16 Assessing and Mitigating Risk for Applied Behavior Analysis Providers During a Pandemic
Joshua B. Plavnick PhD; Krista Clancy; and Sharon Milberger
Plavnick, J. B., Clancy, K., & Milberger, S. (2020). Assessing and Mitigating Risk for Applied Behavior Analysis Providers During a Pandemic. Developmental Disabilities Network Journal, 1(2), 210–220. https://digitalcommons.usu.edu/ddnj/vol1/iss2/17/
Assessing and Mitigating Risk for ABA Providers PDF File
Plain Language Summary
The COVID-19 pandemic presented many barriers to delivery of behavioral health services. Applied behavior analysis (ABA) for children with autism spectrum disorder (ASD) is one example. Yet it is important to maintain ABA services for people with ASD to help them achieve long-term life goals. This paper describes a toolkit that helps ABA providers decrease risk during a pandemic. Three providers used the toolkit with 20 children who had ASD. The toolkit helped providers make decisions that maintained safety from COVID-19. The results showed the toolkit can be useful to ABA providers. The toolkit could also be useful in other situations that provide close-contact therapies.
The novel Coronavirus of 2019 (COVID-19) created massive international shutdowns of almost all basic services across many countries in the early stages of 2020, and these shutdowns sporadically continued throughout the year across the globe (Dawood, et al., 2020). The effects of the loss of services varied from inconvenient (e.g., fitness centers and bars) to potentially debilitating (e.g., mental and behavioral health). In situations where loss could be serious, providers required procedures and tools to deliver essential services without placing the consumer or service provider at excessive risk of contracting COVID-19 or suffering severe symptoms if they were to contract the illness. Early stages of the pandemic saw relatively limited direction for safe delivery of essential services, with guidance increasing as it became clear that the U.S. would be navigating peaks and valleys of infections throughout the summer of 2020 and beyond.
One essential service that struggled in the beginning of the pandemic to optimize care was behavioral health treatments for individuals with autism spectrum disorder (ASD; Cox et al., 2020; Columbo et al., 2020). Although many mental and behavioral health providers pivoted to delivery of services via telehealth, such an approach was not always possible as a direct treatment for individuals with ASD (see Cox et al., 2020, and Rodriguez, 2020, for an explanation of telehealth barriers in ASD treatment). In addition, although some children in daycare settings could quickly learn to wear a mask and distance from others, such safety measures may not have been readily understood or feasible for some children with ASD, who often have communication and social skill deficits and who sometimes experience heightened sensitivity to physical stimuli, such as straps around their ears or coverings over their nose and mouths (Kojovic et al., 2019). As such, the ability to maintain safety for both consumers (i.e., the individuals with ASD and family members) and providers, while also delivering effective services, was particularly challenging for treatment of individuals with ASD during the pandemic shutdowns.
The present paper describes a process for assessing and mitigating health risks to individuals with ASD and their families while trying to fulfill behavioral health needs during the COVID-19 pandemic. Although specific to one group of providers and clients, we believe it offers useful guidance to the broader community of behavioral health providers (e.g., occupational therapists, speech and language pathologists, physical therapists) who may be responsible for devising and delivering therapies to individuals with ASD and related developmental disorders during a major public health emergency, such as a pandemic.
Background
Among the most prevalent and empirically supported treatments for ASD are those therapeutic techniques based on the scientific concepts and principles of applied behavior analysis, or ABA (Leaf et al., 2016). It is not uncommon for people with ASD to engage in behavior that can be very challenging for caregivers and service providers, including aggression and self-injury. In addition, these behaviors can be exacerbated by changes in environment and routine (Cohen & Tsiouris, 2020). As the pandemic shutdowns continued, and many consumers experienced restrictions in services in both the schools and community, the importance of consistently delivering ABA to individuals with ASD increased. Therapeutic interventions based on ABA often directly target challenging behaviors and as part of those interventions, behavior analysts provide guidance to families on how to best handle challenging behaviors in the home. These services most often include staff who work directly with the client in their home or clinic, which can also offer much needed respite for families whose other services have been disrupted, reducing additional stressors on families already experiencing higher levels of stress than normal (James, 2012). Although in cases where therapeutic interventions based on ABA were deemed necessary to continue, mechanisms for doing so safely continued to lag, leaving ABA providers guessing about how to safely continue to serve clients and families in need of care.
