College of Health
42 Exploring the Relationship Between Muscle Strength and Knee Joint Biomechanics in Patients With Knee Osteoarthritis
Maddie Hopkins
Faculty Mentor: Jesse Christensen (Biomedical Engineering, University of Utah)
Abstract
One of the most widespread causes of global disability and impairment is osteoarthritis, and the knee is the joint most commonly affected. Substantial research has been done on knee osteoarthritis (KOA). According to current research, patients with KOA exhibit weakness in their knee extensor muscles, even if there is no visible muscle loss or reports of pain. There is limited knowledge about the relationship between skeletal muscles and joint biomechanics in KOA. This study hypothesized a significant relationship between poor knee biomechanics and weakened knee extensors in patients with KOA. To test this relationship, kinematic data was collected from KOA patients during step-up and step-down tasks as well as knee extensor strength data during a knee extension task. The results of this study show a strong correlation between increased knee extension moment and increased knee extensor strength. In addition, there was a strong correlation between increased knee extension power and increased knee extensor strength. The results also revealed that greater knee flexion angle was correlated with decreased knee extensor strength. These potential relationships suggest that stronger quadriceps may help support the knee joint, enhance overall joint function, and relieve pain during movement. They inform how muscle strength can interact with knee biomechanics in a KOA patient population and support the use of muscle strengthening as a promising strategy to manage KOA.
Introduction
Osteoarthritis is a degenerative joint condition that can significantly impact quality of life and the ability to perform daily activities [1]. Knee osteoarthritis (KOA) has been described as the deterioration of cartilage within the joint surface [2]. Growing evidence suggests that the loss of skeletal muscle function may precede cartilage degradation and could be the underlying cause of reduced mobility and abnormal knee biomechanics [2-4]. A significant challenge in managing the disease is the lack of understanding regarding how muscle dysfunction interacts with joint mechanics.
Extensive research has been conducted on KOA. However, there is limited data regarding the relationship between skeletal muscles and knee biomechanics in patients with KOA. Direct relationships have shown that modified loading mechanisms, increased mechanical stresses, and changes in biomechanics impact the onset and worsening of osteoarthritis [5]. Additionally, studies have shown that quadriceps weakness is observed in patients with KOA, even if muscle atrophy or joint pain is absent [6]. Increased functional impairment is connected to quadriceps weakness, emphasizing the importance of skeletal muscle strength in preserving joint health [6]. Despite these conclusions, the relationship between poor quadriceps strength and abnormal knee biomechanics in KOA is unknown.
In order to explore this possible relationship, quadriceps strength and motion capture data will be collected and processed from patients with knee osteoarthritis. Vicon Nexus and Visual 3D software, along with MATLAB code, will be used to process the data and pinpoint clinically essential patterns. The aim is to uncover valuable information about muscle dysfunction and joint mechanics. This study hypothesizes a significant correlation between quadriceps weakness and altered knee biomechanics in patients with KOA.
Understanding the relationship between muscle dysfunction and knee joint biomechanics will enable the development of more effective treatments and specialized therapies, ultimately improving patient outcomes. This research may also contribute to better management of KOA by physicians, clinicians, and therapists, which would delay the disease’s progression and improve patients’ quality of life. Overall, the results will greatly contribute to the understanding of osteoarthritis, which could be key for disease prevention and intervention efforts.
Background
Understanding osteoarthritis from a broader context is critical to understanding its impact on joint health and function. Osteoarthritis is a progressive disease involving the entire joint caused by a combination of general risk factors, such as age or injury, mechanical stresses and unusual joint mechanics [7]. One of the most common causes of impairment and disability globally is osteoarthritis, particularly in older adults [7]. The knee is the joint most commonly affected by osteoarthritis [7]. There is currently no cure for osteoarthritis, so treatment of the disease involves symptom management and delaying disease progression [7]. Patients with osteoarthritis experience joint stiffness and pain, which significantly impairs their ability to perform daily activities of living, such as walking, standing up from sitting, and climbing stairs [7].
In the early stages of osteoarthritis, the articular cartilage develops surface fibrillation, irregularities, and erosion that progressively spread to the bone as the disease worsens [8]. Articular cartilage lines the ends of bones to create joints. This helps the bones to glide smoothly as the leg extends and bends, and helps absorb shock [8]. Along with the cartilage and bony structure, soft tissues, such as ligaments, menisci, and joint capsules, are also affected [8].
Another factor that advances the onset of the disease is elevated mechanical stress and loading on the knee, which is frequently caused by weakened muscles [8]. Adding friction and joint instability worsen the disease as cartilage breaks down and soft tissues change. The addition of muscle weakness exasperates the disease and contributes to the lack of support of the joint.
It is speculated that structural damage and symptoms associated with osteoarthritis result from improper mechanical loading [9]. Joint tissues are subjected to mechanical stress during movement and this force can contribute to osteoarthritic processes [9]. Joint mechanics in patients with KOA are abnormal, which causes increased strain on the joint and unusual movement. This furthers cartilage degradation and can increase joint pain and deterioration.
