Change Theory to Evidence in Practice
This module will discuss how to be a change agent and leader so that you can take evidence into practice and improve clinical outcomes.
Content contains:
- Changes and the Change Leader
- Promoting Successful Changes and Promoting EBP
- Change Theories
Objectives:
- Define change and change leader.
- Describe approaches to use to promote successful changes and promote EBP
- Describe common change theories
Change and Change Leader
Change is defined making something different or to replace something with something else (Oxford University Press, n.d.). It is common to resist change. Remember how we learned way back in Module 1 that it can be uncomfortable to rock the boat? However, change is essential for improving patient/family/community outcomes. As nurses, we must get more comfortable with being uncomfortable. Change is a fact of life for nurses. That includes making changes. Nurses can learn change strategies to help transition changes, such as promoting the use of evidence-based practice (EBP) in the workplace. A working knowledge of change theories allows nurses equipped with these skills to promote a smooth process to change.
At its core, change leadership is working together to create a shared understanding of change required to execute the strategy, and how to best make it happen. The nurse leader executing an EBP project is called a change leader or Change Agent. Through keen knowledge and application skills about change theory, nurses can promote evidence-based practice to improve patient, family, or community outcomes (Leibold, 2020).
Promotion for Successful Changes to EBP
What about when change is resisted? We have all experienced this, yes? Historically, development and dissemination of new practices was expected to progress from controlled trials to real-world effectiveness studies and then natural uptake by practice communities, but it has been recognized that this expectation is unrealistic (Fixsen et al., 2009; Proctor et al., 2009; Weisz et al., 2004). As we learned in Module 1, there can be a lag of as much as 15-20 years to integrate research findings into actual practice (Balas & Boren, 2000; Walker, 2004). As Leathers et al. (2016) points out, “Even when the practice change appears relatively simple, such as prescribing a different medication, a change in provider behavior is unlikely to occur on the basis of receiving information alone. When interventions are perceived as complex and involve an overall shift in practice orientation supporting uptake and sustained use presents even more challenges” (Henggeler & Lee, 2002; Reimer et al., 2005).
How do we even start in the process of making change? Start by asking yourself some questions to validate the goals and benefits of implementing a proposed change:
- Will the change improve clinical outcomes?
- Will it allow tracking of those outcomes?
- Will it help to more accurately identify areas for improvement?
- Will it increase the safety of care delivery?
- Will it make delivery more efficient?
- Will it resolve process barriers?
You can become a champion for the project or the change agent!
