College of Social and Behavioral Science
92 Air Pollution and Cardiometabolic Diseases: Differences by Occupational Group
Bibiana Rodriguez Vega; David Curtis; Ethan Cheung; Susan Walker; and Mari Takano Okubo
Faculty Mentor: David Curtis (Family & Consumer Studies, University of Utah)
Introduction and Literature Review
Air pollution exposure represents a significant, environmental hazard in the U.S., detrimental in daily life and health, but often overlooked. Exposure to air pollution has been associated with increased risk of cardiovascular diseases (CVD) (Brook et al., 2010), metabolic diseases (Ning et al., 2021), and respiratory diseases (Xing et al. 2016). However, not all people are affected to the same degree by air pollution, because of both differential exposure and susceptibility. For instance, fetuses and young children, elderly people, or persons with pre-existing health conditions (e.g. allergies, pulmonary and heart diseases) are at higher risk of being harmed by air pollution due to physiological susceptibility (Makri & Stilianakis, 2008; Peled, 2011). Additionally, socio-economically disadvantaged people are more vulnerable to pollution-related health risks, potentially due to a combination of pre-existing conditions (Makri & Stilianakis, 2008), limited resources, education, access to services and infrastructure, or living and working conditions (Peled, 2011). For example, commuting or residing in places with high pollution levels, time spent outdoors, or working conditions (Makri & Stilianakis, 2008), are often correlated with socio-economic status (SES).
There is an established link between air pollution and adverse effects on individuals’ health, but there is a lack of research on occupational differences in how air pollution is related to disease outcomes. Previous research has focused on the negative effects of occupational exposure to air pollution (risks to a mix of agents, e.g., physical, chemical, or biological) on health outcomes. Most studies have focused on particulate matter and pollutant concentrations within occupational settings (Fang et al., 2010). Studies indicate that occupational exposure increases the risk of incidence and exasperation of CVD and respiratory diseases (Fang et al., 2010; Nishida & Yatera, 2022). Also, there is an adverse association between both SES characteristics (e.g., income, occupation, and education) and respiratory diseases (Zhang et al., 2021; Sidorchuk et al., 2009; Mao et al., 2001).
Occupational differences in air pollution-related health risks may exist because of differences in job strain, work environment exposure, and occupational status. Individually, each of these factors affect mortality (Matthews et al., 2023; Gonzalez-Mulé & Cockburn, 2021; Christ et al., 2012). Job characteristics can act as a buffer on the positive relationship between job strain and mortality. For example, high job control indicates better physical health even with high job demands (Gonzalez-Mulé & Cockburn, 2021). However, not much is known about occupational differences based on ambient air pollution exposure.
The central aim of this study is to examine how occupation moderates the relationship between air pollution exposure and cardiometabolic (CMB) and respiratory disease outcomes, based on differential exposure or susceptibility to ambient fine particulate matter (PM2.5). Also, this study will examine job characteristics (i.e., job strain, environmental exposure at the workplace, occupational status) that may act as moderators, potentially explaining differential disease outcomes from air pollution exposure across occupational groups.
Materials and Methods
Data and Study Population
We used data from Waves 2 and 3 of the Midlife in the United States (MIDUS) study which is a national study that focuses on health and aging processes among US adults during midlife. The first wave of data collection took place in 1995-96, with follow-ups in 2004-05 (Wave 2; M2) and 2013-14 (Wave 3; M3). The MIDUS study includes a random national sample, oversamples in metropolitan areas, siblings of the random sample, a twin sample, and Black/African Americans from Milwaukee (MKE). We restricted the sample to adults younger than age 65 who were employed at M2. For the current study, sample sizes were 2,338 and 1,683 adults when predicting prevalence and incidence, respectively.
Measures
Two outcomes were measured in this study: cardiometabolic and respiratory diseases. Cardiometabolic (CMB) disease was assessed using a summary score of four health indicators: high blood pressure/hypertension, heart trouble, diabetes/high blood sugar, central adiposity. Participants were asked if they had received medical diagnosis or treatment for hypertension and diabetes in the past 12 months. For heart trouble, participants were asked if heart trouble was suspected or confirmed by doctors. Central adiposity was determined by waist circumference, with cutoffs of ≥102cm for males and ≥88 cm for females. Central adiposity is also a more reliable predictor of cardiometabolic disease and mortality compared to general obesity (Ashwell et al., 2012). We standardized these four indicators and calculated the average to create a summary measure of CMB disease. For respiratory disease, participants self-reported if they had experienced or received treatment for lung conditions in the past 12 months: asthma, bronchitis, and emphysema. If participants experienced any of the conditions, they were categorized to have respiratory disease.
