Jonathan Akin
Unit Outline
Learning Objectives
At the end of this unit, you should be able to:
I. Identify and describe the components of the integumentary system.
II. Identify and describe the five layers of the epidermis of the skin, including the location and function of keratinocytes and melanocytes.
III. Specify the function(s) of epidermal derivatives, including hair, sebaceous glands, sudoriferous glands, ceruminous glands, and nails.
IV. Describe five major functions of the integumentary system.
V. Explain the origin of variation in pigmentation in skin and integumentary derivatives.
VI. Explain underlying causes of common integumentary system conditions.
What do you think of when you look at your skin in the mirror? Do you think about cleaning and caring for it, checking for damage from the sun, or maybe adding a tattoo? Or do you think about the fact that the skin is an organ belonging to one of the body’s most essential and dynamic systems, the integumentary system? The skin makes up about 16% of the body weight of an adult and covers an area of 1.5 to 2 m2, making it the largest organ system in the human body.
The integumentary system refers to the skin, as well as accessory structures, such as hair, nails, and glands. The skin is responsible for much more than your outward appearance, beginning with acting as a protective covering between your internal and external environments. This chapter will introduce the structure and many other functions of the integumentary system.
Part 1: Layers of the Skin
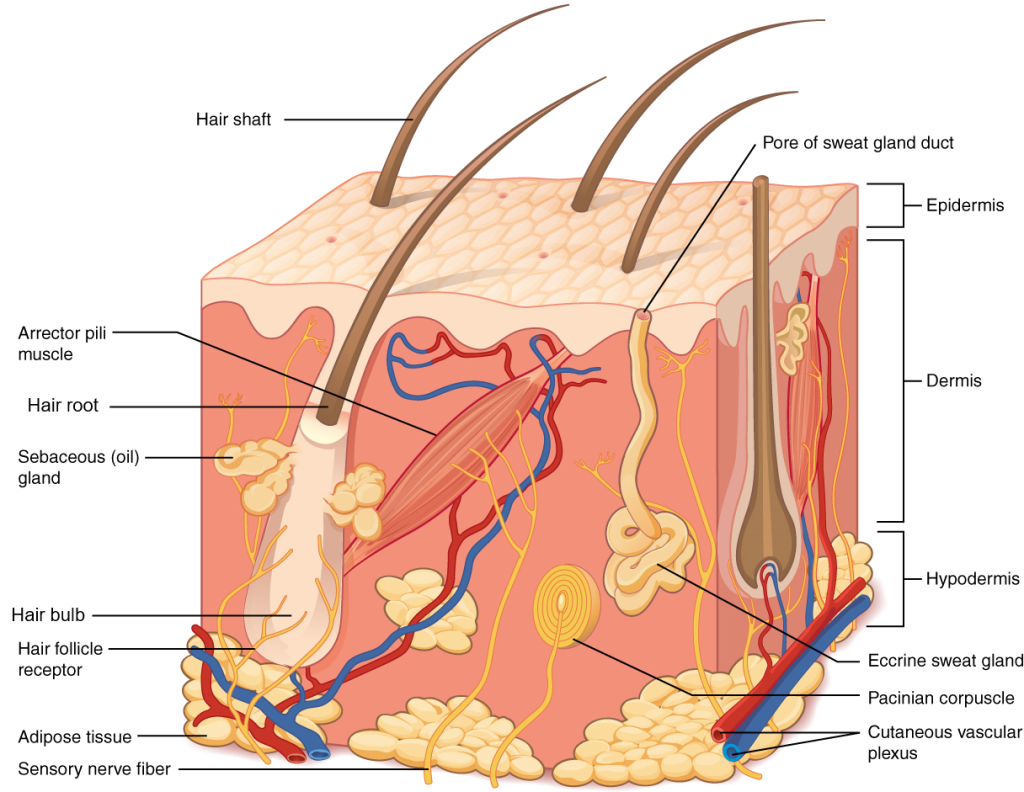
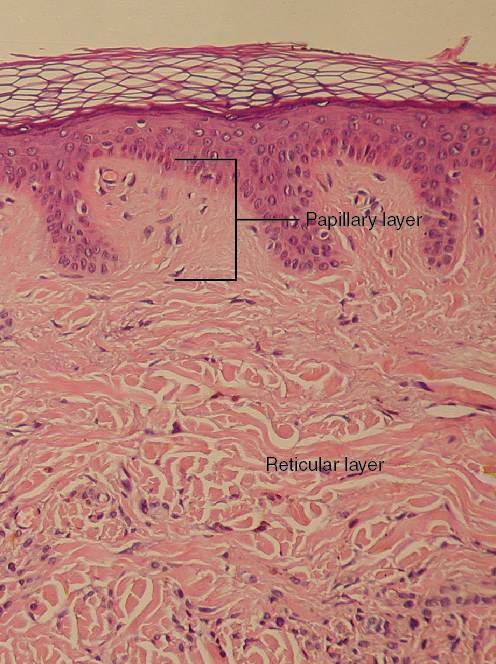
Although you may not typically think of the skin as an organ, it is in fact composed of different types of tissues that work together to perform unique and critical functions. The skin is composed of two main layers: an outer epidermis and a deeper dermis (Figure 9.1). The deeper layer of skin is well vascularized (i.e., has numerous blood vessels). It also has numerous sensory and nerve fibers, ensuring communication to and from the brain. The skin is ultimately affixed to deeper body structures, such as muscle, by connective tissue in a subcutaneous layer known as the hypodermis.

Epidermis
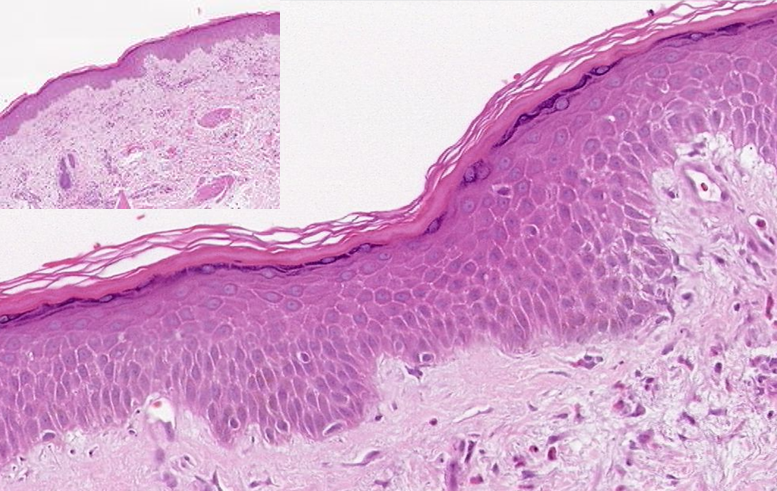
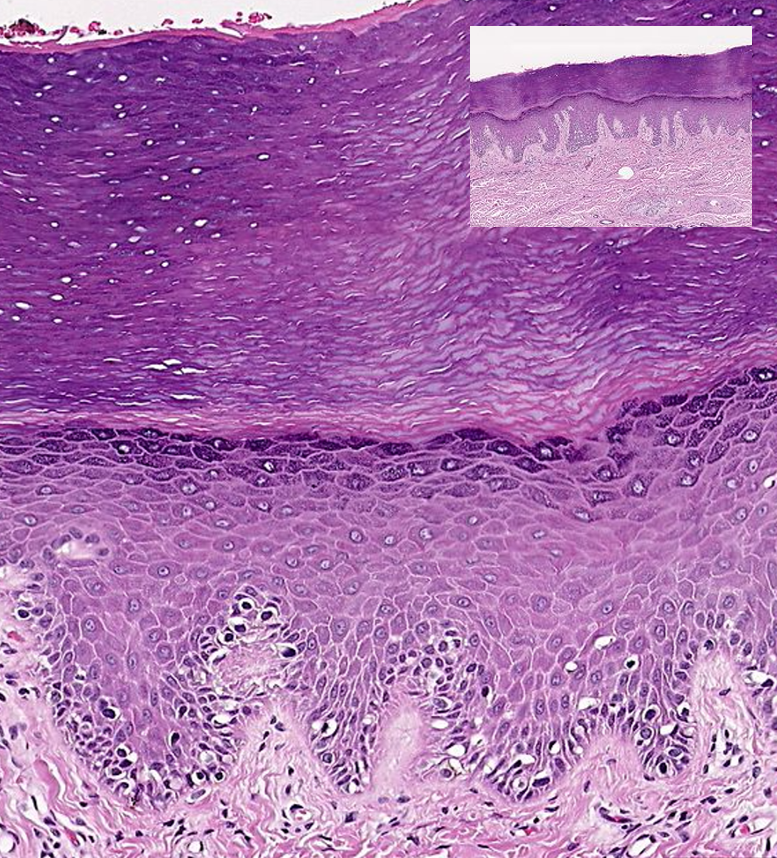
The epidermis (Figures 9.2 & 9.3) is composed of keratinized, stratified squamous epithelium. Like all epithelial tissue, it is avascular. The dark-staining epithelial cells of the epidermis are arranged in multiple strata with the outermost cells appearing the most squamous in shape. The majority of skin areas is classified as thin skin, meaning that it has four visible layers (i.e., strata) of cells (Figure 9.2). From deepest to superficial, these layers are the stratum basale, stratum spinosum, stratum granulosum, and stratum corneum. Thick skin, however, is found exclusively on the palms of the hands and the soles of the feet. This type of epidermis has an additional fifth layer, called the stratum lucidum, located between the stratum corneum and the stratum granulosum (Figures 9.3 & 9.4).