Among the most important ethical tenets in delivering behavioral health services is “do no harm” (Koocher & Keith-Speigel, 1998), which raises several new considerations during a global pandemic. For example, providers might be concerned that delivering in-person treatment during a pandemic puts clients and families at risk of harm. Such a concern is unlikely when not experiencing a pandemic. In addition, the Behavior Analyst Certification Board (BACB, 2016) outlines conduct of a behavior analyst in the Professional and Ethical Compliance Code for Behavior Analysts to include practicing in areas where they are competent (codes 1.01 and 1.02) and considering their responsibility to their clients and the parties involved with therapy, such as the staff and family who work with that client (2.02, 204). It is also necessary to consider the integrity of the treatment and when services need to be discontinued or interrupted for a period of time (2.09 and 2.15). Within the context of the COVID-19 pandemic, behavior analysts and others who provide services to individuals with ASD and related disorders could benefit from a process for assessing risks at the individual level and making treatment decisions based on that assessment to adhere to professional and ethical standards of care.
Risk assessments are used in considering choices for life, health, finances, and many other situations where it is important to consider options that will provide the best outcome during times of uncertainty (Wilson & Crouch, 2001). Experts in the field of ABA recommend using a decision-making framework to determine the risks and benefits of the situation and determine the best course of action. Bailey and Burch (2016) discuss a process for a risk-benefit analysis that includes (a) assessing the general risk factors, (b) assessing the benefits of treatment, (c) assessing the risks for the procedure, and (d) reconciling the risks with the parties involved. This advice for risk analysis is best when considering if treatment is possible and the types of treatment that should be considered. The process can then be used to objectively review and discuss potential risks and risk mitigation strategies with the client and their family to determine the best choice for each individual client.
Following the widespread shelter-in-place orders that were instituted across the country, Colombo et al. (2020) offered a decision model to determine if ABA services are warranted during a time of crisis. They advised behavior analysts to review the setting, the risk of exacerbating behavioral issues to the point where a client might experience imminent harm or hospitalization, the ability to utilize telehealth services, and the possibility of reducing service intensity for a period of time. In April 2020, the Association of Professional Behavior Analysts (APBA) also offered guidance for ABA practitioners on using ABA during the COVID-19 pandemic that defined terms such as “essential,” reviewed legal responsibilities that behavior analysts should consider and recommended that risk mitigation strategies be used when services are necessary. Unfortunately, the risks associated with COVID-19, along with mitigation strategies to reduce risks, are not “common knowledge” for all behavior analysts. In addition, the risks and mitigation strategies are likely to vary from one service provider to another based on where and how they provide services, as well as for the clients receiving services.
Behavior analysts are trained to consider decisions about safety of the client and others in relation to the need to continue therapy, but it has not been until recent times that a behavior analyst would have to make such decisions during a pandemic. Even those with extensive experience in the field found themselves questioning what the best way was to evaluate the need for treatment in such a novel situation (Cox et al., 2020). Many states across the country issued shelter-in-place orders for its citizens in March of 2020. ABA providers were identified as essential workers, but it was unclear from state to state how that role was defined and how providers should respond with treatment during that time (Cox et al., 2020). Some providers chose to stop services for all clients, some continued services or quickly reopened services and added precautionary measures such as the use of personal protective equipment (PPE) for staff, utilization of health screens, social distancing, and increased sanitization of workspaces and hygiene practices (Kornack, et al., 2020). Local government agencies, the Centers for Disease Control and Prevention (CDC), and other various health and human services agencies produced ongoing new information, making it difficult to competently navigate the information while considering the conflicting responsibilities to the client and other parties involved.