PM2.5 air pollution was measured by the annual concentration of fine particulate matter of 2.5 µg/m3 in diameter at the census tract level. We used estimates from the Center for Air, Climate, and Energy Solutions v1 empirical models, which are based on US EPA monitoring sites and air quality monitoring networks. The modeled values were calculated using land use variables and satellite-derived estimates (Kim et al., 2020). We included 5-year averages of PM2.5 air pollution for 2001-05 to predict M2 outcomes, and 2006-10 to predict change in outcomes between M2 and M3.
To assess major occupational group, we used participant-reported current occupation at M2 and M3. Occupation was classified using the 1990 US Census Standard Occupational Classification for M2 (Holman & Hughes, 2021; Scopp, 2003). The occupation classification initially included executive, administrative, and managerial; professional specialty; technician and related support; sales occupation; administrative support including clerical; service occupation; farming, forestry, and fishing; precision production, crafts, and repair; operator, laborer, and military categories. We then grouped these classifications into five categories of interest based on common characteristics: 1) managerial and professional, 2) administration, 3) sales, 4) service work, 5) manual occupations.
To assess major occupational group, we used participant-reported current occupation at M2 and M3. Occupation was classified using the 1990 US Census Standard Occupational Classification for M2 (Holman & Hughes, 2021; Scopp, 2003). The occupation classification initially included executive, administrative, and managerial; professional specialty; technician and related support; sales occupation; administrative support including clerical; service occupation; farming, forestry, and fishing; precision production, crafts, and repair; operator, laborer, and military categories. We then grouped these classifications into five categories of interest based on common characteristics: 1) managerial and professional, 2) administration, 3) sales, 4) service work, 5) manual occupations.
For individual-level control variables, we included the following factors related to CMB and respiratory diseases: age (in year), biological sex (male, female), race (non-Hispanic White, nonHispanic Black, Hispanic, non-Hispanic native Americans, non-Hispanic others), MIDUS sampling types (random digit dialing, sibling, twin, city oversample, Milwaukee [MKE]), marital status (married, separated/divorced, widowed, never married), and current smoking status. We also included three area-level control variables in approximately 2010: tract walkability (compactness composite index), tract median household income (derived from 5-year estimate from 2006-10 American Community Survey), and urban-rural classification (city, suburb, town, rural).
Analysis
Linear regression and linear probability modeling were applied to assess the impact of PM2.5 air pollution on prevalent and incident CMB and respiratory disease, respectively. To assess the moderation of occupational groups in the associations, we created an interaction term to test how the impact of PM2.5 air pollution on each outcome varied by occupational groups. Next, to test underlying process variables, interaction terms by PM2.5 air pollution with job strain, occupational status, and outdoor work environment were added. Standard errors were adjusted to account for clustering in census tracts.
Results
The average age of the sample at M2 was 49 years old (SD = 7.90) with a range of 30-64 years old. The sample was 52.6% female, 71.4% were married (15.5% separated/divorced, 2.0% widowed, 11.1% never married), and 53.46% were non-smokers. Table 1 shows that participants across occupational groups had similar exposure to PM2.5 air pollution. Rates of CMB disease and respiratory disease appeared to vary across occupational groups, with the lowest rate among professional occupations at both waves while prevalent respiratory disease was highest for participants in service occupations at M2 and those in sales occupations at M3. 33% of participants with administrative occupation experienced job strain, while those in professional occupation had, on average, higher occupational status. Also, participants with manual occupation spent more time in outdoor work environment (mean = 2.81).