First, assess the workplace climate for their attitude toward change.
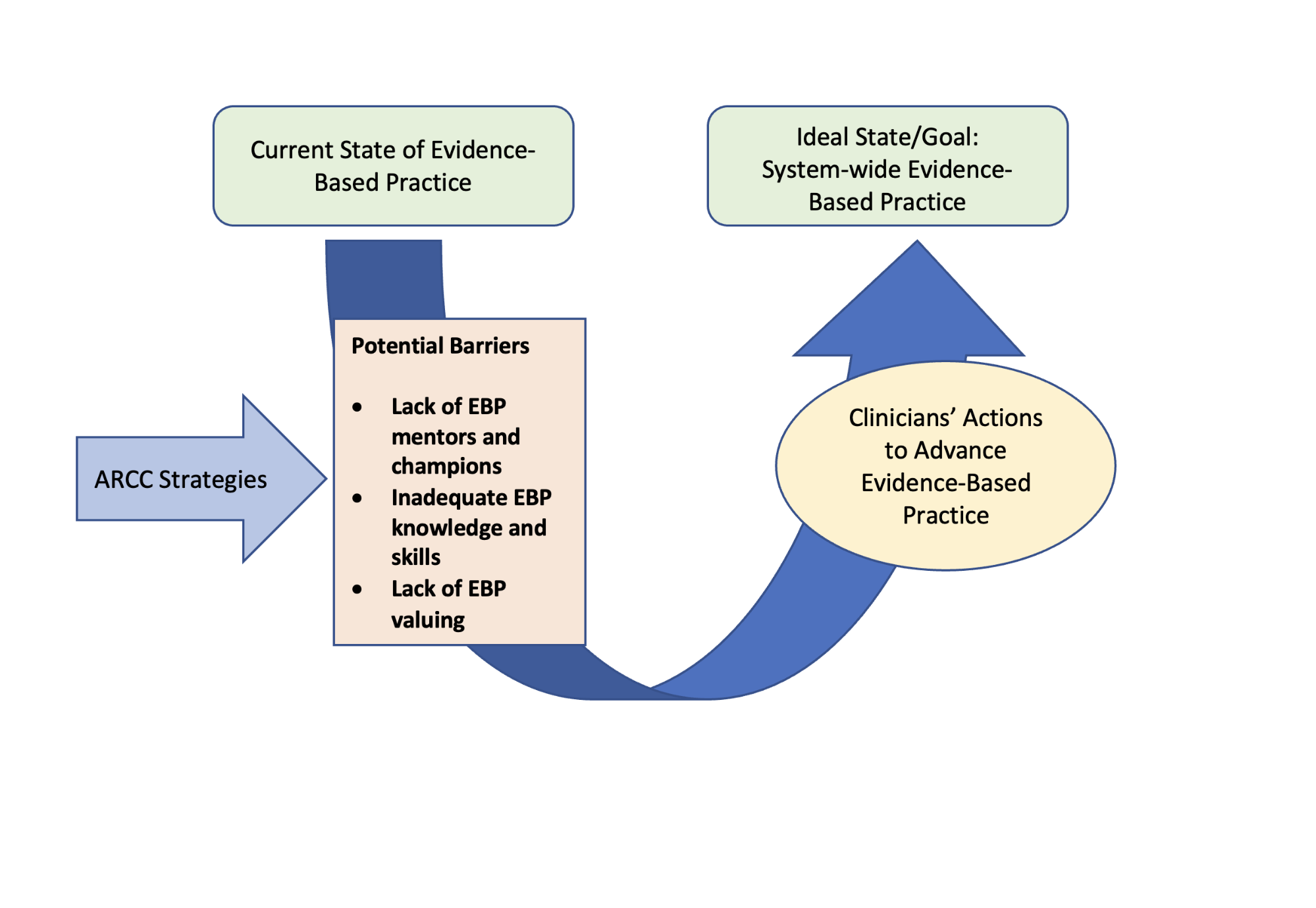
The Advancing Research and Clinical Practice through close Collaboration (ARCC©) Model is a system-wide framework for implementing and sustaining evidence-based practice in hospitals and healthcare systems. This model provides healthcare institutional and clinical settings with an organized conceptual framework that can guide the implementation process. The model is a product of nurse input about barriers and facilitators of EBP, control theory, and cognitive behavioral theory (Carver & Scheier, 1998; Beck et al., 1979).
Model to Guide Implementation and Sustainability of Evidence-Based Practice/ARCC
Then, create a climate in which staff see the change as an improvement for patients. Considering the barriers and facilitators to EBP at the organizational level, it is claimed that, besides personal characteristics, leadership and organizational climate are core elements for its implementation and sustainability. The personal characteristics of frontline staff that are crucial to the successful implementation of EBP include age, level of education, training, level of professional experience and knowledge, attitudes, and practice towards EBP (Apostolo, Cardoso, & Rodrigues, 2016).
When change is rejected, reflect on the who, what, why, and when of the rejection. Think how things could be improved to promote change in the future. Who are the change champions? Change champions are positive staff members who help promote change. Likewise, which staff members will try to obstruct change? Involve both the champions and the obstructers in the change project. Create an environment in which they own the change and want improved practices to succeed. Reframe the change and try again. Giving up is not an option—reframe the change in a different package.
Here is example of a change experience (Leibold, 2020):
There was a manager who did not like anyone else’s ideas. She would start to rip apart any idea before the person had even presented the possibility.
For example, a nurse had an idea to improve a work process within our unit (the current work process was time-consuming and outdated). However, every time the nurse tried to present the idea, she would not be through the first sentence of proposing the notion, and the manager would interrupt and say, “that will never work.”
For five years in a row, the nurse pitched the same idea differently. One day, the manager was quite stressed, and the nurse pitched the same idea but using a different frame that included hope, and the manager said, “that is a really good idea!” The staff and manager implemented the idea, and it worked beautifully and did improve quality and saved time for the healthcare team!
The point of this story is there is usually resistance to change, but it is important not to give up. Things do not always go super smooth on the first attempt! Reframe the strategy and learn from reflections of past failed change attempts. Timing is critical with change. Stakeholders will most likely agree to change when stressed with the current state and see the benefits of change. Stay the course.