Regardless of whether skin is thick or thin, the dominant cells found in the epidermis are called keratinocytes. A keratinocyte is a cell that manufactures and stores the protein keratin. Keratin is an intracellular fibrous protein that confers hardness and water-resistance to skin, hair, and nails. Because the skin covers so much surface area, the presence of keratin helps prevent excessive water loss across the skin surface. The maturation of keratinocytes proceeds from the innermost toward the outermost layers. By the point the keratinocytes reach the stratum corneum, they have died and regularly slough away but will be replaced continuously by cells originating from the deeper layers (Figure 9.4).
1. Stratum Basale: The stratum basale (also called the stratum germinativum), is the deepest epidermal layer and attaches the epidermis to the basal lamina, below which lie the layers of the dermis. The cells in the stratum basale bond to the dermis via intertwining collagen fibers that make up the basement membrane.
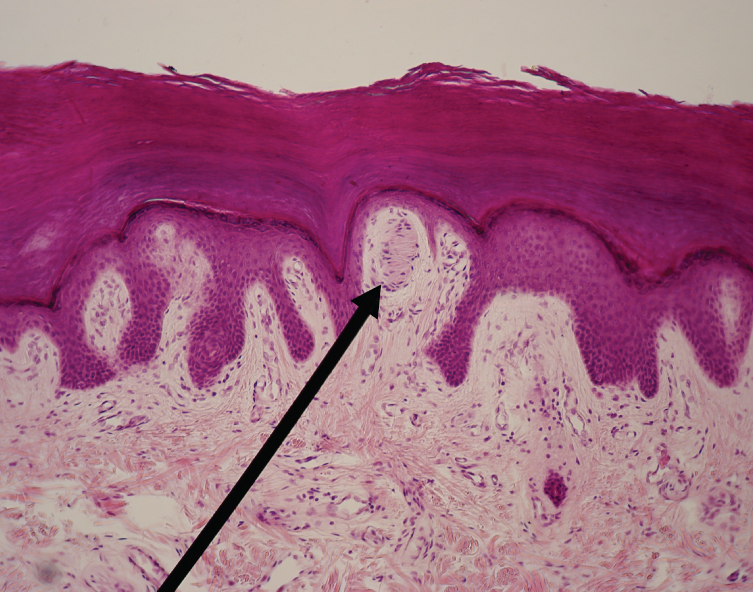
A finger-like projection, or fold, known as the dermal papilla (plural = dermal papillae) is found in the superficial portion of the dermis. Dermal papillae increase the strength of the connection between the epidermis and dermis; the greater the folding, the stronger the connection made (Figure 9.6). In a growing fetus, fingerprints form where the cells of the stratum basale meet the papillae of the underlying dermal layer (papillary layer), resulting in the formation of the ridges on your fingers that you recognize as fingerprints. Why these ridges form in the pattern that you see is a result of genetics and the fetal environment. Fingerprints are unique to each individual and are used for forensic analyses because the patterns do not change with the growth and aging processes.
The stratum basale is a single layer of cells primarily made of basal cells. A basal cell is a cuboidal-shaped stem cell that is a precursor of the keratinocytes of the epidermis. All of the keratinocytes are produced from this single layer of cells, which are constantly going through growth (mitosis) to produce new cells.
As new cells are formed, the existing cells are pushed superficially away from the stratum basale. Two other cell types are found dispersed among the basal cells in the stratum basale. The first is a Merkel cell, which functions as a receptor and is responsible for stimulating sensory nerves that the brain perceives as touch. These cells are especially abundant on the surfaces of the hands and feet. The second is a melanocyte, a cell that produces the pigment melanin. Melanin gives hair and skin its color and also helps protect the living cells of the epidermis from ultraviolet (UV) radiation damage.
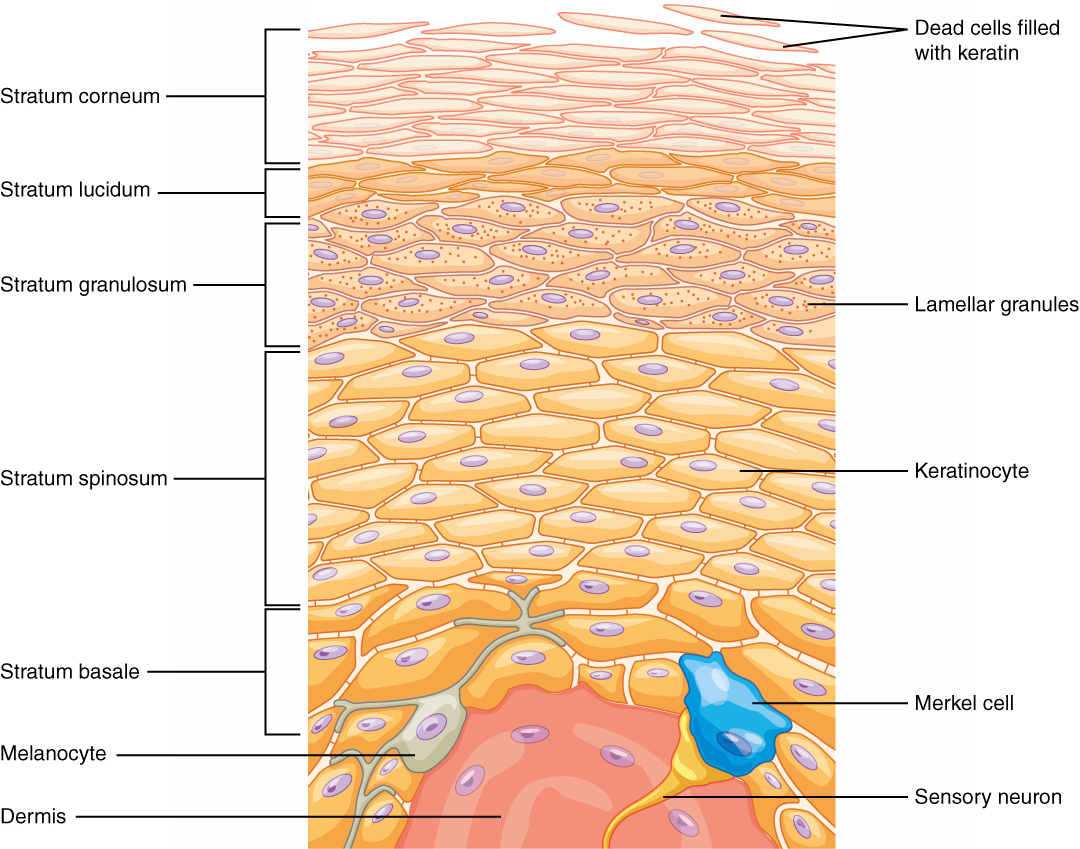
2. Stratum Spinosum: As the name suggests, the stratum spinosum is spiny in appearance due to the protruding cell processes that join the cells via a structure called a desmosome. The desmosomes interlock with each other and strengthen the bond between the cells. It is interesting to note that the “spiny” nature of this layer is an artifact of the staining process. Unstained epidermis samples do not exhibit this characteristic appearance. The stratum spinosum is composed of eight to ten layers of keratinocytes, formed as a result of cell division in the stratum basale (Figure 9.4). Also Interspersed among the keratinocytes of this layer, but not shown in Figure 9.4, is a type of dendritic cell called the Langerhans cell, which functions as a macrophage by engulfing bacteria, foreign particles, and damaged cells that occur in this layer.
The keratinocytes in the stratum spinosum begin the synthesis of keratin and release a water-repelling glycolipid that helps prevent water loss from the body, making the skin relatively waterproof. As new keratinocytes are produced atop the stratum basale, the keratinocytes of the stratum spinosum are pushed into the stratum granulosum.
3. Stratum Granulosum: The stratum granulosum has a grainy appearance due to further changes to the keratinocytes as they are pushed from the stratum spinosum. The cells (three to five layers deep) become flatter, their cell membranes thicken, and they generate large amounts of the proteins keratin, which is fibrous, and keratohyalin, which accumulates as granules within the cells (Figure 9.4). These two proteins make up the bulk of the keratinocyte mass in the stratum granulosum and give the layer its grainy appearance. The nuclei and other cell organelles disintegrate as the cells die, leaving behind the keratin, keratohyalin, and cell membranes that will form the stratum lucidum, the stratum corneum, and the accessory structures of hair and nails.
4. Stratum Lucidum: The stratum lucidum is a smooth, seemingly translucent layer of the epidermis located just above the stratum granulosum and below the stratum corneum. This thin layer of cells is found only in the thick skin of the palms, soles, and digits. The keratinocytes that compose the stratum lucidum are dead and flattened (Figure 9.4). These cells are densely packed with eleiden, a clear substance derived from keratohyalin that gives these cells their transparent (i.e., lucid) appearance and provides a barrier to water.