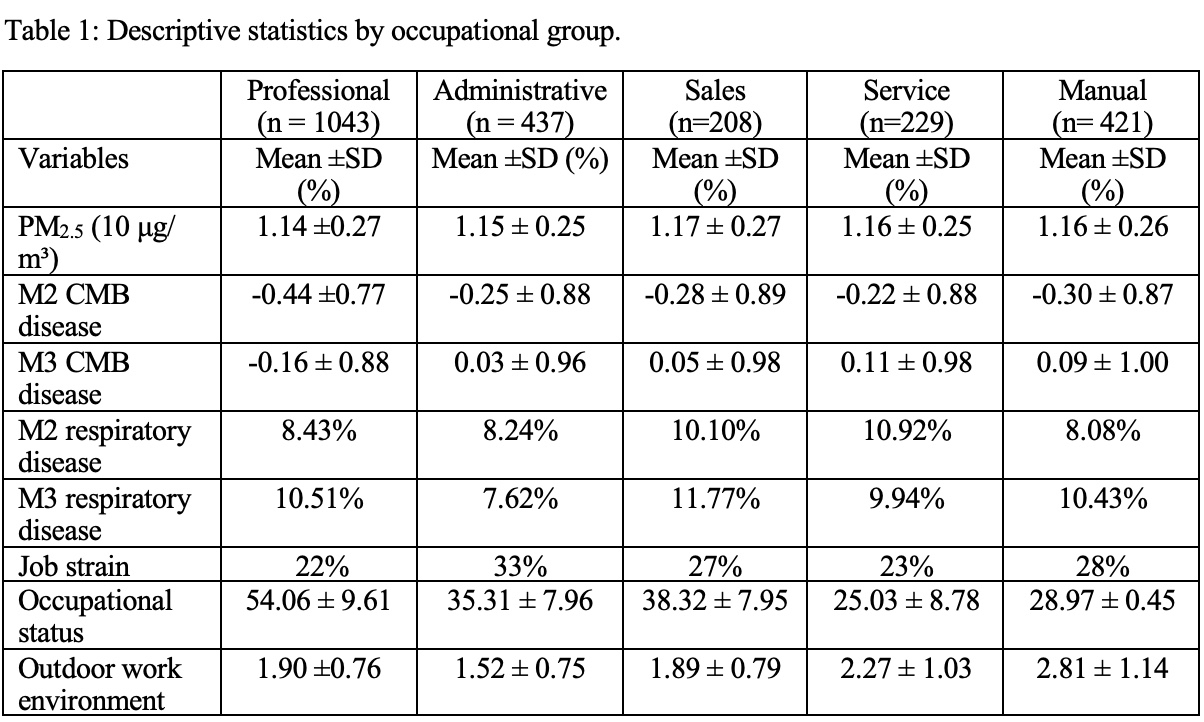
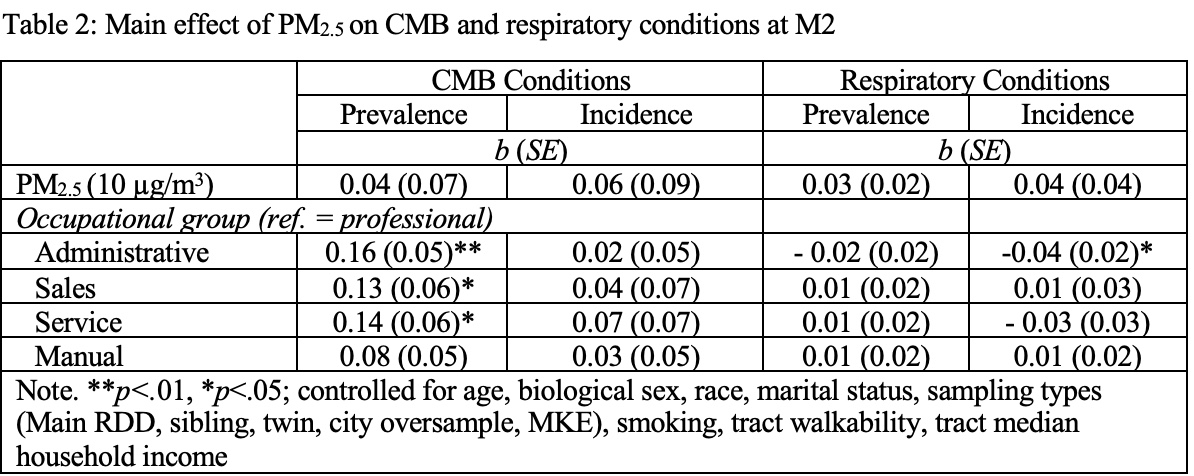
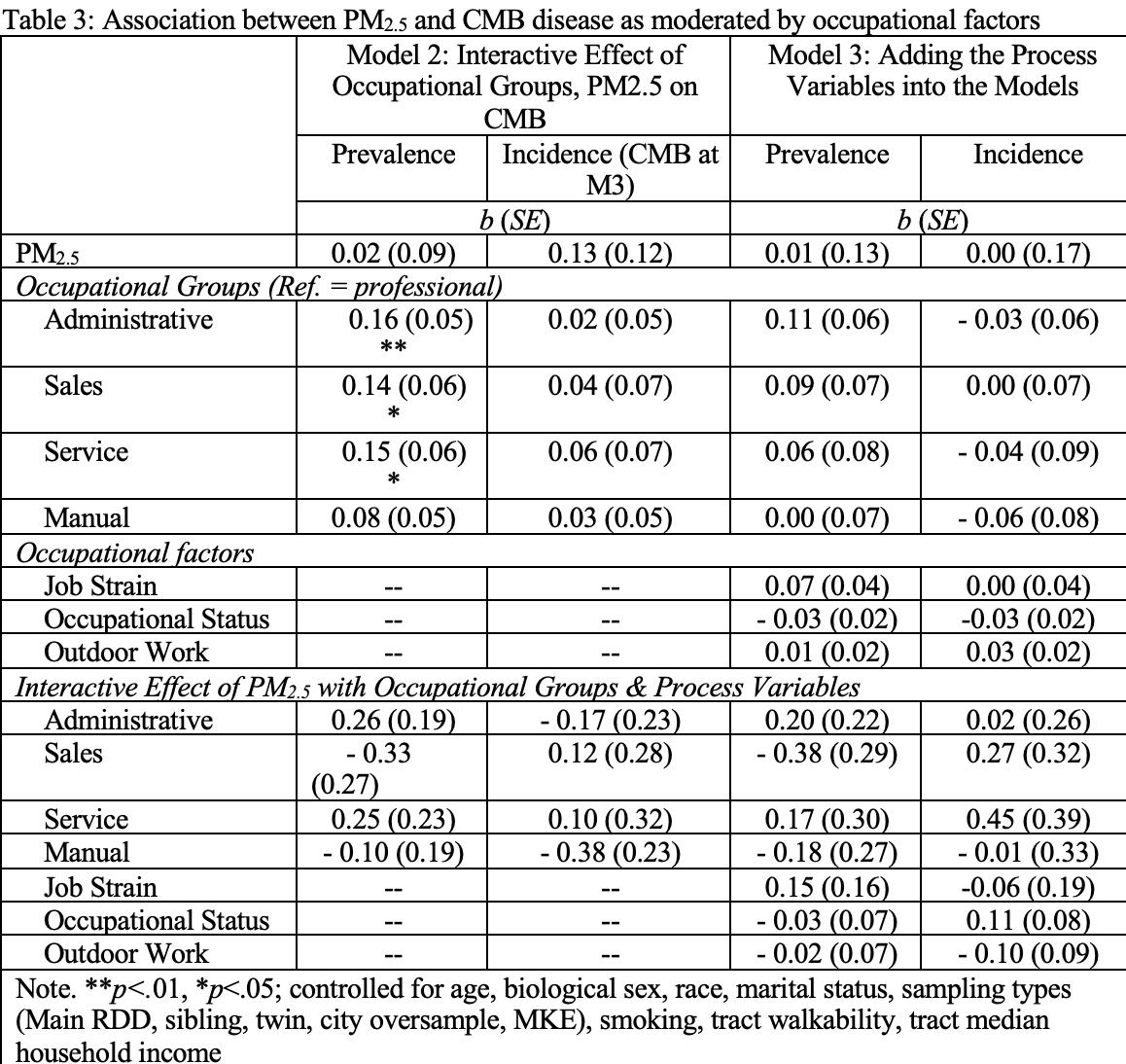
Table 3 shows the associations between PM2.5 air pollution and CMB disease and how it varied by occupational groups and the process factors (job strain, occupational status, outdoor work environment). In Model 2, we found that PM2.5 air pollution did not predict CMB prevalence and incidence. Relative to professional occupational group, participants in administrative, sales, and service occupations likely had higher CMB prevalence. On the other hand, no occupational differences were found for CMB incidence. In addition, as shown in Model 3, occupational factors did not act as moderators for the prevalence and incidence of CMB disease.
