College of Health
44 Relationships Between Total Knee Arthroplasty Preoperative Clinical Factors on Postoperative Recovery
Aubrey Jacobson and Jesse Christensen
Faculty Mentor: Jesse Christensen, DPT, PhD (Physical Therapy and Athletic Training, University of Utah)
Introduction
Knee osteoarthritis (KOA) is a degenerative joint disease that greatly reduces mobility and is associated with increased mortality rates in older adults [5]. While many conservative treatment options exist for managing KOA (i.e. lifestyle management, physical therapy, pharmacotherapy), a total knee arthroplasty (TKA) has been shown to be the most effective treatment for managing pain and disability [12].
A TKA can greatly reduce knee pain and improve physical function postoperatively. However, recent data has shown that abnormal gait mechanics, defined as overloading of the nonoperative knee and underloading of the operative knee, are observed even years post-TKA and are similar to those observed pre-TKA [7]. This is concerning as abnormal gait mechanics can result in a higher risk for falls, muscle imbalance, and decreased quality of life [2].
The purpose of this study is to investigate the relationship between preoperative clinical factors and abnormal gait mechanics in adults post-TKA. Specifically, we will determine if knee angle, moment, and power influence underloading of the operative joint post-TKA. We hypothesize that adults with poorer clinical factors (i.e. gait speed, residual knee pain, weakness, comorbidities) pre-TKA will have poorer gait mechanics 3 months post-TKA.
Methods
This study was conducted at the VA Salt Lake City Medical Center Gait Lab. All participants (n=25) underwent a primary unilateral TKA due to end-stage KOA. Participants completed motion analysis testing, self-reported measures (numeric pain rating scale, functional comorbidity index), and physical performance measures (40-meter walk test, maximal isometric quadriceps, and hamstring testing) preoperatively and 3 months post-TKA. Motion capture analysis (Nexus) was used to evaluate knee mechanics and inverse kinematic and dynamic solutions (Visual 3D) were conducted with traditional methods.
Tables/figures
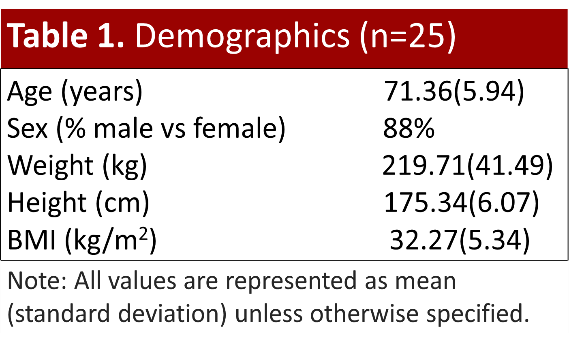
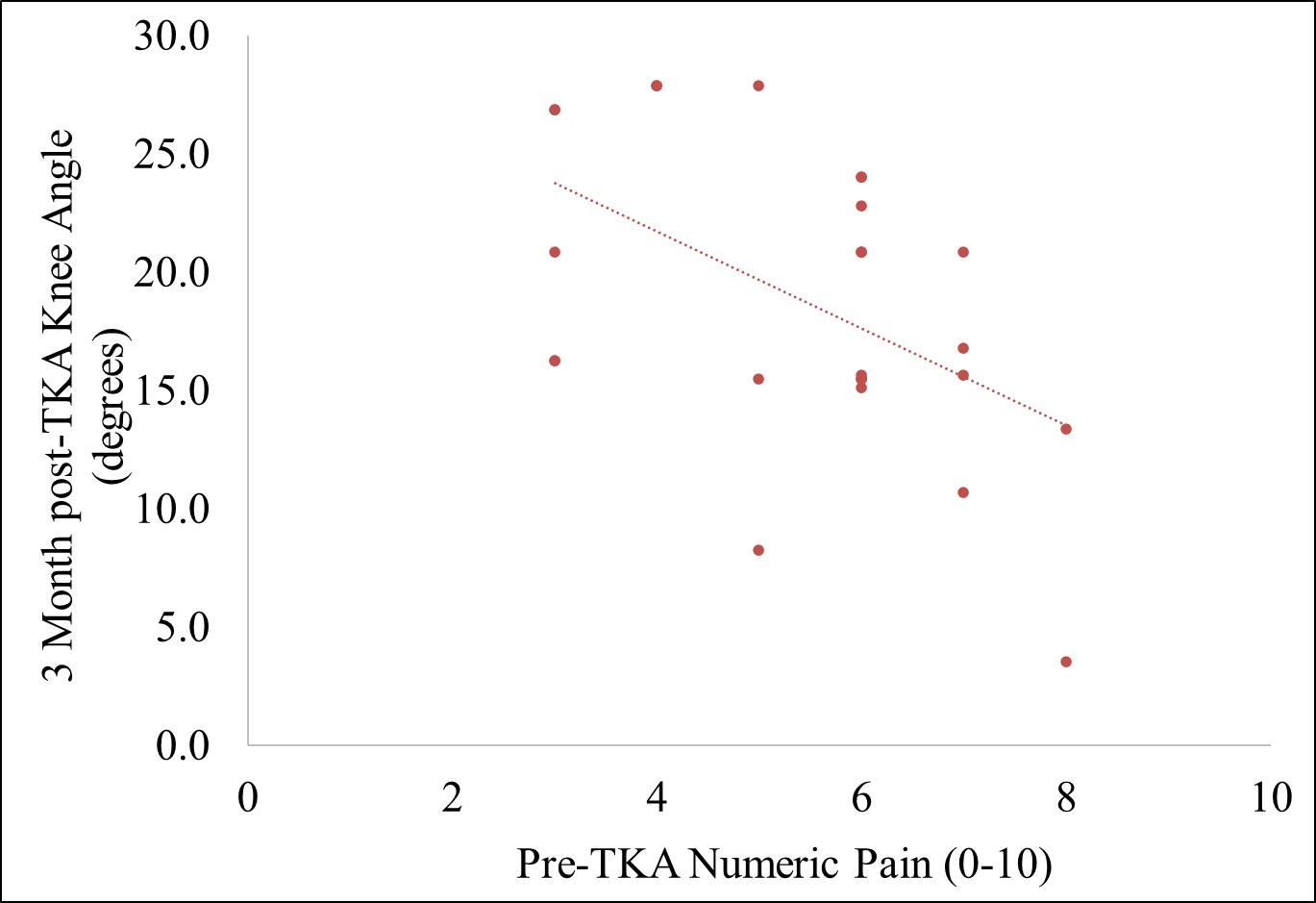
Figure 1. Relationship between preoperative numeric knee pain on surgical knee flexion angle (t=-2.82, p=0.01 r=-0.51) at weight acceptance during self-selected gait at 3 months post-TKA.
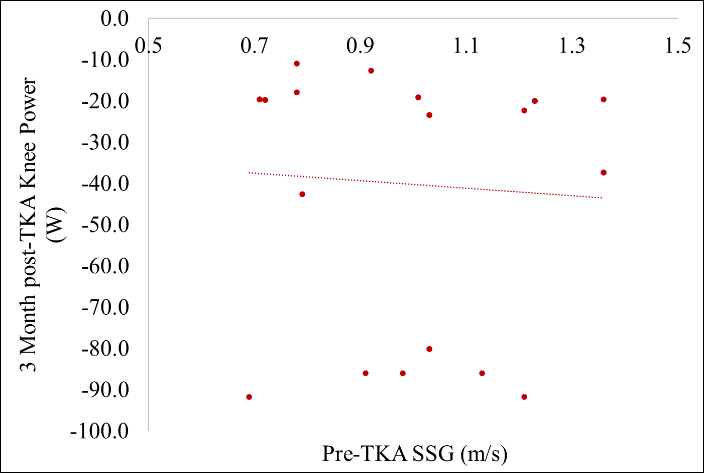
Figure 2. Relationship between preoperative gait speed on surgical knee power (t=-2.30, p=0.03 r=-0.43) during weight acceptance during self-selected gait at 3 months post-TKA.