5. Stratum Corneum: The stratum corneum is the most superficial layer of the epidermis and is the layer exposed to the outside environment (Figure 9.4). The increased keratinization (also called cornification) of the cells in this layer gives it its name. There are usually 15 to 30 layers of cells in the stratum corneum. This dry, dead layer helps prevent the penetration of microbes and the dehydration of underlying tissues and provides a mechanical protection against abrasion for the more delicate, underlying layers. Cells in this layer are shed periodically and are replaced by cells pushed up from the stratum granulosum (or stratum lucidum in the case of the palms and soles of feet). The entire layer is replaced during a period of about four weeks. Cosmetic procedures, such as microdermabrasion, help remove some of the dry, upper layer and aim to keep the skin looking “fresh” and healthy.
Dermis
The dermis might be considered the “core” of the integumentary system (derma- = “skin”), as distinct from the epidermis (epi- = “upon” or “over”) and hypodermis (hypo- = “below”). It contains blood and lymph vessels, nerves, and other structures, such as hair follicles and sweat glands. The dermis is made of two layers of connective tissue that compose an interconnected mesh of elastin and collagenous fibers, produced by fibroblasts (Figure 9.5).
1. Papillary Layer: The papillary layer is made of loose, areolar connective tissue, which means the collagen and elastin fibers of this layer form a loose mesh. This superficial layer of the dermis projects into the stratum basale of the epidermis to form finger-like dermal papillae (Figure 9.5). Within the papillary layer are fibroblasts, a small number of fat cells (adipocytes), and an abundance of small blood vessels.
In addition, the papillary layer contains phagocytes, defensive cells that help fight bacteria or other infections that have breached the skin. This layer also contains lymphatic capillaries, nerve fibers, and touch receptors called the tactile (Meissner) corpuscles (Figure 9.11).
2. Reticular Layer: Underlying the papillary layer is the much thicker reticular layer, composed of dense, irregular connective tissue. This layer is well vascularized and has a rich sensory and nerve supply. The reticular layer appears reticulated (net-like) due to a tight meshwork of fibers. Elastin fibers provide some elasticity to the skin, enabling movement. Collagen fibers provide structure and tensile strength, with strands of collagen extending into both the papillary layer and the hypodermis. In addition, collagen binds water to keep the skin hydrated.
Hypodermis
The hypodermis (also called the subcutaneous layer or superficial fascia) is a layer directly below the dermis and serves to connect the skin to the underlying fascia (fibrous tissue) of the bones and muscles. It is not considered a part of the skin, although the border between the hypodermis and dermis can be difficult to distinguish. The hypodermis consists of well-vascularized, loose, areolar connective tissue and adipose tissue, which functions as a mode of fat storage and provides insulation and cushioning for the integument.
The hypodermis is one of the common injection sites for delivering medication because this layer contains relatively few blood vessels versus adipose tissue. Thus, medicines will be slowly absorbed by the body compared to other injection sites, such as a muscle or vein. Another term for an injection into the hypodermis is subcutaneous injection (Figure 9.6). For example, insulin injections are administered subcutaneously.
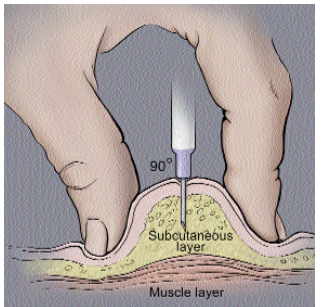
A correctly administered hypodermic injection places the needle into the skin at a 45–90 degree angle until the needle is completely covered by skin. No blood should appear in the syringe; if so, the needle should be repositioned before completing the injection.
Test Your Knowledge
I. Identify and describe the components of the integumentary system.
- List and identify all the organs and accessory structures of the integumentary system.
- Define “organ.” Explain why the skin specifically would fit your definition of an organ.
- For the two layers of the dermis, state their proper anatomical name and the specific tissue type of which each is primarily composed.
- Identify the accessory structures of the skin that are embedded in each of the two layers of the dermis.
- Draw an annotated diagram of the skin, clearly showing:
- The epidermal and dermal layers of the skin and the hypodermis
- The type(s) of tissue of that comprise each of the above layers indicated above (hint: refer back to the Tissue Structure topic)
- The layer(s) of the skin that contain(s) blood vessels
- The layer(s) of the skin that contain(s) nervous structures
II. Identify and describe the five layers of the epidermis of the skin, including the location and function of keratinocytes and melanocytes.
- Draw an annotated diagram of the epidermis of thick skin, clearly showing the five layers of the epidermis and specifying the distinguishing physical characteristics of each layer.
- Identify which layer in the diagram you created above would be missing from thin skin.
- Specify the two main types of cells found in the epidermis and which important chemical each of them produce. Briefly explain how each of those chemicals provide protection to underlying tissues.
Part 2: Accessory Structures of the Skin
Accessory structures of the skin include hair, nails, sweat glands, and sebaceous glands. These structures embryologically originate from the epidermis and can extend down through the dermis into the hypodermis.
Hair
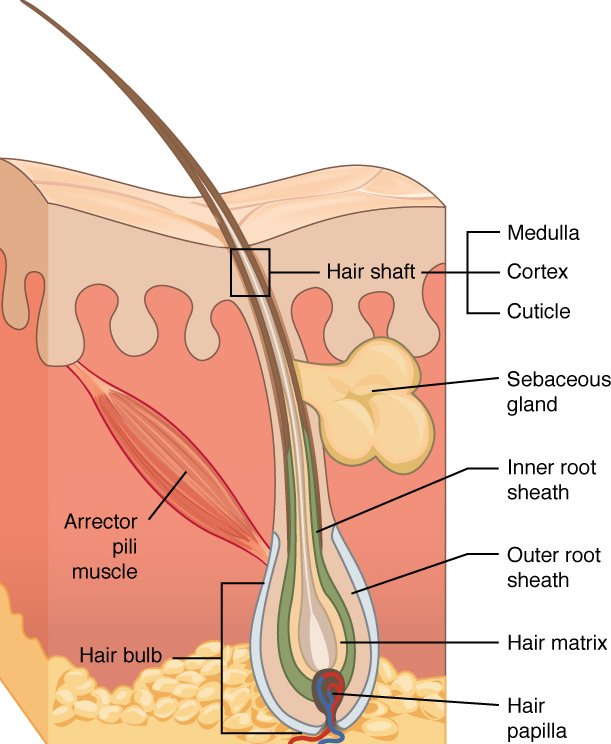
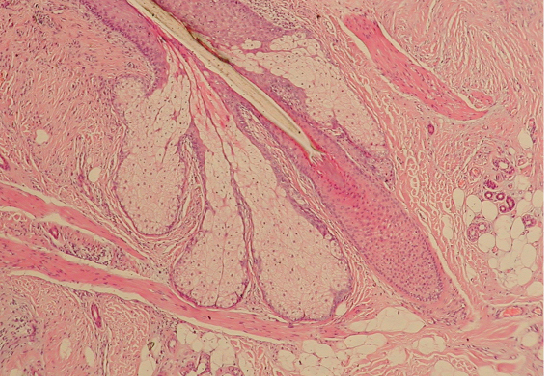
Hair is a keratinous filament growing out of the epidermis. It is primarily made of dead, keratinized cells. Strands of hair originate in an epidermal penetration of the dermis called the hair follicle (Figures 9.7 & 9.8).

The hair shaft is the part of the hair not anchored to the follicle, and much of this is exposed at the skin’s surface. The rest of the hair, which is anchored in the follicle, lies below the surface of the skin and is referred to as the hair root. The hair root ends deep in the dermis at the hair bulb (which is the deep end of the hair follicle). The root includes a layer of actively growing basal cells called the hair matrix. The hair bulb surrounds the hair papilla, which is made of connective tissue and contains blood capillaries and nerve endings from the dermis (Figure 9.7).
Just as the basal layer of the epidermis forms the layers of epidermis that get pushed to the surface as the dead skin on the surface sheds, the basal cells of the hair bulb divide and push cells outward in the hair root and shaft. The external hair is completely dead and composed entirely of keratin. For this reason, hair does not have sensation. Furthermore, you can cut your hair or shave without damaging the hair structure because the cut is superficial. Most chemical hair removers also act superficially; however, electrolysis and plucking both attempt to destroy the hair bulb so hair cannot grow.
Hair serves a variety of functions in the human body, including protection, sensory input, and communication. For example, hair on the head protects the skull from the sun. The hair in the nose and ears and around the eyes (eyelashes) defends the body by trapping and excluding dust particles that may contain allergens and microbes. Hair of the eyebrows prevents sweat and other particles from dripping into and bothering the eyes. Hair also has a sensory function due to sensory innervation by a hair root plexus surrounding the base of each hair follicle.
