Hormonal Control of Bone and Remodeling of Bone
Objective 9.6
9.6.1 Explain how hormones are involved in bone growth and maintenance.
9.6.2 Explain the roles of calcitonin, parathyroid hormone, and calcitriol in bone remodeling and blood calcium regulation.
9.6.3 Describe the process of bone remodeling.
9.6.4 Compare and contrast the function of osteoblasts and osteoclasts during bone growth, repair, and remodeling.
Osteoblasts build bone. They lay down the organic (collagen) and inorganic (hydroxyapatite) extracellular matrix of bone. Osteoblasts are bone builders.

The Greek word κλαστος clastos means “breaking into pieces.” Iconoclasts are people who break icons into pieces; pyroclastic flow from volcanos breaks everything in its path into pieces. Osteoclasts break (chew) bone into pieces. Osteoclasts are bone chewers.
Bone tissue is a reservoir of calcium and phosphate. If blood calcium is low, the body breaks down mineralized bone to release calcium into the bloodstream. If blood calcium is high, the body removes calcium from the bloodstream and stores it in bone for future needs.
Both osteoblasts and osteoclasts are constantly at work on bone. A balance between building and chewing (osteoblasts and osteoclasts) is critical and is under hormonal control.
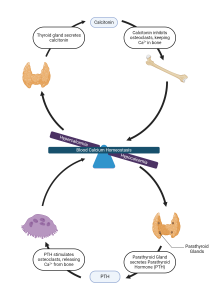
High blood calcium (hypercalcemia): If blood calcium is too high, it’s time to deposit the extra calcium in the “calcium bank” – bone. Calcitonin (CT), made by parafollicular cells in the thyroid gland, is secreted when blood calcium is too high. Calcitonin inhibits osteoclasts and their bone chewing, and slightly stimulates osteoblasts, allowing these bone builder cells to “get ahead” with bone building. In doing so, the osteoblasts absorb calcium from the bloodstream and deposit it as hydroxyapatite in bone, thereby lowering blood calcium levels back to normal.
Low blood calcium (hypocalcemia): If blood calcium falls too low, the body withdraws some from the bone “calcium bank.” Parathyroid hormone (PTH) is secreted from the parathyroid glands, a set of small, pea-shaped glands on posterior edges of the thyroid gland. PTH stimulates osteoclastic (chewing) activity. Osteoclasts break down the mineralized portion of bone [hydroxyapatite, Ca10(PO4)6(OH)2], releasing calcium into the bloodstream and raising the blood calcium level back to normal. There is also a slight inhibition of osteoblasts, which helps the osteoclasts release even more calcium into the bloodstream since the osteoblasts are not taking it back out.
In summary:
High blood Ca2+ → parafollicular cells in thyroid release calcitonin → calcitonin inhibits osteoclasts while osteoblasts keep depositing Ca2+ in new bone → blood Ca2+ goes down to normal → calcitonin release stops
Low blood Ca2+ → parathyroid glands release parathyroid hormone (PTH) → PTH stimulates osteoclasts → osteoclasts chew more bone → Ca2+ released from bone → blood Ca2+ goes up to normal → PTH release stops
One additional consideration is the third hormone involved in blood calcium homeostasis, calcitriol, which is hormonally-active vitamin D. PTH stimulates the kidneys to release calcitriol, which increases calcium absorption (from food) in the digestive system. This, along with the PTH, helps increase blood calcium, restoring it to normal.
Clinical Connection
Vitamin D & Bone Formation
 There are actually two D vitamins – Vitamin D2 (ergocalciferol) and Vitamin D3 (cholecalciferol). Both are available in a balanced diet (D2 from plant-sourced foods and D3 from animal-sourced foods), and D3 is made in the skin with the help of UV-B radiation (natural sunlight). Their common root, calciferol, indicates both play a role in calcium management (calciferol, calcium).
There are actually two D vitamins – Vitamin D2 (ergocalciferol) and Vitamin D3 (cholecalciferol). Both are available in a balanced diet (D2 from plant-sourced foods and D3 from animal-sourced foods), and D3 is made in the skin with the help of UV-B radiation (natural sunlight). Their common root, calciferol, indicates both play a role in calcium management (calciferol, calcium).