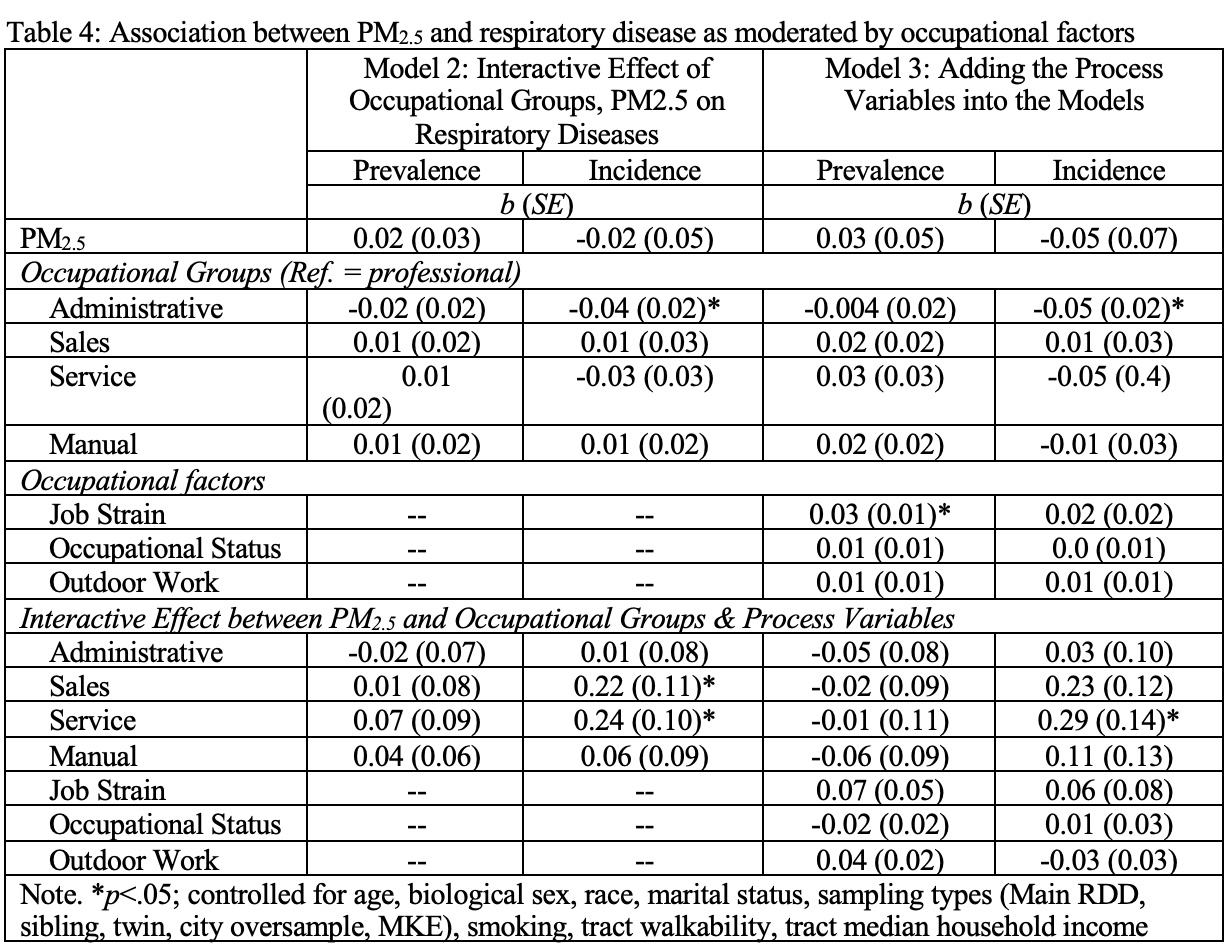
As for respiratory disease, PM2.5 air pollution was not a predictor of respiratory disease prevalence and incidence, as shown in Table 4. In terms of occupational difference in Model 2, the only group with a significant difference relative to professional occupations was the administrative group when predicting incidence respiratory diseases. Specifically, compared to professional occupation, participants in administrative occupation likely have 4-percentage-point lower in the risk of incident respiratory disease. We also found two interactive effects by PM2.5 air pollution with sales and service occupational groups. Relative to the professional occupational group, participants in sales and service occupations likely have higher incident respiratory disease. No interactive effect was found for the prevalent models. According to Model 3, job strain was the only process variable that predicted prevalent respiratory disease. Job strain was associated with an increase in respiratory disease prevalence, but not when interacting with PM2.5 air pollution. The other process variables did not have a significant effect on respiratory disease, even when interacting with PM2.5 air pollution.