Hair is extremely sensitive to air movement or other disturbances in the environment, much more so than the skin surface. This feature is also useful for the detection of the presence of insects or other potentially damaging substances on the skin surface. Each hair root is connected to a smooth muscle called the arrector pili that contracts in response to nerve signals from the nervous system, making the external hair shaft “stand up” (Figure 9.7). The primary purpose for this would be to trap a layer of air to add insulation, but in humans, the hairs are too far away from each other to be effective as insulation. The erection of the hair shafts in response to low body temperature nevertheless persists in humans and is visible as “goose bumps.”
Hair grows and is eventually shed and replaced by new hair. On average, 50 hairs are lost and replaced per day. Hair loss occurs if there is more hair shed than what is replaced and can happen due to hormonal or dietary changes. Hair loss can also result from the aging process, or the influence of hormones.
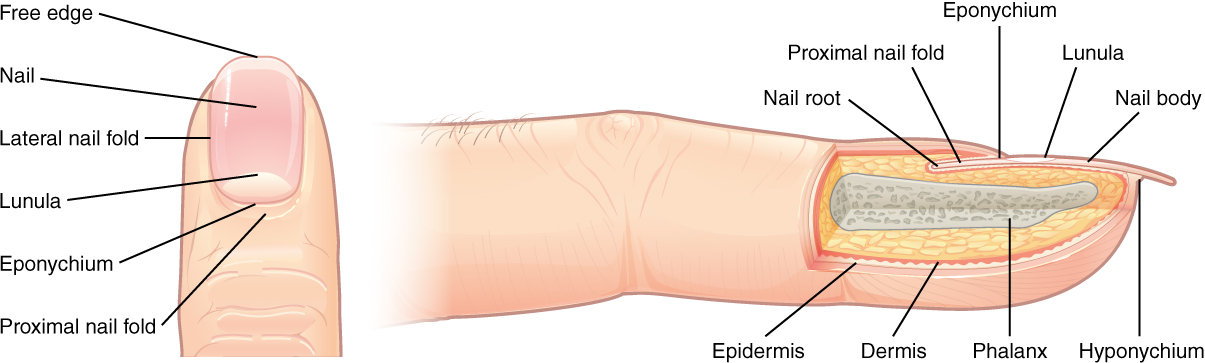
Nails
The nail bed is a specialized structure of the epidermis that is found at the tips of our fingers and toes. The nail body is formed on the nail bed and protects the tips of our fingers and toes, as they are the farthest extremities and the parts of the body that experience the maximum mechanical stress (Figure 9.9). In addition, the nail body forms a back support for picking up small objects with the fingers. The nail body is composed of densely packed dead keratinocytes. The nail body forms at the nail root, which has a matrix of proliferating cells from the stratum basale that enables the nail to grow continuously.
Sweat Glands
When the body becomes warm, sudoriferous glands produce sweat to cool the body. Sweat glands develop from epidermal projections into the dermis and are classified as merocrine glands; that is, the secretions are excreted by exocytosis through a duct without affecting the cells of the gland. There are two main types of sweat glands, each secreting slightly different products.
An eccrine sweat gland is a type of gland that produces a hypotonic (relative to blood plasma) sweat for thermoregulation. These glands are found all over the skin’s surface but are especially abundant on the palms of the hand, the soles of the feet, and the forehead (Figure 9.10).
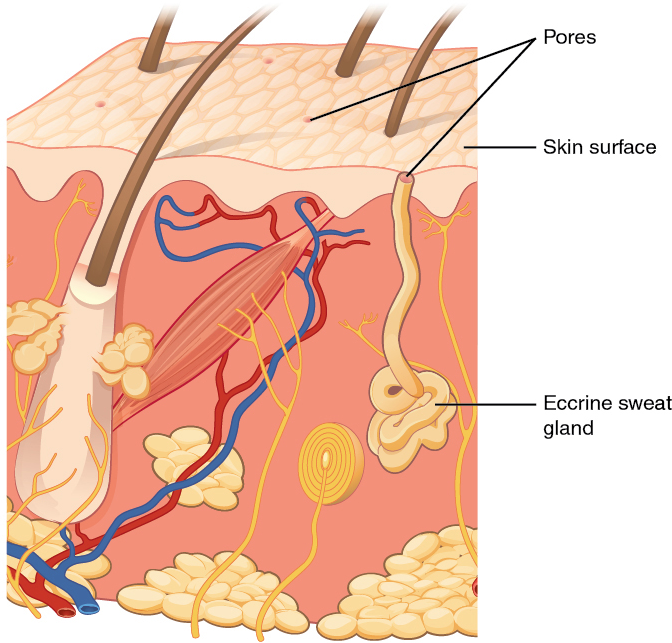
They are coiled glands lying deep in the dermis, with the duct rising up to a pore on the skin surface, where the sweat is released. This type of sweat, released by exocytosis, is composed mostly of water, with some salt, antibodies, traces of metabolic waste, and dermicidin, an antimicrobial peptide. Eccrine glands are a primary component of thermoregulation in humans and thus help to maintain homeostasis.
An apocrine sweat gland is usually associated with hair follicles in densely hairy areas, such as the armpits and anogenital regions. Apocrine sweat glands are larger than eccrine sweat glands and lie deeper in the dermis, sometimes even reaching the hypodermis, with the duct normally emptying into the hair follicle. In addition to water and salts, apocrine sweat includes organic compounds that make the sweat thicker and subject to bacterial decomposition and subsequent smell. The release of this sweat is under both nervous and hormonal control and plays a role in the poorly understood human pheromone response. Most commercial antiperspirants use an aluminum-based compound as their primary active ingredient to stop sweat. When the antiperspirant enters the sweat gland duct, the aluminum-based compounds precipitate due to a change in pH and form a physical block in the duct, which prevents sweat from coming out of the pore.
There are several different types of modified apocrine glands that have become specialized to serve particular functions. One example is the mammary gland, which allows mammals to produce and secrete milk (a mixture of water, salt, and organic compounds) in appropriate concentrations to nourish growing offspring. Another example is the ceruminous gland, which is found in the external auditory meatus (ear canal) and secretes a pigmented mixture of lipids and proteins that combines with the sebum secreted from sebaceous glands (see below) and dead keratinocytes to form cerumen (earwax). This sticky substance is used to trap small foreign bodies (e.g., dirt, small insects) and help prevent damage to the tympanic membrane (eardrum).
Sebaceous Glands
A sebaceous gland is a type of oil gland that is found all over the body and helps to lubricate and waterproof the skin and hair. Most sebaceous glands are associated with hair follicles (Figures 9.7 & 9.8). They generate and excrete sebum, a mixture of lipids, onto the skin surface, thereby naturally lubricating the dry and dead layer of keratinized cells of the stratum corneum, keeping it pliable. The fatty acids of sebum also have antibacterial properties and prevent water loss from the skin in low-humidity environments. The secretion of sebum is stimulated by hormones, many of which do not become active until puberty. Thus, sebaceous glands are relatively inactive during childhood.
Test Your Knowledge
III. Specify the function(s) of epidermal derivatives, including hair, sebaceous glands, sudoriferous glands, ceruminous glands, and nails.
- List the main function(s) served in human by the hairs of the:
- Scalp
- Eyelids
- Nostrils
- Rest of the body
- What is the main function(s) of nails, and what about their structure allows them to perform that function(s)?
- Complete the following table regarding integumentary glands:
| Gland name | Location(s) in the body | Product contents | Product function(s) |
| Eccrine sudoriferous gland | |||
| Apocrine sudoriferous gland | |||
| Ceruminous gland | |||
| Sebaceous gland |
Part 3: Functions of the Integumentary System
The skin and accessory structures perform a variety of essential functions, such as protecting the body from invasion by microorganisms, chemicals, and other environmental factors; preventing dehydration; acting as a sensory organ; modulating body temperature and electrolyte balance; and synthesizing vitamin D. The underlying hypodermis has important roles in storing fats, forming a “cushion” over underlying structures and providing insulation from cold temperatures.
Protection: The skin protects the rest of the body from the basic elements of nature such as wind, water, and UV sunlight. It acts as a protective barrier against water loss, due to the presence of layers of keratin and glycolipids in the stratum corneum. It also is the first line of defense against abrasive activity due to contact with grit, microbes, or harmful chemicals. Sweat excreted from sweat glands deters microbes from over-colonizing the skin surface by generating dermicidin, which has antibiotic properties.
Sensation: The fact that you can feel an ant crawling on your skin, allowing you to flick it off before it bites, is because the skin, and especially the hairs projecting from hair follicles in the skin, can sense changes in the environment. The hair root plexus surrounding the base of the hair follicle senses a disturbance and then transmits the information to the central nervous system (brain and spinal cord), which can then respond by activating the skeletal muscles of your eyes to see the ant and the skeletal muscles of the body to act against the ant.
The skin acts as a sense organ because the epidermis, dermis, and the hypodermis contain specialized sensory nerve structures that detect touch, surface temperature, and pain. These receptors are more concentrated on the tips of the fingers, which are most sensitive to touch, especially the tactile (Meissner) corpuscle (Figure 9.11), which responds to light touch, and the lamellated (Pacinian) corpuscle, which responds to vibration.
