloyer, T. Catalino, & E. Shamus, (Eds.), The clinical practice of pediatric physical therapy. Jones and Bartlett Learning Publications.
Snodgrass, M. R., Chung, M. Y., Biller, M. F., Appel, K. E., Meadan, H., & Halle, J. W. (2016). Telepractice in speech-language therapy: The use of online technologies for parent training and coaching. Communication Disorders Quarterly, 38(4), 242–254. https://doi.org/10.1177/1525740116680424
Soto, G., & Yu, B. (2014). Considerations for the provision of services to bilingual children who use augmentative and alternative communication. Augmentative and Alternative Communication, 30(1), 83–92. https://doi.org/10.3109/07434618.2013.878751
Steel, E. J., Gelderblom, G. J., & Witte, L. P. D. (2012). The role of the international classification of functioning, disability, and health and quality criteria for improving assistive technology service delivery in Europe. American Journal of Physical Medicine & Rehabilitation, 91(13), S55-S61. https://doi.org/10.1097/phm.0b013e31823d4ee6
World Health Organization. (2020, March 26). Disability considerations during the COVID-19 outbreak. https://www.who.int/publications/i/item/WHO-2019-nCoV-Disability-2020-1
Zengapp Company. (2020). Smart mirror – TV & device. https://apps.apple.com/us/app/smart-mirror-tv-device/id1484794346