In the current situation, many behavior analysts, including the authors, did not feel like they had the knowledge in disease management or the ability to keep up with the changing information to carry out a competent risk analysis. In response to this challenge, a task force was established through our state’s Leadership Education in Neurodevelopmental and Related Disabilities (LEND) network, with experts in specialty areas including practicing behavior analysts, medical experts in pediatric care and epidemiology, and community and advocacy leaders in ABA and the treatment of ASD. Questions regarding information necessary to conduct a risk analysis were presented to the task force. Each expert gathered supporting documentation in their area of expertise from local and national governmental agencies and published research. The information collected and discussed included the most up-to-date recommendations for safety measures for direct care workers from a variety of areas (medicine, childcare, etc.; CDC, 2020; Michigan Department of Health and Human Services, 2020), recently published articles on COVID-19 (health risks for different populations, comorbid disease-related health concerns, and the populations most at risk; Ludvigsson, 2020; Mullen et al., 2020), and governmental websites with daily and weekly data regarding cases, hospitalizations, and deaths related to COVID-19 (Michigan.gov, 2020a, 2020b; Mi Safe Start Map, 2020; Whitmer, 2020).
The product developed by the task force was a toolkit that behavior analysts could use to assess individual client risk and devise corresponding risk mitigation strategies to increase the likelihood of maintaining client and staff safety while delivering behavioral health services to clients (see Clancy et al., 2020). Although specific to behavior analysts, the toolkit was informed by and modeled after a similar resource from the Johns Hopkins Bloomberg School of Public Health (Mullen et al., 2020), which was intended for the broader business community in its return to operations during COVID-19. The task force adapted this broader resource to meet the specific needs of ABA providers and children with ASD. At minimum, we believe our toolkit (i.e., Clancy et al., 2020) could be adapted for use across many behavioral health providers, and likely also has applicability in educational and recreational settings where individuals with intellectual and developmental disabilities (I/DD) may receive services. The following case study describes our first use of the toolkit for a behavioral health center and discusses the broader implications of this work.
Method
Based on discussions from a series of meetings, the task force developed a toolkit to provide support for behavior analysts in the field to gain knowledge about COVID-19, the necessary background information providers needed to gather about the client and their family, and the unique aspects of the therapeutic environment and the community that influenced risk (Clancy et al., 2020). This knowledge could then be used to complete a risk assessment for each individual client. The toolkit also included extensive considerations for risk mitigation across a range of service options for clients. Together, the risk assessment and risk mitigation options provided the information necessary for a behavior analyst to feel competent in using a decision-making framework similar to what is recommended for complex situations the professionals are likely to encounter.
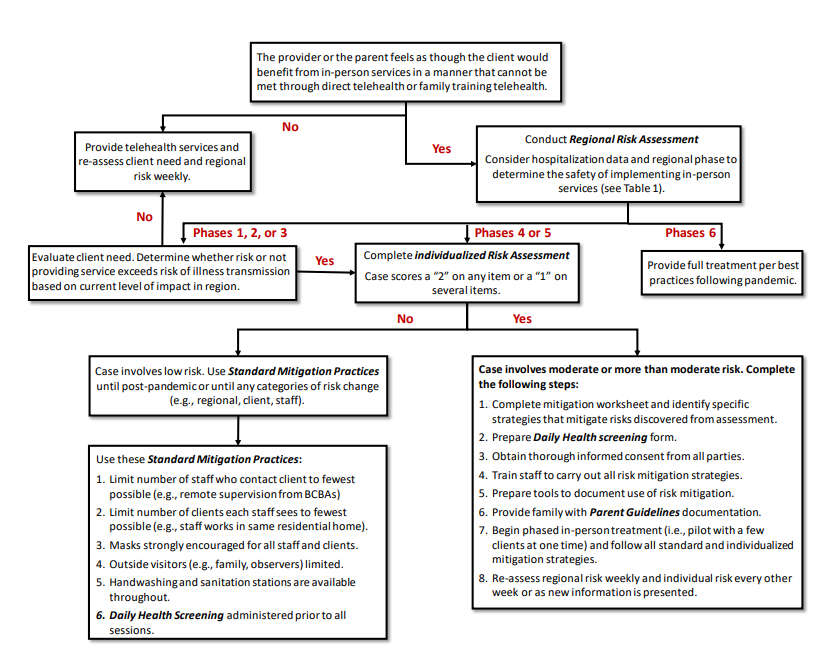
The toolkit, titled “Risk Assessment and Mitigation Strategies for Applied Behavior Analysis: Treatment of Children with Autism During a Pandemic” (Clancy et al., 2020), is divided into two sections (see Table 1). The first section focuses on risk assessment and includes an Individualized Risk Assessment tool that requires the behavior analyst review several aspects of service delivery and assign to specific items a ranking of minimal, moderate, or more than moderate risk, to make decisions about the overall exposure to COVID-19 as well as a client’s risk of a severe COVID-19 infection. Assessment questions targeting the therapeutic environment include the size and number of people in the therapeutic space, the ability for the staff to keep the area disinfected, the ability to keep others out of the treatment area, and access to handwashing in the treatment area. Assessment questions targeting the individual