Merkel cells (Figure 9.4), seen scattered in the stratum basale, are also touch receptors. In addition to these specialized receptors, there are sensory nerves connected to each hair follicle, pain and temperature receptors scattered throughout the skin, and motor nerves that innervate the arrector pili muscles and glands. This rich innervation helps us sense our environment and react accordingly.
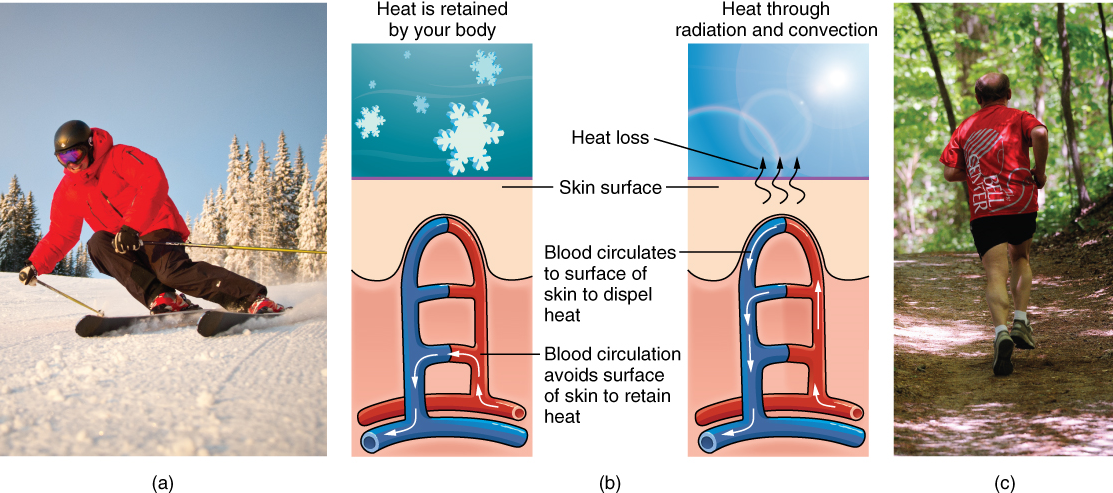
Thermoregulation: The integumentary system helps regulate body temperature through its tight association with the nervous system. The nervous system is continuously monitoring body temperature and initiating appropriate motor responses. Recall that sweat glands, accessory structures to the skin, secrete water, salt, and other substances to cool the body when it becomes warm.
Even when the body does not appear to be noticeably sweating, approximately 500 mL of sweat (insensible perspiration) are secreted a day. If the body becomes excessively warm due to high temperatures, vigorous activity (Figure 9.12ac), or a combination of the two, sweat glands will be stimulated by the sympathetic nervous system to produce large amounts of sweat, as much as 0.7 to 1.5 L per hour for an active person. When the sweat evaporates from the skin surface, the body is cooled as body heat is dissipated.
In addition to sweating, arterioles in the dermis dilate so that excess heat carried by the blood can dissipate through the skin and into the surrounding environment (Figure 9.12b). This accounts for the skin redness that many people experience when exercising.
When body temperatures drop, the arterioles constrict to minimize heat loss, particularly in the ends of the digits and tip of the nose. This reduced circulation can result in the skin taking on a whitish hue. Although the temperature of the skin drops as a result, passive heat loss is prevented, and internal organs and structures remain warm. If the temperature of the skin drops too much (such as environmental temperatures below freezing), the conservation of body core heat can result in the skin actually freezing, a condition called frostbite.
Other Functions: The epidermal layer of human skin synthesizes vitamin D when exposed to UV radiation. In the presence of sunlight, a precursor of vitamin D is synthesized from a derivative of the cholesterol in the skin. Further biochemical reactions in the liver and kidney then produce calcitriol, the active chemical form of the vitamin, which has important roles in the absorption of calcium from the small intestine. In present day society, vitamin D is added as a supplement to many foods, including milk and orange juice, compensating for the need for sun exposure.
The skin is also a minor component of the excretory system, which is used to remove metabolic waste products from the body. Most metabolic waste products are removed from the body via the urinary and respiratory systems. However, the skin does release in sweat some of the metabolic waste products that are found in blood plasma, albeit at relatively low concentrations.
Test Your Knowledge
IV. Describe five major functions of the integumentary system.
- Explain the mechanisms by which the integumentary system carries out each of the following functions:
- Protection
- Body temperature regulation
- Sensation
- Synthesis of vitamin D
- Excretion
Part 4: Pigmentation
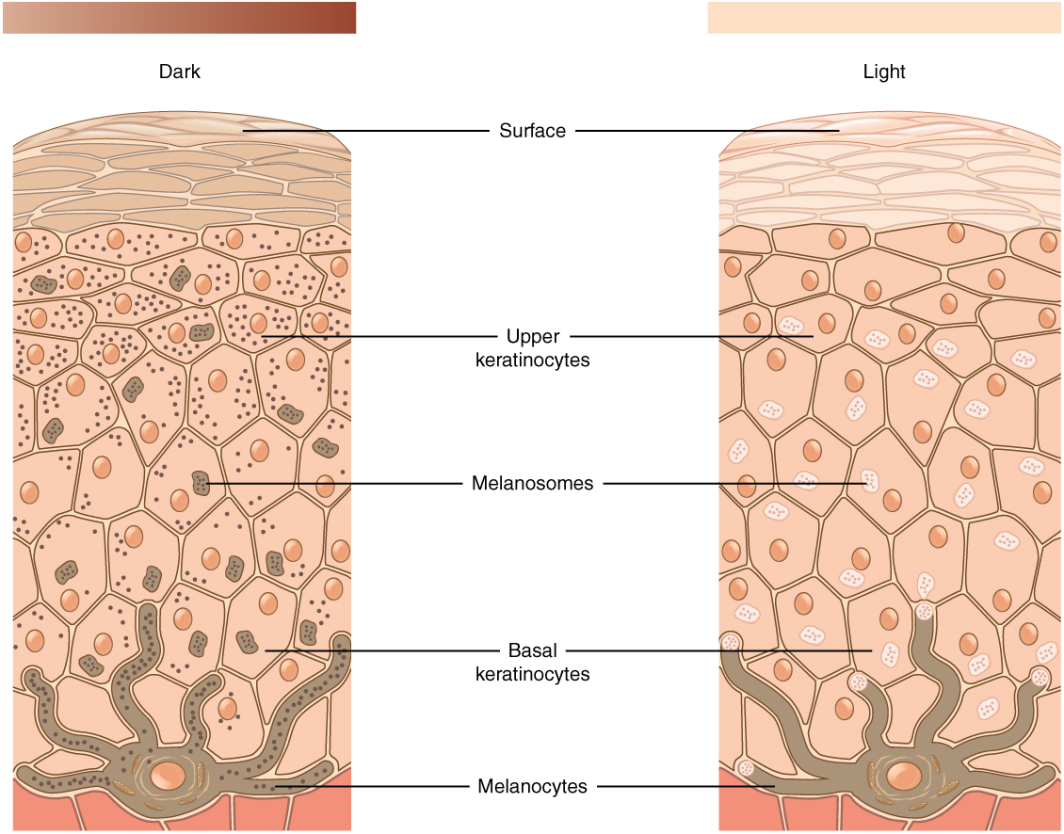
Most cells in the body are naturally colorless, but the integumentary system appears colorful due in part to the presence of pigments. The color of skin is influenced by a number of pigments, including melanin, carotene, and hemoglobin. Recall that melanin is produced by cells called melanocytes, which are found scattered throughout the stratum basale of the epidermis. The melanin is transferred in the keratinocytes via a cellular vesicle called a melanosome (Figure 9.13).
Dark-skinned individuals produce more melanin than those with pale skin. Exposure to the UV rays of the sun or a tanning salon causes melanin to be manufactured and built up in keratinocytes, as sun exposure stimulates keratinocytes to secrete chemicals that stimulate melanocytes. The accumulation of melanin in keratinocytes results in the darkening of the skin, or a tan. This increased melanin accumulation protects the DNA of epidermal cells from UV ray damage. In contrast, too much melanin can interfere with the production of vitamin D, an important nutrient involved in calcium absorption.
It requires about 10 days after initial sun exposure for melanin synthesis to peak, which is why pale-skinned individuals tend to suffer sunburns of the epidermis initially. Dark-skinned individuals can also get sunburns but are more protected than are pale-skinned individuals. Melanosomes are temporary structures that are eventually destroyed by fusion with lysosomes; this fact, along with melanin-filled keratinocytes in the stratum corneum sloughing off, makes tanning impermanent.
Too much sun exposure can eventually lead to wrinkling due to the destruction of the cellular structure of the skin, and in severe cases, can cause sufficient DNA damage to result in skin cancer.
Persons with albinism do not produce any melanin (Figure 9.14), and their skin and integumentary derivatives, such as a hair, are devoid of pigmentation; this necessitates seeking enhanced protection against UV damage when out in the sunlight. This condition is recessively inherited and does not cause ill health effects other than vision. The lack of pigmentation throughout the eye, not just in the iris, can affect visual acuity.