Discussion
This study adds to the current literature on PM2.5 exposure and health outcomes as it is among the first studies to examine occupational group and occupational characteristics as moderators of non-occupational air pollution exposure. The results of this study generally did not support our expectations that the health risks of PM2.5 exposure would vary be occupational factors. Several estimates were in the expected direction but not significant, which could be attributed to limited statistical power. However, overall, the estimates showed a mixed pattern of relationships that indicate that occupation likely does not moderate the link between residential air pollution exposure and health outcomes.
Air pollution was not associated with CMB disease or respiratory disease, as observed in Table 2. The null relationship between PM2.5 and cardiometabolic disease outcomes among workingage adults with employment stands in contrast to a significant and seemingly stronger relationship that has been reported among the larger MIDUS sample (in a study under review), which includes individuals who are retired or do not currently hold employment—both of which are groups that spend more time at one’s residence where the PM2.5 exposure may be more accurate. It would be interesting to research why fine particulate matter does not have the same effect on cardiometabolic diseases as it does respiratory diseases. Is this due to sample size, or is there a biological reasoning behind this finding? Occupation did not impact the relationship between air pollution and CMB disease outcomes. In relation to professional occupations, administrative, sales, and service occupations had higher CMB prevalence. The prevalence increase could be due to the environment in their jobs — added stress of job demands and the lifestyles of the people who work these jobs. A reason that job characteristics did not moderate the relationship between air pollution and CMB disease outcomes could be due to resources available to employees as they work. We looked at outdoor work environment, job strain, and occupational status. It could be that the participants of the study are not experiencing much distress at their job.
The statistically significant lower incidence of respiratory diseases (Table 3) among administrative occupations, in comparison to the professional group, may suggest that there are occupational differences playing a role in this association across occupations. Based solely on the results of this study, it is challenging to pinpoint an explanation as to why there was a difference specific to the administrative group (and not the other ones) or what specific factors could have contributed to those results.
Job strain was associated with higher prevalence of respiratory diseases (Table 3), an unexpected result as most research to date has indicated that there is no robust evidence for the association between job strain and risk of respiratory diseases (Magnusson Hanson et al., 2017; Heikkilä et al., 2014). On the other hand, the interaction between PM2.5 and job strain, which was not significant, possibly indicates that the combination of air pollution exposure and job strain is not a source/cause of higher risk of respiratory diseases.
Finally, the significant interactive effect of PM2.5 and sales and services occupational groups (Table 3) could mean that those occupations are more often exposed to or affected by air pollution exposure. Given that the air pollution measure of the study was based on residential tracts, those differences could also be explained by socio-economic differences, in which residential areas of lower socio-economic status tend to experience higher concentrations of air pollution (Hajat et al., 2015), assuming that sales and services are linked to low socio-economic status.
This study, however, is not without limitations. The PM2.5 measure was based on residential location, which differs from the workplace air pollution exposure, such that our air pollution measure represents long-term exposure only when within one’s residential neighborhood. Our sample was of moderate size but was less racially/ethnically diverse than the national population, limiting our ability to generalize. Also, the measures of CMB and respiratory diseases were selfreported, creating potential response bias in our dataset. Future research in the topic is needed, as there is limited research addressing this issue, and when doing so, it should address those limitations previously mentioned, for more generalizable conclusions.