and their family include health questions about pre-existing conditions, age of the client and family members, behaviors that could increase the risk of contamination (e.g., pica, mouthing, eye poking, nose picking), the ability of the client and family to maintain social distance from staff, and the ability for an alternative caregiver to care for the client if the current caregivers were to become ill. There are also questions targeting the staff including age of the staff, comorbid medical conditions, possibility of exposure to COVID-19 outside of work, and the risk of contamination from working with a client with increased contamination behaviors, as discussed above. The risk assessment tool also has an example of a health screen that can be used by the behavior analyst to monitor symptoms in clients, family, and staff, and a flow chart used to guide the behavior analyst in the decision model if they identify items that increase risk on the assessment tool.
| Section | Description | Purpose |
|---|---|---|
| 1. Individualized risk assessment | Assesses risk pertaining to 3 areas: • Treatment environment • Client and family • Staff members |
Allows behavior analyst to identify greatest risk factors for spread of illness or severe response if infected. |
| 2. Health screen | Assess daily health condition of staff, client, and client family if needed. | Make decisions about need for daily cancellation due to report of illness. Must be adapted regularly to align with health guidelines. |
| 3. Mitigation strategies worksheet | List of potential mitigation actions at organization or individual level. | Takes outcomes from assessment and guides provider to optimize mitigation strategies. |
| 4. Parent planning guidelines | Considerations for providers to discuss with parents. | Assists in revising treatment plan to account for health risks. |
The second section of the toolkit focuses on mitigation strategies and includes an individualized Mitigation Strategy Worksheet that provides strategies related to physical distancing between persons and objects, health screenings, sanitation and hygiene measures, agency policy, and communication between the agency and staff as well as between the agency and families (Clancy et al., 2020). These strategies, although not all encompassing, are a summary of many of the risk mitigation strategies compiled in the task force discussions and the documents collected during the task force workgroup. Collecting these strategies into a single toolkit allows providers to complete an assessment and mitigation plan for each client, discuss critical operating procedures with each member of the staff team, coordinate planning and logistics with the client and family, and embed implementation guidelines within a client’s treatment plan. Figure 1 is part of the toolkit and depicts a process that providers can use to guide decision making as information is collected using the various assessments within the toolkit.
A Sequence for Administering Assessment Tools and Aligning to Individual Risk Mitigation Strategies
When possible, it is important to involve the client in the planning process. When not possible, the family must be involved to ensure a balance between client or family needs, effective treatment, and overall safety. Also included in the toolkit (Clancy et al., 2020) is a set of parent planning guidelines for the behavior analyst to use with the family or to provide to the family prior to completing the risk assessment with them. This tool helps to educate the parent on the risks of COVID-19 and the expectations and considerations that are made in determining if and how treatment should be continued during this time.
At its inception, the Clancy et al. (2020) toolkit was a collection of resources and practice guidelines the authors believed would be beneficial to providers and families alike. In the time since, a preliminary evaluation of the toolkit was conducted to determine the feasibility of providers utilizing the various components and deriving modified treatment plans as a result. During this pilot evaluation, we sought to evaluate whether the toolkit effectively assessed risk for individual clients and families, as well as risk of behavior technicians in delivering ABA services. In addition, the feasibility of Board-Certified Behavior Analysts (BCBAs) to use the toolkit to develop individualized risk mitigation plans for each client was also evaluated.