Leadership and EBP:
Any nurse who writes and develops an evidence-based practice project is a leader, because they are leading the project! The nurse change agent can use positive thinking and positive energy to successfully complete the project! Several research studies in the literature relate to positivity in leaders!
In a study by Goswami et al. (2016), the use of positive humor by leaders and the emotions and work performance of employees at work was studied. Positive humor by the leader did increase employee positive emotions and work engagement. With leaders that used strong levels of transformational leadership, a higher level of positive emotions and work performance were present in the employees.
Wu and Lee (2017) studied the impact of leader positivity and group interaction. Leaders who have a positive approach, for example, empowering others, tend to result in group members that have positive psychological strategies (Wu & Lee, 2017).
Furthermore, team positivity has been linked to improved decision making and problem solving (Lehmann-Willenbrock et al., 2017). A positive leadership approach promotes team interaction, sharing, performance, and positive emotions. These are all approaches that a nurse change agent can use to implement EBP. A nurse leader is not a job title. Leadership means a person who is able to mentor, coach, steer, or role model for others in the quest for a shared goal. Any nurse who is promoting EBP is a leader.
As frontline providers and the largest body of healthcare professionals, nurses are called to further the efforts of leading research and practice improvements. The science of leadership is still emerging, and the lack of evidence-based leadership practices creates role confusion and delays professional success. AACN charges the prelicensure nurse with evidence-based practice and leadership educational competencies so that you have the knowledge and skillset to help make these changes.
Change Theories
There are theorists who have spent quite a bit of time developing change theories. Knowledge of the science of change theory is critical to altering organizational systems. Being conversant with various change theories can provide a framework for implementing, managing, and evaluating change within the context of human behavior. Change theories can be linear or non-linear; however, even linear theories do not unfold in a systematic and organized pattern. In the following section, we identify the role of leader and the typical pattern of events that occur in a change event (Wagner, 2018).
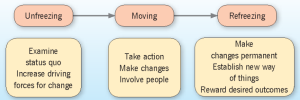
In Lewin’s Change Theory, the process of “Unfreezing, Moving, and Refreezing” is explored. Kurt Lewin’s change model is a simple and easy-to-understand framework to humanize the change management process. These three distinct stages of change (unfreeze, change, and refreeze) allow you to plan & implement the required change. Lewin’s theory proposes that individuals and groups of individuals are influenced by restraining forces, or obstacles that counter driving forces aimed at keeping the status quo, and driving forces, or positive forces for change that push in the direction that causes change to happen (Roussel et al., 2018).
Lippitt built upon Lewin’s original change theory to add more phases of emphasis. Lippitt’s Phases of Change focuses on the aspect of needing change, has seven phases, and uses similar language to the nursing process (Murray, 2017). Since the language is similar to the nursing process, nurses may benefit from using Lippitt’s model.
|
Nursing Process Elements |
Lippitt’s Change Theory Phases |
|
Assessment |
Phase 1: Diagnosing the problem Phase 2: Assessment the motivation and capacity for change Phase 3: Assess the change agents motivations and resources |
|
Planning |
Phase 4: Selecting progressive change objectives Phase 5: Choosing the appropriate role of the change agent |
|
Implementation |
Phase 6: Maintaining the change |
|
Evaluation |
Phase 7: Terminating the helping relationship |
Chaos theory explains why the smallest of change can create havoc. This is often referred to as the “butterfly effect” because of the impact the change can have on the system (Murray, 2017). The chaos theory reminds change agents to think with systems theory, because even the change in an EBP intervention that requires a supply can also change the supply department practices. For example, should a supply be needed for the new EBP project, it is important to consider the expense and to communicate with those responsible for ordering and inventorying the supply needed. Bloom (2010) points out that chaos theory is challenging for most people to apply. Bloom (2010) also argues that chaos theory is not really chaotic at all, as organizations are often seen as complex systems. The most important take-away from Chaos Theory is that when making change in an organization with an EBP project, it is important to assess how the change may impact all the departments.
Any EBP project necessitates change for health care workers and nurses. Since many people resist change, a planned method to promote change in the workplace is essential for the success of any EBP project. It is recommended to use a change theory and pay special attention to communicating with stakeholders and creating a climate where people perceive an improvement is needed. In this chapter, change approaches and theories were explained for the specific purposes of promoting EBP projects to improve patient/family/community outcomes.