Patches of melanin-free skin characterizes the condition known as vitiligo (Figure 9.15). The primary cause is an autoimmune response that destroys the melanocytes in localized regions of the skin in the body but, unlike albinism, does not affect the whole skin surface of the body. This condition is more noticeable in dark-skinned individuals because the melanin-free patches stand out more. There are no additional health effects of having vitiligo, and moreover, it is not contagious.

In addition to natural pigmentation, some persons augment skin color artificially by getting a tattoo. A permanent tattoo involves injecting artificial pigments into the dermal layer of the skin where it can be seen through the overlying epidermis. Some tattoo ink colors, however, do fade over time as the pigments are broken down by immune system cells and dispersed from the original pattern.
Variation in Skin Color
One of the most variable aspects of human anatomy is skin tone, resulting in a rainbow of color shades ranging from yellow to reddish to tan to brown to black. These different colors result from varying ratios of the dominant pigments of the skin: melanin and carotene.
While the number of melanocytes in the epidermis is the same among persons of different skin tones, the color differences result from differences in activity of cells and location of pigment deposition. For example, dark-skinned individuals have more active melanocytes than light-skinned individuals, and dark-skinned individuals accumulate pigment in the more superficial stratum granulosum layer.
In addition, skin color is affected by blood flow through capillaries in the dermis, which contributes red coloration from hemoglobin in red blood cells. Emotional states, especially in light-skinned individuals, can be revealed by skin tone appearance. Skin can flush red during embarrassment or blanch white from fear. Indeed, the appearance of skin is noticeably different after death due to lack of oxygen and reduced blood circulation.
Excess blood pooling in the dermis of the skin, called a hematoma, due to damage from a punch or bump, is visible as a bruise through the outer layers of the skin. While initially red, the bruise color will gradually progress through a series of color changes—blue/black to purple to green to yellow as hemoglobin is broken down and transformed into bilirubin.

Freckles and Moles
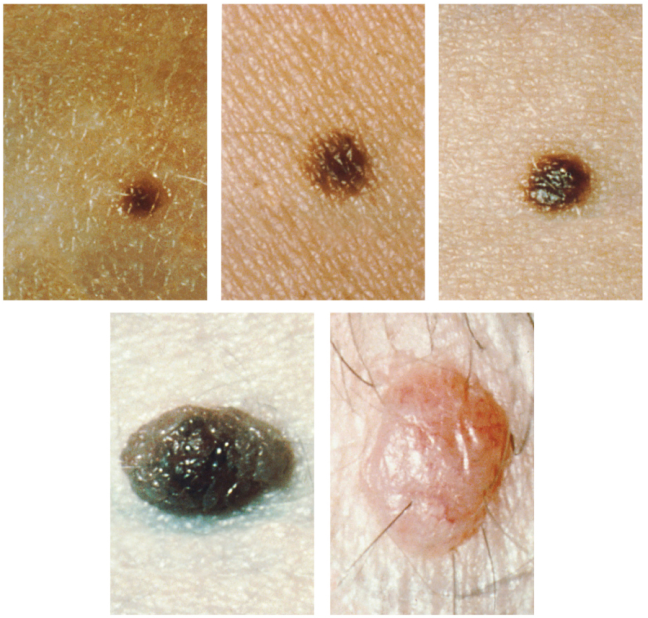
Dermatology is the medical specialty that studies the integument. In a dermatological exam, special attention is given to spots of pigmentation called freckles and moles. Freckles are flat spots of pigmentation that develop as a result of overactivity of melanocytes in these areas. They are prevalent in sun-exposed areas of the body, such as the face, arms, neck, and chest, but will fade seasonally.
Moles (also known as nevi) are larger masses of melanocytes, and although most are benign, they should be monitored for changes that might indicate the presence of cancer (Figure 8). Cancerous moles may have an irregular border or uneven halves. In contrast to freckles, moles are raised and do not disappear with seasons.
Hair color
Similar to the skin, hair gets its color from the pigment melanin, produced by melanocytes in the hair papilla. Different hair color results from differences in the type of melanin, which is genetically determined. As a person ages, the melanin production decreases, and hair tends to lose its color and becomes gray and/or white.
Test Your Knowledge
V. Explain the origin of variation in pigmentation in skin and integumentary derivatives.
- Describe how melanocytes transfer pigment to keratinocytes.
- Explain how skin tone differences are not related to melanocyte number.
- Describe the roles pigmentation and blood flow play in skin tone appearance.
- Use the evolutionary past to explain dark-skinned and light-skinned individuals.
- Compare and contrast tanning, bruising, albinism, vitiligo, freckles, and moles in terms of origin, appearance, and longevity.
Part 5: Skin Conditions
Because the skin is the most conspicuous organ of the body, any changes to skin appearance may be noticeable to yourself and to others. Are these changes just due to variation among humans in skin color? Or do these changes indicate an underlying cause due to hormones, stress, or disease? Understanding these conditions can make you feel better about yourself and better informs how others see you. Your understanding of the structure and function of the skin from previous sections of this chapter can be used to better understand these conditions.
Acne
Acne is a common skin condition that involves the appearance of temporary blemishes on the surface of the skin called pimples (Figure 9.17). These reddish and swollen structures can appear where hair follicles emerge from the skin surface. The association between acne and hair follicles results from a blockage of the oil (i.e., sebum) products from sebaceous glands. Normally, these secretions lubricate the hair shaft that grows from the follicle and spill out to the surrounding epidermal surface. Sebum production increases during puberty; thus, teenagers often experience more outbreaks of acne than adults. However, pimples can develop throughout life and are often exacerbated by stress hormones.

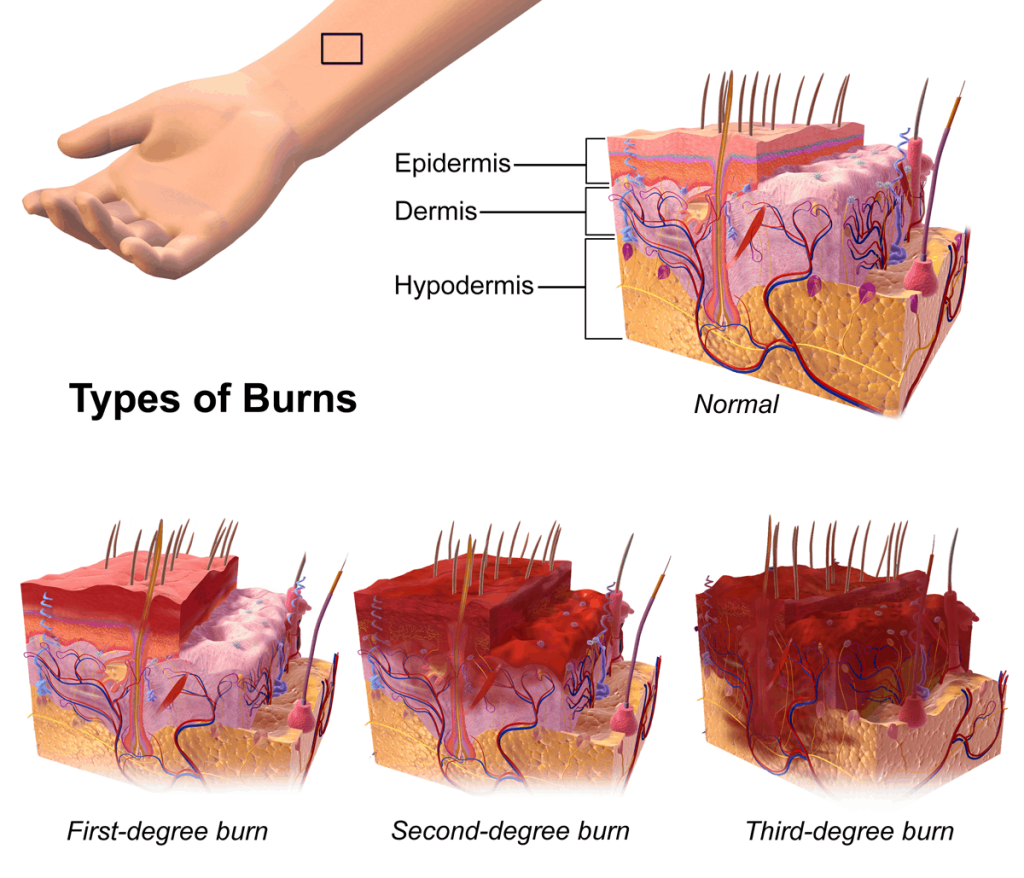
Burns
Burns are damage to skin caused by exposure to radiation, chemicals, or electricity. Any burn is serious and warrants care to restore the important functions provided by the skin. But burn severity is typically ranked due to the extent of damage to the skin layers (Figure 9.18).
A first-degree burn, such as from a sunburn or brushing into a hot stove element, is the least severe category of burn severity. This kind of burn damage is limited to the epidermis, causes reddening, and is painful to the touch.