Conclusion
In our study, the association between PM2.5 and incident respiratory diseases varied by occupational groups. Meanwhile, the association between PM2.5 and CMB diseases (prevalence and incidence) did not vary by occupational group. PM2.5 more strongly predicts incident respiratory disease for individuals in sales and service occupations compared to professional, but findings were mixed as the same moderation effect was not detected for prevalent respiratory disease. Although participants in administrative, sales, and service occupations had higher prevalent CMB disease in comparison to professional/managerial (white collar) professions, neither occupational group nor occupational factors acted as moderators, as previously hypothesized.
References
Ashwell, M., Gunn, P., & Gibson, S. (2012). Waist‐to‐height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta‐analysis. Obesity reviews, 13(3), 275-286.
Brook, R. D., Rajagopalan, S., Pope, C. A., Brook, J. R., Bhatnagar, A., Diez-Roux, A. V., Holguin, F., Hong, Y., Luepker, R. V., Mittleman, M. A., Peters, A., Siscovick, D., Smith, S. C., Whitsel, L., & Kaufman, J. D. (2010). Particulate Matter Air Pollution and Cardiovascular Disease. Circulation, 121(21), 2331–2378.
Christ, S. L., Fleming, L. E., Lee, D. J., Muntaner, C., Muennig, P. A., & CabanMartinez, A. J. (2012). The effects of a psychosocial dimension of socioeconomic position on survival: Occupational prestige and mortality among US working adults. Sociology of Health & Illness, 34(7), 1103–1117. https://doi.org/10.1111/j.14679566.2012.01456.x
Fang, S. C., Cassidy, A., & Christiani, D. C. (2010). A Systematic Review of Occupational Exposure to Particulate Matter and Cardiovascular Disease. International Journal of Environmental Research and Public Health, 7(4), 1773–1806. https://doi.org/10.3390/ijerph7041773
Gonzalez-Mulé, E., & Cockburn, B. S. (2021). This job is (literally) killing me: A moderated-mediated model linking work characteristics to mortality. Journal of Applied Psychology, 106(1), 140–151. https://doi.org/10.1037/apl0000501
Grzywacz, J. G., Segel-Karpas, D., & Lachman, M. E. (2016). Workplace Exposures and Cognitive Function During Adulthood: Evidence from National Survey of Midlife Development and the O*NET. Journal of occupational and environmental medicine, 58(6), 535-541.
Hajat, A., Hsia, C., & O’Neill, M. S. (2015). Socioeconomic Disparities and Air Pollution Exposure: a Global Review. Current environmental health reports, 2(4), 440–450. https://doi.org/10.1038/s41598-017-07508-x 1
Häusser, J., Mojzisch, A., Niesel, M., & Schulz-Hardt, S. (2010). Ten years on: A review of recent research on the Job Demand-Control (-Support) model and psychological wellbeing. Work & Stress, 24(1), 1–35. https://doi.org/10.1080/02678371003683747 Liu, C., Yang, D., Liu, Y., Piao, H., Zhang, T., Li, X., Zhao, E., Zhang, D., Zheng, Y., & Tang, X. (2023). The effect of ambient PM2.5 exposure on survival of lung cancer patients after lobectomy. Environmental Health, 22(1), 23. https://doi.org/10.1186/s12940-023-00976-x
Heikkilä, K., Madsen, I. E., Nyberg, S. T., Fransson, E. I., Westerlund, H., Westerholm, P. J., Virtanen, M., Vahtera, J., Väänänen, A., Theorell, T., Suominen, S. B., Shipley, M. J., Salo, P., Rugulies, R., Pentti, J., Pejtersen, J. H., Oksanen, T., Nordin, M., Nielsen, M. L., Kouvonen, A., … IPD-Work Consortium (2014). Job strain and the risk of severe asthma exacerbations: a meta-analysis of individual-participant data from 100 000 European men and women. Allergy, 69(6), 775–783. https://doi.org/10.1111/all.1238
Holman, D. J., & Hughes, D. J. (2021). Transactions between Big-5 personality traits and job characteristics across 20 years. Journal of Occupational and Organizational Psychology, 94(3), 762–788. https://doi.org/10.1111/joop.12332
Kim S.-Y.; Bechle, M.; Hankey, S.; Sheppard, L.; Szpiro, A. A.; Marshall, J. D. 2020. “Concentrations of criteria pollutants in the contiguous U.S., 1979 – 2015: Role of prediction model parsimony in integrated empirical geographic regression.” PLoS ONE 15(2), e0228535. https://doi.org/10.1371/journal.pone.0228535
Magnusson Hanson, L. L., Westerlund, H., Goldberg, M., & et al. (2017). Work stress, anthropometry, lung function, blood pressure, and blood-based biomarkers: A cross sectional study of 43,593 French men and women. Scientific Reports, 7, 9282. https://doi.org/10.1038/s41598-017-07508-x
Makri, A., & Stilianakis, N. I. (2008). Vulnerability to air pollution health effects. International Journal of Hygiene and Environmental Health, 211(3), 326–336. https://doi.org/10.1016/j.ijheh.2007.06.005
Matthews, T. A., Robbins, W., Preisig, M., von Känel, R., & Li, J. (2021). Associations of job strain and family strain with risk of major depressive episode: A prospective cohort study in US working men and women. Journal of Psychosomatic Research, 147, 110541.