The toolkit was piloted following the shutdown—at a time when services for those involved had been temporarily suspended and the providers were working toward restarting ABA services within clients’ homes. In order to pilot the toolkit, three BCBAs completed the risk assessment and developed corresponding mitigation strategies for 23 children with ASD. All BCBAs were employed with the same organization, which delivered early intensive intervention based on the principles of ABA to children between 2 and 6 years of age. Each of the providers had a master’s degree and had been working as a BCBA for at least 3 years.
Each of the families for whom an assessment and mitigation plan were developed had received services within a clinic setting prior to the COVID-19 pandemic. When the pandemic began, in-person services were paused, and telehealth was administered when possible. Prior to relaunching in-person services, the organization made the decision to administer in-home services only, as the clinic setting in which services had been provided did not allow for appropriate social distancing. Therefore, the risk assessment and mitigation strategies had to be aligned to each families’ unique home environment. Some families had multiple generations living within a single home, with home size ranging from quite small (e.g., one-bedroom apartments) to large (e.g., 3,000 square feet or more).
The BCBAs all completed the same risk assessment toolkit described above. Each BCBA completed all items on the toolkit for each client, assigning a rating of minimal, moderate, or more than moderate for each item. The BCBAs had served all participating clients for at least 6 months prior to the start of the pandemic. For any items the BCBA could not answer on the assessment, they contacted parents of the child to derive a risk rating of low, medium, or high for that item. Once each of the items on the risk assessment had been scored (minimal = 1, moderate = 2, more than moderate = 3), the BCBAs calculated overall risk scores by adding each of the rankings together and dividing the sum by the total possible score to derive a percentage. Although some items may involve greater risk than others, a weighted analysis was beyond the scope of this preliminary evaluation. Instead, the purpose of the overall score was to derive a general profile of the risk each client, family, and the behavior technicians, may face in delivering services. Higher risk scores were interpreted to mean more precautions and possibly resources were needed, though each item with a moderate risk score was addressed with a corresponding risk mitigation strategy. Risk scores were not used to make decisions about pausing services. All clients continued to receive services unless the family opted out of treatment.
Results
After administering the risk assessment across 23 families, BCBAs identified a mean risk score of 36.4%, with a range from 13% to 59%. The sample involved in this pilot evaluation demonstrated relatively low overall risk, with some clients and families having very low risk and others demonstrating moderate risk. In what follows, we discuss the use of system-wide mitigation strategies that can contribute to overall reduction of risk for all clients, as well as the importance of individualized mitigation strategies to support health and safety of each client, family, and staff member in the delivery of behavioral services during a pandemic.
Although the sample mean was relatively low, it should be noted that the service provider had already eliminated one major element of risk in that services within the same treatment room had been stopped in favor of delivering treatment within each clients’ home environment. This strategy exemplifies a system-level mitigation effort that was optimal for this specific agency because of spacing issues within the clinic. Although the types of systemic mitigation approaches will vary from agency to agency, providers will likely benefit from incorporating some system-wide mitigation strategies, regardless of assessed risk levels. Similar systemic risk mitigation efforts in the present investigation involved conducting health screenings with all staff, clients, and family members prior to beginning a treatment session, and requiring masks for all staff and families while teaching clients to tolerate wearing a mask as often as possible during treatment sessions. Finally, though the assessment may have deemed clients at a low risk for either contracting or having a severe outcome from COVID-19, this is different than identifying no risk, as in a post-pandemic environment. Thus, developing individualized risk-mitigation strategies can be useful even when overall risk starts at a low level.
The variation of risk scores across clients and families with some very low scores to some moderate risk scores speaks to the importance of an individualized assessment followed by mitigation strategies at the level of individual clients, families, and staff members. For example, one common approach when delivering ABA services within a client’s home in the absence of a pandemic is to provide at least two different behavior technicians (one at a time during different times of the day) to promote multiple social partners and interactions. In addition, a BCBA will supervise within the home once per week to review program implementation and adjust as needed. However, in situations where clients had higher risk scores, one mitigation strategy used was to reduce the total number of people who entered the home. This was accomplished by only pairing one behavior technician with each client and the BCBA conducting supervision sessions via videoconferencing.