A second-degree burn involves both the epidermis and dermis. The burn damage extends into the dermal layer and may cause leakage of fluid, forming a blister (Figure 9.19). The loss of the epidermal protection and possible bursting of the blister makes the burn area more susceptible to infection. In addition, scars may appear in the healed area.
The third-degree burn is the most severe burn condition and involves the destruction of both the epidermal and dermal areas. The damaged region extends to the hypodermis, and because nerves are destroyed along with the dermis, painful sensation may be absent. This extensive burn damage cannot heal on its own and generally requires skin grafting.
Repair of burn damage requires both enhanced hydration and nutrition, as there will be increased water loss across damaged areas, and the regeneration of tissue is energetically expensive.

Eczema
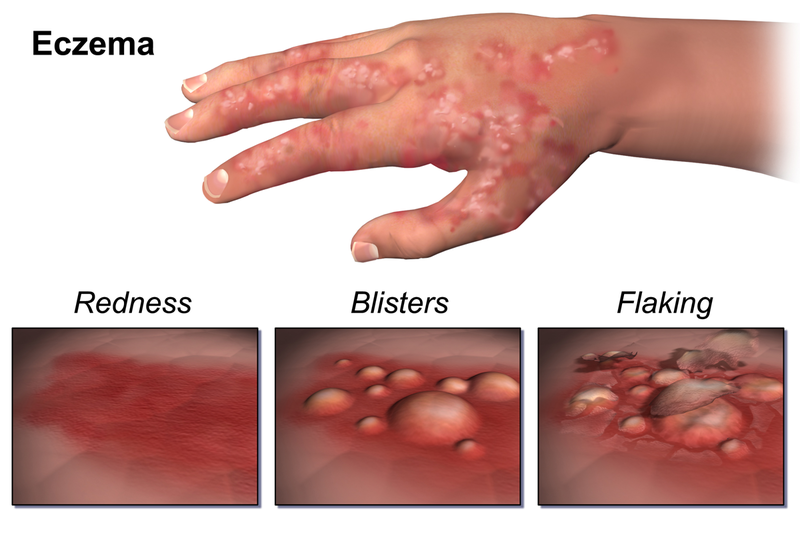
Eczema, also known as atopic dermatitis, is an inflammation of the skin seen as a rash of eruptions (Figure 9.20) that vary in severity. These itchy, irritated regions may become raw from scratching. Environmental conditions that stimulate eczema outbreaks include allergens, stress, soaps, fabrics. The condition is usually chronic but not contagious.
Hansen’s Disease
Hansen’s disease, also known as leprosy, is caused by a bacterial infection of Mycobacterium leprae (https://www.cdc.gov/leprosy/index.html). It affects not only the skin surface but also the nerves, eyes, and lining of the nasal passageway. The skin of infected persons develops thickened patches, swollen nodules, and painless ulcers on different parts of the body, including the face, ears, and soles of the feet (Figure 9.21). Due to misinformation and prejudice, persons with Hansen’s disease have been historically shunned. While the condition is mildly contagious, transmission would require months of close contact with an untreated infected person. The infection grows slowly, and symptoms appear gradually, but the condition is treatable with antibiotics. If left untreated, however, the condition can develop into permanent paralysis, the crippling of hands and feet, and disfigurement.
Louisiana has a special connection to Hansen’s Disease by being the location of the National Leprosarium (https://www.hrsa.gov/hansens-disease/museum). This facility, located in Carville, a town about 18 miles southeast of Baton Rouge, operated for over 100 years from 1894 to 2005.

Psoriasis
Psoriasis is an autoimmune disorder that appears as regions of rash-like spots on the surface of some parts of the skin. Both eczema and psoriasis share common triggers for outbreaks, but unlike eczema, the rash is not an inflammation (i.e., dermatitis). Instead, psoriasis results from rapidly dividing skin cells that pile up on the skin surface of some body regions as well-defined scaly lesions (Figure 9.22). Persons with psoriasis do not experience as intense an itching sensation as those with eczema, and this condition is also not contagious.

Test Your Knowledge
VI. Explain underlying causes of common integumentary system conditions.
- Define and explain the cause of each of the following integumentary system conditions:
-
- Acne
- Burns
- Eczema
- Hansen’s disease
- Psoriasis
Practice
For the exercise below, drag the structure names to the correct empty boxes on the figure.
For the following questions, click the correct answer choice.
Image Descriptions
Figure 9.1 image description: This illustration shows a cross-section of skin tissue. The outermost layer is called the epidermis and occupies one-fifth of the cross section. Several hairs are emerging from the surface. The epidermis dives around one of the hairs, forming a follicle. The middle layer is called the dermis, which occupies four-fifths of the cross section. The dermis contains an erector pili muscle connected to one of the follicles. The dermis also contains an eccrine sweat gland, composed of a bunch of tubules. One tubule travels up from the bunch, through the epidermis, opening onto the surface a pore. There are two string-like nerves traveling vertically through the dermis. The right nerve is attached to a Pacinian corpuscle, a yellow structure consisting of concentric ovals similar to an onion. The lowest level of the skin, the hypodermis, contains fatty tissue, arteries, and veins. Blood vessels travel from the hypodermis and connect to hair follicles and erector pili muscle in the dermis. [Return to image.]
Figure 9.3 image description: A skin section viewed under a microscope that shows extensive outer layers of compressed keratinocytes in the epidermis. Even though the magnification used is the same as Figure 9.2, all layers are noticeably thicker, and the underlying dermis is barely visible. [Return to image.]
Figure 9.4 image description: The bulk of the epidermis of the skin is composed of layers (or strata) of stratified epithelial cells. The most common cell type is the keratinocyte, but the appearance of the keratinocyte changes based on the strata. The lowermost layer, called the stratum basale, has a cell type called a melanocyte in addition to the keratinocyte. The melanocyte has tentacle-like extensions that reach up between the keratinocytes in the adjacent strata, but the main part of the cell with the nucleus remains adjacent to the membrane separating the epidermis and dermis. The stratum spinosum layer is found above the stratum basale, and the keratinocytes look different here because they have visible connections linking them together to adjacent cells. The next layer higher is called the stratum granulosum, and the keratinocytes here are filled with granules. A change in cell shape is noteworthy as the strata layers accumulate; the outermost cells are flattened in appearance, while the keratinocytes in the lower strata appear more cuboidal. The thinnest strata is the stratum lucidum that appears right above the stratum granulosum. The keratinocyte cells here still have their nuclei. In the final stratum, the outermost stratum corneum, the cells here are sloughing off from the epidermis and have lost their nuclei. [Return to image.]
Figure 9.5 image description: A skin section viewed under the microscope that shows in the interdigitation between the epidermis and dermis. Finger-like extensions of connective tissue in the papillary layer of the dermis project upward into the epidermis. This resembles fingers from two different hands woven together. Below the extensions of the papillary layer, the bulk of the dermis is made up of connective tissue that is unorganized.[Return to image.]
Figure 9.6 image description: A syringe with needle is inserted into the skin at a ninety-degree angle. The skin has been pinched into a fold so that the fatty subcutaneous layer bulges for easier insertion. The needle is completely buried into the skin, and only fat tissue cells are seen in the vicinity of the tip. Also shown is a muscular layer, but this is located far below where the injection site occurs. [Return to image.]
Figure 9.7 image description: A cross section of the skin containing a hair follicle. The follicle is teardrop shaped. Its enlarged base, labeled the hair bulb, is embedded in the hypodermis. The outermost layer of the follicle is the epidermis, which invaginates from the skin surface to envelope the follicle. Within the epidermis is the outer root sheath, which is only present on the hair bulb. It does not extend up the shaft of the hair. Within the outer root sheath is the inner root sheath. The inner root sheath extends about half of the way up the hair shaft, ending midway through the dermis. The hair matrix is the innermost layer. The hair matrix surrounds the bottom of the hair shaft where it is embedded within the hair bulb. The hair shaft, in itself, contains three layers: the outermost cuticle, a middle layer called the cortex, and an innermost layer called the medulla. [Return to image.]
Figure 9.8 image description: A hair follicle is obvious in a skin section viewed under a microscope because it shows a finger-like projection of the epidermis plunging into the underlying dermis. The epidermal region is made up of more densely packed cells than the tissue in the dermis. The deepest part of the follicle is a rounded bulb of cells that appear to ensheath the hair. While these cells are solid in appearance, they are surrounded by clusters of sebaceous glandular cells that resemble inflated sacs. [Return to image.]
Figure 9.9 image description: The anatomy of the fingernail region. The left image shows a dorsal view of a finger. The proximal nail fold is the part underneath where the skin of the finger connects with the edge of the nail. The eponychium is a thin, pink layer between the white proximal edge of the nail (the lunula) and the edge of the finger skin. The lunula appears as a crescent-shaped white area at the proximal edge of the pink-shaded nail. The lateral nail folds are where the sides of the nail contact the finger skin. The distal edge of the nail is white and is called the free edge. An arrow indicates that the nail grows distally out from the proximal nail fold. The right image shows a lateral view of the nail bed anatomy. In this view, one can see how the edge of the nail is located just proximal to the nail fold. This end of the nail, from which the nail grows, is called the nail root. [Return to image.]