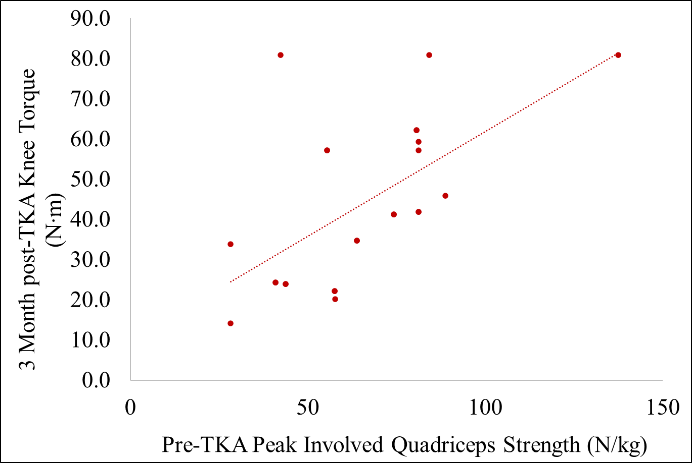
Figure 3. Relationship between preoperative peak surgical quadriceps strength on surgical knee torque (t=3.16, p=0.01 r=-0.55) during weight acceptance during self-selected gait at 3 months post-TKA.
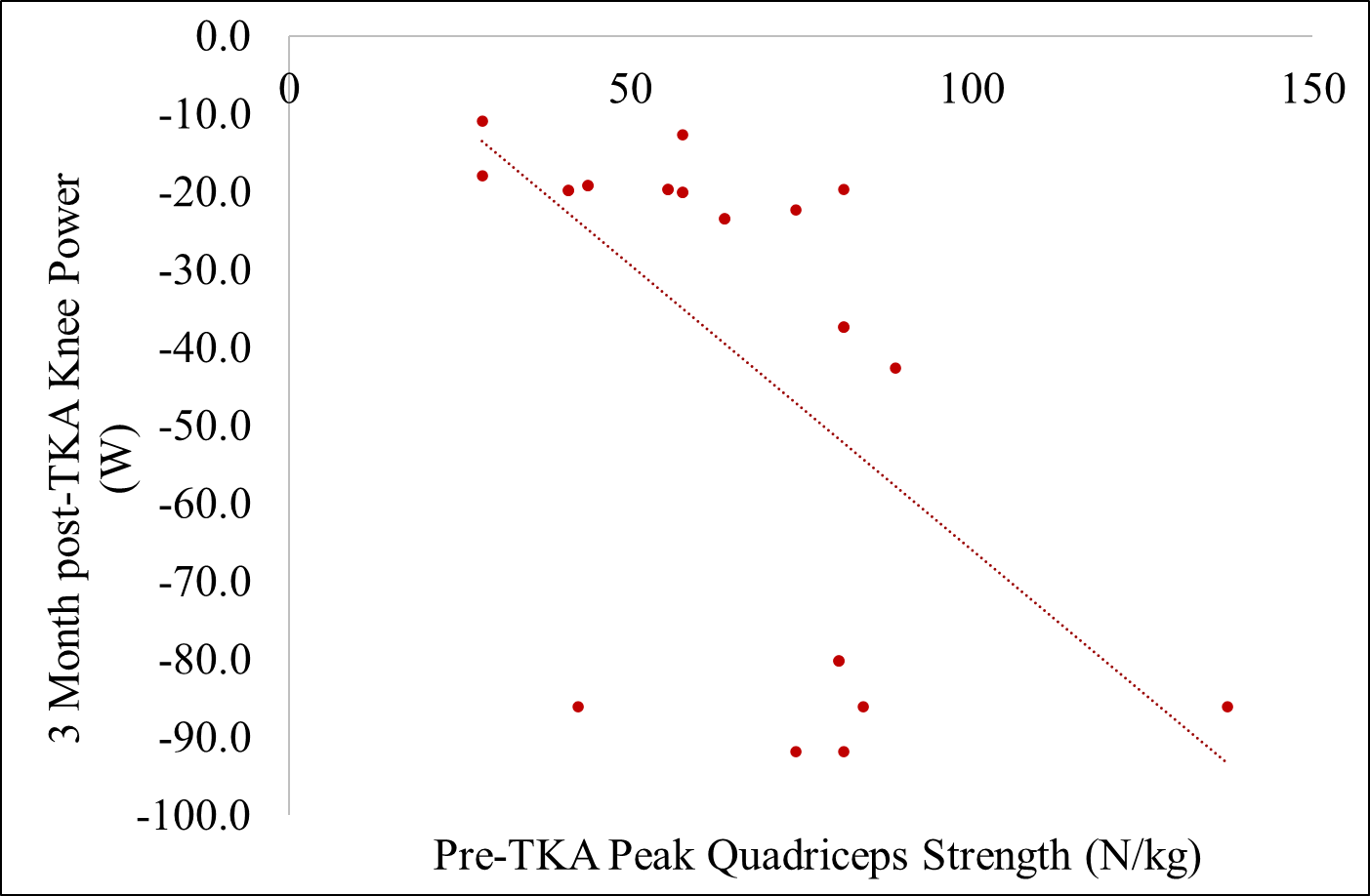
Figure 4. Relationship between preoperative peak surgical quadriceps strength on surgical knee power (t=3.09, p=0.01 r=0.54) during weight acceptance during self-selected gait at 3 months post-TKA.