Conclusion
The toolkit developed by Clancy et al. (2020) was a useful way for the individual providers and organization to make decisions about delivery of treatment to clients and families during the COVID-19 pandemic. Individual risk factor scores indicated some clients presented greater risk than others. Calculating those scores allowed for a decision-making process that ensured resources were allocated toward clients and families, or staff members with higher risk scores. The authors of this paper believe all clients who consent to treatment should receive services during a pandemic or similar situation, and strongly caution against using risk scores as a mechanism for allocating treatment to some clients and not others. Instead, risk scores should be used to inform the level of support needed for all clients.
The strategies described in this paper were developed for Michigan ABA providers treating children with ASD during the COVID-19 pandemic, though they were based on risk mitigation procedures from a general return-to-work document written by public health officials at Johns Hopkins University (Mullen et al., 2020). Therefore, these strategies can easily be applied to several other contexts including non-ABA providers, children with disabilities other than ASD, use outside of Michigan, and use with adults as well as children. Moreover, the strategies have potential to be extended beyond the COVID-19 pandemic to address future public health emergencies, and possibly to other barriers to in-person service provision, as well as client and family preferences.
The flowchart shown in Figure 1 can serve as a reasonable framework for many behavioral health providers. The language used in the flowchart is nonspecific to any particular provider or type of disability with one minor exception (an example is given to “use remote supervision from BCBAs” as a mitigation practice to limit the number of staff who come in contact with the client). Similarly, the Individualized Risk Assessment and Daily Health Screening Tool are written in a manner that can be used by any provider serving clients in a behavioral health setting. The Risk Mitigation Worksheet does make a few references to behavior analysts and behavior technicians, but these terms could easily be substituted with more general words such as “provider” or discipline-specific terminology. In order to make the tools applicable to adult clients, items may need to be revised in a manner that asks the individual to answer on behalf of themselves (or have an option to have the person be supported in answering the questions).
The Parent Guidelines are geared to ABA services and would need modification for other behavioral and nonbehavioral services. The guidelines provided could serve as a template from which to work. These guidelines could also be modified for any family member including those who support an adult with a disability.
Although the strategies focus on our state’s Safe Start Plan, which delineates six phases (Phase 1 indicating extreme caution and Phase 6 referring to post-pandemic), they could be applicable to other states. More specifically, the portion of the flowchart following Conduct Regional Assessment can be adapted to refer to state-specified risk levels rather than being organized by phase. Each provider should abide by their particular state’s public health requirements.
The strategies identified in this report can be readily used if there is a resurgence of COVID-19 or another pandemic emerges. In addition, the toolkit may be of use when not in a pandemic, as risks to health and safety of consumers are applicable anytime behavioral health providers administer services to individuals with disabilities or mental health disorders. Future research could assess the benefit of using the tools described herein when not in a pandemic and determine whether risk assessments and mitigation strategies decrease general spread of illness or injury during service delivery. COVID-19 led to many innovations that will be essential to incorporate across a range of business and service-delivery entities. The toolkit described herein offers a potential solution to a number of challenges that could arise in the delivery of behavioral health services.
References
Bailey, J. S., & Burch, M. R. (2016). Ethics for behavior analysts (3rd ed). Routledge.
Behavior Analyst Certification Board. (2016). Professional and ethical compliance code for behavior analysts. Littleton, CO: Author.
Centers for Disease Control and Prevention. (2020). COVID-19 one-stop shop toolkits. https://www.cdc.gov/coronavirus/2019-ncov/communication/toolkits/index.html
Clancy, K., Plavnick, J., Allen, C., Capuano, A., Daar, J., English, K., Fuqua, W., Milberger, S., Schrum, S., & Turner, J. (2020). Risk assessment and mitigation strategies for applied behavior analysis: Treatment of children with autism during a pandemic. https://ddi.wayne.edu/covid19/aba_risk_management_document_revised_and_disseminated_july_2020.pdf
Cohen, I. L., & Tsiouris, J. A. (2020). Triggers of aggressive behaviors in intellectual disabled adults and their association with autism, medical conditions, psychiatric disorders, age and sex: A large-scale study. Journal of Autism and Developmental Disorders, 50, 3748-3762.