Figure 9.10 image description: An illustration of an eccrine sweat gland embedded in a cross section of skin tissue. The eccrine sweat gland is a bundle of white tubes embedded in the dermis. A single white tube travels up from the bundle and opens on to the surface of the epidermis. The opening is called a pore. There are several pores on the small block of skin portrayed in this diagram. [Return to image.]
Figure 9.11 image description: An arrow points to a cluster of nerve cells that resemble a beehive. This bundle is located in a projection of the dermis up into the epidermis that causes it to be just underneath the skin’s outer surface. Most of the dermal papillary layer projections do not contain this nervous structure. The nerve cells are distinctly clearer in appearance than the denser connective tissue cells in the surrounding dermis. [Return to image.]
Figure 9.12 image description: Part A is a photo of a man skiing with several snow-covered trees in the background. Part B is a diagram with a right and left half. The left half is titled “Heat is retained by the body,” while the right half is titled “Heat loss through radiation and convection.” Both show blood flowing from an artery through three capillary beds within the skin. The beds are arranged vertically, with the topmost bed located along the boundary of the dermis and epidermis. The bottommost bed is located deep in the hypodermis. The middle bed is evenly spaced between the topmost and bottommost beds. In each bed, oxygenated blood (red) enters the bed on the left, and deoxygenated blood (blue) leaves the bed on the right. The left diagram shows a picture of snowflakes above the capillary beds, indicating that the weather is cold. Blood is only flowing through the deepest of the three capillary beds, as the upper beds are closed off to reduce heat loss from the outer layers of the skin. The right diagram shows a picture of the sun above the capillary beds, indicating that the weather is hot. Blood is flowing through all three capillary beds, allowing heat to radiate out of the blood, increasing heat loss. Part C is a photo of a man running through a forested trail on a summer day. [Return to image.]
Figure 9.13 image description: A comparison of skin from dark (left) and light (right) skin tones shows skin color variants do not differ structurally. While the number of pigment-producing melanocytes in the stratum basale is the same, more pigment is ultimately produced by darker-skinned individuals. This is seen as relatively more pigment-releasing vesicles budding off of the melanocytes and filling the keratinocytes with color. [Return to image.]
Figure 9.14 image description: A boy with albinism is seen smiling. His integument appears normal except that melanin is not produced, making the skin appear pinkish or pale. The lack of pigment does not just affect keratinocytes but is also seen where hair grows, such as eyebrows, eyelashes, and scalp. [Return to image.]
Figure 9.15 image description: A person with vitiligo is typing on a keyboard. Some fingers and parts of the palm show patches of white skin on an otherwise dark-skinned individual. The patches are irregular shaped and not uniformly distributed on the integument; for example, the exposed wrist shows no vitiligo patches. [Return to image.]
Figure 9.16 image description: A series of images showing different appearances of non-malignant common moles on the skin. These small moles are roundish in shape with a regular edge and have even coloration of pink, tan, or black skin. [Return to image.]
Figure 9.18 image description: A complex image of unburned skin (upper right) and burned skin (lower series). The unburned skin is composed of undamaged epidermis, dermis, and hypodermis layers. In the first-degree burn image (lower left), redness indicates burn damage to the outer epidermis layers but the skin. The redness and damage extends to the entire epidermis and part of the underlying dermis in a second-degree burn (lower middle). Finally, the most extensive damage and spread of redness is seen to all three skin layers; this is the third-degree burn. The third-degree burned area is the thickest in damage and has completely burned through the epidermis and dermis layers, as well as penetrating substantially into the hypodermis region. [Return to image.]
Figure 9.20 image description: A diagram of a hand from a person with eczema shows rash-like irritations compared to surrounding areas of smooth skin. The irritation progresses through Redness (lower left), Blister (lower middle), and Flaking (lower right). The images convey a rawness to the rash that makes one think of wanting to scratch this irritation; itchiness is commonly associated with areas of the skin having an eczema outbreak.[Return to image.]
Figure 9.21 image description: A boy with Hansen’s disease sits on a bed alone, not facing the camera. He has a pensive expression while waiting in a location that is presumably an institution, such as a hospital. The skin of his exposed arms and legs is covered extensively with scaly patches and crusty lesions. This condition has also affected his face, especially his cheeks and the outside of his ears. [Return to image.]
Figure 9.22 image description: The back and arms of a person with psoriasis are covered with red patches, some of which appear as raised plaques. Although visibly red in contrast with the surrounding white skin, the condition looks dry without any blistering or flaking as in eczema. [Return to image.]
An anatomically distinct structure of the body composed of two or more tissue types.
Relating to circulation of blood.
outermost tissue layer of the skin
Type of structural protein that gives skin, hair, and nails its hard, water-resistant properties.
Tissue that consists of multiple layers of cells with the most apical being flat scale-like cells; protects surfaces from abrasion.
Lacking blood vessels.
Cell that produces keratin and is the most predominant type of cell found in the epidermis.
Deepest layer of the epidermis, made of epidermal stem cells.
Layer of skin between the epidermis and hypodermis, composed mainly of connective tissue and containing blood vessels, hair follicles, sweat glands, and other structures.
The most abundant of three protein fibres found in the extracellular matrix of connective tissues.
(Plural = dermal papillae) extension of the papillary layer of the dermis that increases surface contact between the epidermis and dermis.
Developing human during the time from the end of the embryonic period (week 9) to birth.
A superficial ridge on the skin surface of fingertips that forms from the dermal papillae underlying the epidermis in this location.
Type of stem cell found in the stratum basale and in the hair matrix that continually undergoes cell division, producing the keratinocytes of the epidermis.
Cell that is oligo-, multi-, or pleuripotent that has the ability to produce additional stem cells rather than becoming further specialized.
Division of genetic material, during which the cell nucleus breaks down and two new, fully functional, nuclei are formed. Usually immediately followed by cytokinesis (cell division).
Receptor cell in the stratum basale of the epidermis that responds to the sense of touch.
Cell found in the stratum basale of the epidermis that produces the pigment melanin.
Pigment that determines the color of hair and skin.
Layer of the epidermis superficial to the stratum basale, characterized by the presence of desmosomes.
A type of anchoring junction found between adjacent epithelial cells.
A monocyte-derived phagocytic cell, functions as antigen-presenting cells in the immune system.
Specialized dendritic cell found in the stratum spinosum that functions as a macrophage.
Ameboid (irregular outline with peripheral projections) phagocyte found in several tissues throughout the body.
A molecule composed of carbohydrate and lipid components.
Layer of the epidermis superficial to the stratum spinosum.
Granulated protein found in the stratum granulosum.
Any of several different types of membrane-enclosed specialized structures in the cell that perform specific functions for the cell.
Layer of the epidermis between the stratum granulosum and stratum corneum, found only in thick skin covering the palms, soles of the feet, and digits.
Finger or toe.
Clear protein-bound lipid found in the stratum lucidum that is derived from keratohyalin and helps to prevent water loss.
Most superficial layer of the epidermis.
Describes a position closer to the surface of the body.
Connective tissue connecting the integument to the underlying bone and muscle.
Most abundant cell type in connective tissue, secretes protein fibers and matrix into the extracellular space.
A type of connective tissue proper that shows little specialization with cells dispersed in the matrix.
One of three protein fibres found in connective tissues.
Lipid storage cells.
(Also, Meissner corpuscle) receptor in the skin that responds to light touch.
Cavity or sac from which hair originates.
Part of hair that is below the epidermis anchored to the follicle.
Structure at the base of the hair root that surrounds the dermal papilla.
Smooth muscle that is activated in response to external stimuli that pull on hair follicles and make the hair “stand up.”
Secretion of an endocrine organ that travels via the bloodstream or lymphatics to induce a response in target cells or tissues in another part of the body.
Sweat gland.
Gland whose secretions are excreted by exocytosis.
Export of a substance out of a cell by formation of a membrane-bound vesicle.
Type of sweat gland that is common throughout the skin surface; it produces a hypotonic sweat for thermoregulation.
Describes a solution concentration that is lower than a reference concentration.
(Also, immunoglobulin) antigen-specific protein secreted by plasma cells.
Steady state of body systems that living organisms maintain.
Type of sweat gland that is associated with hair follicles in the armpits and genital regions.
A chemical, either secreted or excreted, that produces a social response in other individuals.
Milk-producing gland in mammals.
Wax producing gland in the ear canal.
Class of nonpolar organic compounds built from hydrocarbons and distinguished by the fact that they are not soluble in water.
Class of organic compounds that are composed of many amino acids linked together by peptide bonds.
Type of oil gland found in the dermis all over the body and helps to lubricate and waterproof the skin and hair by secreting sebum.
Encapsulated mechanoreceptor cell found in the skin that responds to pressure and touch.
Sum of all catabolic and anabolic reactions that take place in the body.
An extracellular fluid, the fluid component of blood.
Oxygen-carrying protein in erythrocytes (red blood cells).
Membrane-bound structure that contains materials within or outside of the cell.
Membrane-bound cellular organelle originating from the Golgi apparatus and containing digestive enzymes.