Matthews, T. A., Chen, L., & Li, J. (2023). Increased job strain and cardiovascular disease mortality: A prospective cohort study in U.S. workers. Industrial Health, 61(4), 250–259. https://doi.org/10.2486/indhealth.2021-0233
Mao, Y., Hu, J., Ugnat, A.-M., Semenciw, R., & Fincham, S. (2001). Socioeconomic status and lung cancer risk in Canada. International Journal of Epidemiology, 30(4), 809–817. https://doi.org/10.1093/ije/30.4.809
National Center for O*NET Development. O*NET OnLine. https://www.onetonline.org/
Ning, J., Zhang, Y., Hu, H., Hu, W., Li, L., Pang, Y., Ma, S., Niu, Y., & Zhang, R. (2021). Association between ambient particulate matter exposure and metabolic syndrome risk: A systematic review and meta-analysis. Science of The Total Environment, 782, 146855. https://doi.org/10.1016/j.scitotenv.2021.146855
Nishida, C., & Yatera, K. (2022). The Impact of Ambient Environmental and Occupational Pollution on Respiratory Diseases. International Journal of Environmental Research and Public Health, 19(5), 2788. https://doi.org/10.3390/ijerph19052788
Peled, R. (2011). Air pollution exposure: Who is at high risk? Atmospheric Environment, 45(10), 1781–1785. https://doi.org/10.1016/j.atmosenv.2011.01.001
Scopp, T. S. (2003). The relationship between the 1990 census and census 2000 industry and occupation classification systems. Washington, DC: US Census Bureau.
Sidorchuk, A., Agardh, E. E., Aremu, O., Hallqvist, J., Allebeck, P., & Moradi, T. (2009). Socioeconomic differences in lung cancer incidence: A systematic review and meta-analysis. Cancer Causes & Control, 20(4), 459–471. https://doi.org/10.1007/s10552-009-9300-8
Van der Doef, M., & Maes, S. (1999). The Job Demand-Control (-Support) Model and psychological well-being: A review of 20 years of empirical research. Work and Stress, 13(2), 87–114. https://doi.org/10.1080/026783799296084
Xing, Y.-F., Xu, Y.-H., Shi, M.-H., & Lian, Y.-X. (2016). The impact of PM2.5 on the human respiratory system. Journal of Thoracic Disease, 8(1), E69–E74. https://doi.org/10.3978/j.issn.2072-1439.2016.01.19
Zhang, D.-D., Liu, J.-N., Ye, Q., Chen, Z., Wu, L., Peng, X.-Q., Lu, G., Zhou, J.-Y., Tao, R., Ding, Z., Xu, F., & Zhou, L. (2021). Association between socioeconomic status and chronic obstructive pulmonary disease in Jiangsu province, China: A population-based study. Chinese Medical Journal, 134(13), 1552–1560. https://doi.org/10.1097/CM9.0000000000001609
Media Attributions
- 137489262_table1(1)
- 146879582_table2
- 146879585_table3
- 146881378_table4