Colombo, R. A., Wallace, M., & Taylor, R. (2020). An essential service decision model for ABA providers during crisis. Behavior Analysis in Practice, 13, 306–311. http://doi.org/10.1007/s40617-020-00432-z
Cox, D. J., Plavnick, J. B., & Brodhead, M. T. (2020). A proposed process for risk mitigation during the COVID-19 pandemic. Behavior Analysis in Practice, 13, 299-305. http://doi.org/10.1007/s40617-020-00430-1
Dawood, F. S., Ricks, P., Nijie, G. J., Doughtery, M., Davis, W., Fuller, J. A., Winstead, A., McCarron, M., Scott, L. C., Chen, D, Blain, A. E., Moolenaar, R., Li, C., Popoola, A., Jones, C., Anantharam, P., Olson, N., Marston, B. J., & Bennett, S. D. (2020). Observations of the global epidemiology of COVID-19 from the prepandemic period using web-based surveillance: A cross sectional analysis. The Lancet, 20, 1256-1262. https://doi.org/10.1016/S1473-3099(20)30581-8
James, N. (2012). The formal support experiences of family carers of people with an intellectual disability who also display challenging behaviour and/or mental health issues: What do carers say? Journal of Intellectual Disabilities, 17(1), 6-23. http://doi.org/10.1177/1744629512472610
Kojovic, N., Ben Hadid, L., Franchini, M., & Schaer, M. (2019). Sensory processing issues and their association with social difficulties in children with autism spectrum disorders. Journal of Clinical Medicine, 8, 1508-1524. https://doi.org/10.3390/jcm8101508
Koocher, G. P., & Keith-Spiegel, P. (1998). Ethics in psychology (2nd ed). Oxford University Press
Kornack, J., Williams, A. L., Johnson, K. A., & Mendes, E. M. (2020). Reopening the doors to center-based ABA services: Clinical and safety protocols during COVID-19. Behavior Analysis in Practice, 13, 543-549. http://doi.org/10.1007/s40617-020-00462-7
Leaf, J. B., Leaf, R., McEachin, J., Taubman, M., Ala’i-Rosales, S., Ross, R. K., Smith, T., & Weiss, M. J. (2016). Applied behavior analysis is a science and, therefore, progressive. Journal of Autism and Developmental Disorders, 46, 720-731. doi: 10.1007/s10803-015-2591-6
Ludvigsson, J. F. (2020). Children are unlikely to be the main drivers of the COVID-19 pandemic: A systematic review. Acta Paediatrica. https://doi.org/10.1111/apa.15371
Michigan Department of Health and Human Services, Behavioral Health and Developmental Disabilities Administration. (2020). Guidance for specific clinical essential face to face encounters in behavioral health clinics, substance use services and residential settings in the COVID-19 context. https://www.michigan.gov/documents/mdhhs/BH_Communication_Essential_Virtual_and_F2F_Services_COVID-19_Guidance_20-11_695961_7.pdf
Michigan.gov. (2020a). Coronavirus statewide available PPE and bed tracking. https://www.michigan.gov/coronavirus/0,9753,7-406-98159-523641–,00.html
Michigan.gov. (2020b). Coronavirus Michigan data. https://www.michigan.gov/coronavirus/0,9753,7-406-98163_98173—,00.html
MI Safe Start Map. (2020). Dashboard. https://www.mistartmap.info/
Mullen, L., Kobokovich, A., Trotochaud, M., Sell, T. K., Rivers, C., Martin, E., Cicero, A., Inglesby, T., & Watson, C. (2020). Operational toolkit for businesses considering reopening or expanding operations in COVID-19. Baltimore, MD: Center for Health Security, Johns Hopkins Bloomberg School of Public Health
Rodriguez, K. A. (2020). Maintaining treatment integrity in the face of crisis: A treatment selection model for transitioning direct ABA services to telehealth. Behavior Analysis in Practice, 13(2), 291-298. https://doi.org/10.1007/s40617-020-00429-8
Wilson, R., & Crouch, E. A. C. (2001). Risk-benefit analysis. Harvard University Press
Whitmer, G. (2020). MI Safe Start: A plan to re-engage Michigan’s economy. https://www.michigan.gov/documents/whitmer/MI_SAFE_START_PLAN_689875_7.pdf