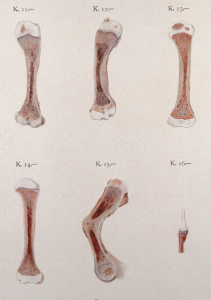
Like calcitriol, vitamins D2 and D3 stimulate calcium absorption in the digestive system. In the absence of dietary D vitamins, children cannot produce enough vitamin D in the skin and, therefore, are unable to absorb sufficient calcium to synthesize the large amount of mineralized bone needed during growth. The organic collagen component of bone is still produced normally, but without enough calcium for hydroxyapatite, the resulting bones are soft and pliable, producing the characteristic bent bones of the disease rickets.
In adults, failure to mineralize bone is usually not due to vitamin D deficiency. Rather, metabolic disturbances, cancer, and chemotherapy for cancer can cause problems with calcium homeostasis. This, in turn, can cause softening of bones, or osteomalacia.

Bone Remodeling
In children, bone is undergoing several dynamic processes all at once. In addition to constant remodeling and being involved in calcium homeostasis as just described, children’s bones are rapidly growing, along with the rest of the body. Human growth hormone (hGH) drives new bone tissue formation and bone growth at the epiphyseal plates of long bones and at multiple ossification centers in other bones. Levels of hGH are high in childhood, gradually decrease after puberty, drop fairly precipitously to low levels in young adults, and stay low the rest of our lives. After epiphyseal plates close, excess hGH (as from a secretory tumor) will not cause bones to lengthen further, but will cause bones to enlarge and thicken.
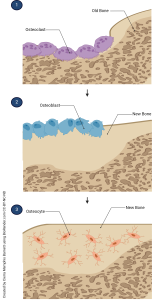
Throughout our lifetimes, bone is constantly remodeled. The activity that predominates—osteoblastic or osteoclastic—determines whether there is a net gain or a net loss of bone. In addition to blood calcium levels, physical stress (absence, presence, degree) also determines which type of osteo- cells are the most active. In adolescent and adult bones (and somewhat less so in children’s bones), moderate “good” stress (weight-bearing exercise) stimulates osteoblastic activity which thickens and strengthens bone.
Weight-lifters and other athletes know well the effects of moderate stress on bone formation and use that to their advantage in training. On the other hand, one of the side effects of extended space travel is bone loss due to being in a “weightless” environment (very little to no physical stress on bones). Astronauts loose just over 1% of their bone mass per month spent in space. “Bad” stress (friction in joints as a result of articular cartilage loss) also results in bone formation, in the form of bone spicules (bone spurs). This new bone formation is responsible for the joint deformities commonly seen in severe osteoarthritis.
The constant, active remodeling of bone is also the reason bone can heal after a fracture. The periosteum is critically important to and very involved in the repair process (more detail on this if/when you take our Pathophysiology course, HTHS 2230).
Examples
Clinical Connection
Osteoporosis
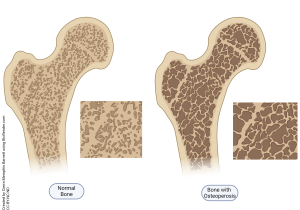
The elderly have very low levels of hGH and tend to have problems with calcium absorption and homeostasis. This may result in the disease osteoporosis (literally, holes in bone) which weakens bone tissue and leads to increased risk of fracture. Drugs called bisphosphonates stabilize hydroxyapatite and make it more difficult for osteoclasts to break it down (or chew it up, whichever makes the most sense to you). For this reason, many patients, especially middle-aged and older patients, take oral calcium to ensure calcium absorption from the digestive tract is maximal. Remembering that calcitriol is a form of vitamin D, and that it increases absorption of calcium from the gut, these same patients usually take a vitamin D supplement as well.
Media Attributions
- U09-026 replacement © Laboratoires Servier is licensed under a CC BY-SA (Attribution ShareAlike) license
- U09-027 Hormonal Control of Bone © BioRender is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U09-028 Sections through bones affected by rickets. Chromolithograph by W. Gummelt, ca. 1897 © Gummelt, W. is licensed under a Public Domain license
- L0014375 Photograph: three children with rickets © Wellcome Collection gallery is licensed under a CC BY (Attribution) license
- U09-030 Bone Remodeling © Barnett, Cerra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U09-032 Osteoporosis © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license