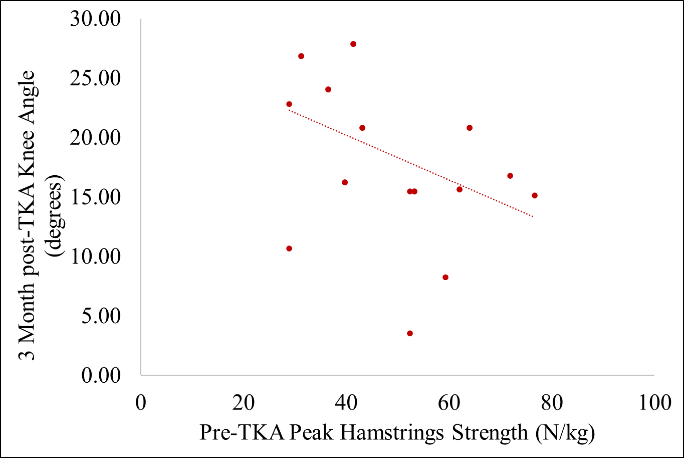
Figure 5. Relationship on preoperative peak surgical hamstring strength on surgical knee flexion (t=2.13, p=0.01 r=-0.42) angle during weight acceptance during self-selected gait at 3 months post-TKA.
Results
Increased numeric pain levels preoperatively were related to a lower knee angle at weight acceptance at 3 months post-TKA (p=0.01, t=-2.82, r=-0.51). Faster gait speeds preoperatively were related to greater knee power during weight acceptance at 3 months post-TKA (p=0.03, t=-2.30, r=-0.43). Greater quadriceps torque preoperatively were related to greater knee extensor torque during weight acceptance at 3 months post-TKA (p=0.01, t=3.16, r=-0.55). Greater quadriceps torque preoperatively was related to greater knee power during weight acceptance at 3 months post-TKA (p=0.01, t=3.09, r=0.54). Greater hamstring torque was related to less knee angle at weight acceptance at 3 months post-TKA (p=0.01, t=2.13, r=-0.42).
Discussion
The relationship between numeric pain levels and knee angle mobility may be explained by muscle guarding. This can be partially explained by the Integrated Pain Adaptation Model[6][10]. This model describes that as pain arises, it is common for the body to modify muscular activity in ways such as muscle guarding in order to protect the affected joint and prevent further injury[6][10].
The relationship between faster gait speed and increased knee power is likely the result of faster movements requiring greater muscle activation, which results in increased power production [8][11]. This is also consistent with the relationships between increased quadriceps strength and knee extension torque and quadriceps strength and knee power during weight acceptance of the gait cycle. Power is the product of torque and angular velocity. Torque reflects the force applied, while speed (angular velocity) determines how quickly that force is applied. Together, they equal the total power produced.[8][9][11].
