Spencer Fox Eccles School of Medicine
48 Disparities in Delivery of Hypofractionated Radiotherapy in Underserved Populations
Joshua Sokeye; Brock O'Neil; Nicole Murray; Joshua Horns; Jonathan Chipman; and Gita Suneja
Faculty Mentor: Brock O’Neil (Surgery, University of Utah)
Background
Cancer is the second leading cause of mortality in the United States and it is estimated that 50% of all people diagnosed with cancer require radiotherapy as part of their treatment (1, 2). A conventional course of radiotherapy, delivered through individual doses called fractions, could take up to 8 weeks to deliver in full (3). Shorter radiation courses, or hypofractionation, use larger doses per fraction, reducing the overall duration of a radiotherapy course (4). In this study, we investigate whether there are currently disparities in hypofractionation delivery to underserved populations that would influence withholding novel payment policies catered to supporting these patients. We hypothesize that cancer patients from racially and ethnically minoritized, rural, and low socioeconomic backgrounds are less likely to receive hypofractionated radiotherapy than other populations.
Methods
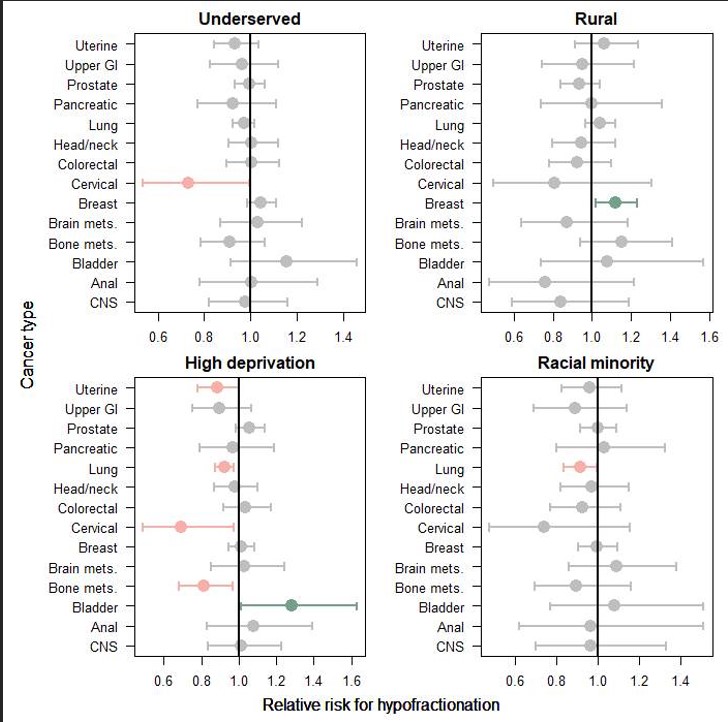
The Centers for Medicare and Medicaid Services (CMS) claims data from 2016-2018 was used for patients treated with radiotherapy for any of 14 cancers included in a proposed novel payment model, the Radiation Oncology Model. Data on radiation fractions was collected from the first round of radiation and stopped at a break in radiation fractions for more than 14 days. Models were then created from the 14 cancer types we analyzed over 4 exposure levels. The results were displayed on a 4-panel forest plot to analyze the likelihood of hypofractionation delivery.
Results
We found that minority and low socioeconomic status (SES) patients were just as likely to receive hypofractionated radiotherapy across most cancer types, compared to high socioeconomic status patients. Looking at specific cancers and underserved groups more closely demonstrates that rural breast cancer patients are more likely to undergo hypofractionation. For patients in high-deprivation areas, uterine, lung, cervical, and bone mets cancer patients are less likely to receive hypofractionation while bladder is more likely. Racial/ethnic minoritized lung cancer patients are also less likely to receive hypofractionation.
Discussion
Overall, the results for all of the cancer types except cervical suggest that hypofractionation is just as likely to be prescribed to underserved patients, but with some important exceptions in which underserved patients – especially those from low-resource areas – are less likely to receive shorter course radiation. These findings suggest an urgent need for value-based payment models like the Radiation Oncology Model, which incentivizes hypofractionation. Limitations of the study were that the study had a retrospective nature with a focus on the data and models occurring before 2018. Future studies should look into the potential faults in the current fee-for-service (FFS) payment model.
Footnotes
- Prevention. CfDCa. National Center for Health Statistics: Cancer deaths.: U.S. Department for Health and Human Services. .
- Abdel-Wahab M, Gondhowiardjo SS, Rosa AA, Lievens Y, El-Haj N, Polo Rubio JA, et al. Global Radiotherapy: Current Status and Future Directions-White Paper. JCO Glob Oncol. 2021;7:827-42. doi: 10.1200/go.21.00029. PubMed PMID: 34101482; PubMed Central PMCID: PMC8457786.
- Allen C, Her S, Jaffray DA. Radiotherapy for Cancer: Present and Future. Adv Drug Deliv Rev. 2017;109:1-2. doi: 10.1016/j.addr.2017.01.004. PubMed PMID: 28189183.
- Santos A, Penfold S, Gorayski P, Le H. The Role of Hypofractionation in Proton Therapy. Cancers (Basel). 2022;14(9). Epub 20220502. doi: 10.3390/cancers14092271. PubMed PMID: 35565400; PubMed Central PMCID: PMC9104796.
Media Attributions
- 137489262_range_joshsokeye_figure