Course Summary:
And, that’s it! You’ve made it through the course. Give yourself a big pat on the back! Take the information you have learned, be a change agent, and make changes in your clinical setting for the betterment of patient outcomes. The world of healthcare needs your insight, fresh eyes, energy, and knowledge.
References & Attribution
Chapter adapted from “The Art and Science of Evidence-based Practice in Nursing (2nd Edition)” by Nancy Leibold licensed CC BY NC
Balas, E.A., Boren, S.A. (2000). Managing clinical knowledge for health care improvement. In: Bemmel J, McCray AT, editors. Yearbook of medical informatics 2000: Patient-centered systems. Stuttgard, Germany: Schattauer Verlagsgesellschaft mbH. pp. 65–70.
Beck, A. T., Rush, A., Shaw, B., & Emery, G. (1979). Cognitive Therapy of Depression. The Guilford Press.
Bloom, S. (2010). Chaos theory and complex change. The Sanctuary Model. http://www.sanctuaryweb.com/TheSanctuaryModel/THESANCTUARYMODELFOURPILLARS/Pillar1SharedKnowledge/KNOWLEDGEABOUTGROUPS/OrganizationsasComplexAdaptiveSystems/ChaosTheoryandComplexChange.aspx
Carver, C.S. & Scheier, M.F. (1998). On the self-regulation of behavior. Cambridge University Press. https://doi.org/10.1017/CBO9781139174794
Henggeler S., & Lee T. (2002). What happens after the innovation is identified? Clinical Psychology: Science and Practice, 9, 191–194.
Leibold, N. (2020). The praxis of critical thinking in nursing (2nd ed.). Nanza Publications. Creative Commons License: BY NC ND. Available at https://thepraxisofcriticalthinkinginnursing.yolasite.com/
Fixsen DL, Naoom SF, Blase KA, Friedman RM, Wallace F. 9 (2005). Implementation research: A synthesis of the literature. Tampa, FL: University of South Florida, Louis de la Parte Florida Mental Health Institute, The National Implementation Research Network.
Goswami, A., Nair, P., Beehr, T., & Grossenbacher, M. (2016). The relationship of leaders’ humor and employees’ work engagement mediated by positive emotions: Moderating effect of leaders’ transformational leadership style. Leadership & Organization Development Journal, 37(8), 1083-1099. https://doi.org/10.1108/LODJ-01-2015-0001
Leathers et al., (2016). The effect of a change agent on use of evidence-based mental health practices. Administration Policy Mental Health, 43(5), 768-782.
Lehmann-Willenbrock, N., Chiu, M. M., Lei, Z., & Kauffeld, S. (2017). Understanding positivity within dynamic team interactions: A statistical discourse analysis. Group & Organization Management, 42(1), 39-78. https://doi.org/10.1177/1059601116628720
Mitchell, G. (2013). Selecting the best theory to implement planned change. Nursing Management, 20(1), 32-7.
Murray, E. J. (2017). Nursing leadership and management for patient safety and quality care (1st ed.). F.A. Davis Company.
Oxford University Press. (n.d.) Oxford Languages. https://languages.oup.com/google-dictionary-en/
Proctor, E. K., Landsverk, J., Aarons, G., Chambers, D., Glisson, C., & Mittman, B. (2009). Implementation research in mental health services: an emerging science with conceptual, methodological, and training challenges. Administration and Policy in Mental Health, 36(1), 24–34. https://doi.org/10.1007/s10488-008-0197-4
Riemer, M., Rosof-Williams, J., & Bickman, L. (2005). Theories related to changing clinician practice. Child and Adolescent Psychiatric Clinics of North America, 14(2), 241–254.
Roussel, L., Harris, J. L., & Thomas, P. L. (2018). Management and leadership for nurse administrators (8th ed.). Jones & Bartlett Learning.
Wagner, J. (2018). Leadership and Influencing Change in Nursing. CC BY. https://pressbooks.pub/leadershipandinfluencingchangeinnursing/
Weisz, J. R., Chu, B. C., & Polo, A. J. (2004). Treatment dissemination and evidence-based practice: Strengthening intervention through clinician-researcher collaboration. Clinical Psychology: Science and Practice, 11(3), 300–307. https://doi.org/10.1093/clipsy.bph085
Wu, W., & Lee, Y. (2017). Empowering group leaders encourages knowledge sharing: Integrating the social exchange theory and positive organizational behavior perspective. Journal of Knowledge Management, 21(2), 474-491. https://doi.org/10.1108/JKM-08-2016-0318