Increased hamstring strength was related to reduced knee angle mobility. One possible reason for this is the formation of scar tissue. This can limit joint flexibility and range of motion[3]. Another possible reason is muscle adaptations (inhibition of muscle activation, muscle guarding)[4] during recovery of a TKA. It is possible for this to lead to increased stiffness or changes in neuromuscular control, resulting in reduced mobility despite the increase in muscle strength[1][3][4].
My study provides preliminary data suggesting increased quadriceps strength, faster gait speeds, and lower pain levels preoperatively will potentially result in improved biomechanical outcomes at 3 months post-TKA. These findings indicate that pre-TKA physical function plays a crucial role in post-TKA recovery. This evidence may assist clinicians in developing prehabilitation programs and improving patient education pre-TKA. Thus, contributing to more informed decision-making and better long-term outcomes post-TKA.
References
- An, J., Cheon, S.-J., & Lee, B.-H. (2024). The effect of combined balance exercise on knee range of motion, balance, gait, and functional outcomes in acute phase following total knee arthroplasty: a single-blind randomized controlled trial. Medicina, 60(9), 1389. https://doi.org/10.3390/medicina60091389
- Ataullah, A. H. M., & De Jesus, O. (2024). Gait disturbances. In StatPearls. StatPearls Publishing.
- Bong, M. R., & Di Cesare, P. E. (2004). Stiffness after total knee arthroplasty. The Journal of the American Academy of Orthopaedic Surgeons, 12(3), 164–171. https://doi.org/10.5435/00124635-200405000-00004
- Cavanellas, N. T., Cossich, V. R. A., Nicoliche, E. B., Martins, M. B., Sousa, E. B., & Salles, J. I. (2018). Comparative analysis of quadriceps and hamstrings strength in knee osteoarthritis before and after total knee arthroplasty: a cross-sectional study. Revista brasileira de ortopedia, 53(2), 158–164. https://doi.org/10.1016/j.rboe.2018.02.009
- Cleveland, R. J., Nelson, A. E., & Callahan, L. F. (2019). Knee and hip osteoarthritis as predictors of premature death: A review of the evidence. Clinical and Experimental Rheumatology, 37(Suppl 120(5)), 24–30.
- Graven-Nielsen, T., Svensson, P., & Arendt-Nielsen, L. (1997). Effects of experimental muscle pain on muscle activity and co-ordination during static and dynamic motor function. Electroencephalography and Clinical Neurophysiology/Electromyography and Motor Control, 105(2), 156-164.
- Marino, G., De Capitani, F., Adamo, P., Bolzoni, L., Gatti, R., & Temporiti, F. (2024). Long-term gait analysis in patients after total knee arthroplasty: A systematic review and meta-analysis. Gait & Posture, 113, 75–98. Advance online publication. https://doi.org/10.1016/j.gaitpost.2024.06.002
- National Strength and Conditioning Association. (2017, June 1). Muscle activation and strength training.
- https://www.nsca.com/education/articles/kinetic-select/muscle-activation-and-strength-training
- Ottinger, C. (2020). Biomechanics and growth. The Muscle PhD. https://themusclephd.com/biomechanics-and-growth/#:~:text=Therefore%2C%20since%20po wer%20is%20W,major%20impact%20on%20muscle%20size.
- Peck, C. C., Murray, G. M., & Gerzina, T. M. (2008). How does pain affect jaw muscle activity? The Integrated Pain Adaptation Model. Australian Dental Journal, 53(3), 201–207. https://doi.org/10.1111/j.1834-7819.2008.00050.x
- Pojednic, R. M., Clark, D. J., Patten, C., Reid, K., Phillips, E. M., & Fielding, R. A. (2012, May 22). The specific contributions of force and velocity to muscle power in older adults. Experimental Gerontology. https://pubmed.ncbi.nlm.nih.gov/22626972/
- Zhang, Y., & Liu, H. (2021). Safety of total knee arthroplasty in the treatment of knee osteoarthritis and its effect on postoperative pain and quality of life of patients. Contrast Media & Molecular Imaging, 2021, 6951578. https://doi.org/10.1155/2021/6951578
About the authors
name: Aubrey Jacobson
name: Jesse Christensen
institution: University of Utah