Current studies on knee kinematics focus primarily on external knee joint moments, which include knee adduction moment (KAM), knee flexion moment (KFM), and knee rotation moment (KRM) during gait analysis [10]. According to prior studies, patients with KOA have substantial varus deformities during gait analysis [11]. This means that their knees predominantly angle inward while walking. They found that KOA patients experience a larger KAM and smaller KFM, showing elevated strain on the medial side of the knee and potentially weakened muscles near the joint [10]. Other studies reveal additional abnormal knee kinematics, such as increased joint reaction forces and reduced knee flexion angles, which further contribute to the deterioration of cartilage [11-12]. These biomechanical abnormalities suggest that knee osteoarthritis is a mechanical issue compromising joint function while also being a progressive cartilage disease.
Preserving knee stability and controlling joint movement largely depends on the muscles near the joint, specifically the quadriceps and hamstrings. Adequate muscle strength enables proper absorption of forces, which mitigates stress on the knee joint. The muscles surrounding the knee greatly affect joint mechanics. Therefore, weakness in those muscles can contribute to the worsening of KOA [12]. Patients with KOA often experience muscle weakness without noticeable muscle atrophy or joint pain [6]. There is a strong connection between severe functional impairment of the knee and weak quadriceps muscles. This implies that muscle dysfunction develops relatively early in the onset of the disease, indicating its importance [6].
In regards to knee mechanics, the connection to quadriceps weakness remains unclear. A previous study indicates that there is not a linear relationship between lower limb muscle strength and knee joint movements in patients with KOA [11]. However, despite the lack of a definitive relationship, researchers maintain that lower limb muscles possibly influence the knee’s biomechanics during gait [11]. Other studies have reached similar tentative conclusions but have yet to explore additional kinematic variables and tasks, such as stairs, as the majority of these studies involve gait analysis [11-12]. Further research must be conducted to fully comprehend these mechanisms and determine a connection between knee joint mechanics and muscle strength.
Methods
Patient Population
This IRB approved study consisted of a patient population of eight male, veteran KOA patients from ages 50-75 years old. Each patient had a Kellgren and Lawrence classification of osteoarthritis severity in the knee joint of grade I or greater. Proper consent was obtained from each participant before the trials were conducted.
Motion Capture Data Collection
Each patient performed three trials of step-up and stepdown tasks during the data collection process. These tasks were selected because they place a high demand on the knee and simulate stair navigation, which is a challenging task for patients with KOA. The motion capture data was collected using VICON Nexus, a 24-camera motion analysis system. To measure the ground reaction forces during the tasks, force plates were used. Reflective markers were placed on important anatomical landmarks, specifically bony prominences, on the patients during collection. The cameras in the Vicon system captured the various locations of these markers and then triangulated their positions to generate of 3D model of motion. Quadriceps strength data was collected for all patients during a knee extension task using a System 4 Biodex, which is a computerized measuring device for measuring muscle strength. The kinematic data collected for each patient during the stair tasks includes: frontal and sagittal plane knee joint angles, moments and power.
Kinematic Data Processing
After collection, the kinematic data for each trial was processed in VICON Nexus software to access data quality. The data was checked for potential gaps, as small gaps in certain markers can occur due to anatomical variations among patients. Any gaps present were filled in VICON Nexus using data from adjacent markers located in comparable anatomical positions. Once the data had been checked and cleaned, it was transferred to the Visual 3D software. In Visual 3D, the data was processed through pipelines to generate graphs and reports of kinematic variables for each trial. Using code written in Visual 3D, biomechanical variables of interest were extracted for further analysis. Key variables included knee angle, knee moment and knee power. The maximum values in the sagittal plane and frontal plane for all trials and all variables were pinpointed during this extraction. These values were exported and put into MATLAB.
Statistical Analysis
MATLAB code was used to average the maximum values for the tasks for each patient and each variable. These values were then compared to average quadriceps strength for each patient. To check for normality in the data, the Lilliefors test was used in MATLAB, and all data was found to be normally distributed, so parametric statistical analysis was conducted in MATLAB. This included the use of Pearson correlation to evaluate potential relationships between the variables and quadriceps strength. Statistical significance for the Pearson correlation analyses was determined by a p-value less than 0.05. R2 values to indicate the amount of variance in quadriceps strength related to the other corresponding variables were also calculated in MATLAB.
Results
In eight patients with KOA, we measured quadriceps strength and estimated a large set of knee joint biomechanical variables from the stair task data. We analyzed the correlation between quadriceps strength and a subset of biomechanical variables including maximum knee extension moment, maximum knee extension power and maximum knee flexion angle.
For maximum knee extension moment, the results show a positive correlation to quadriceps strength during a step-up task. Patients with greater quadriceps strength exhibited a greater rotational force as they straightened their leg while ascending the stair. To quantify the strength of this relationship, the Pearson correlation coefficient (r) was calculated to be 0.884 (Fig. 1).
According to established guidelines, a correlation closer to 1 signifies a strong, positive correlation. This correlation coefficient suggests that that increased knee extension moment is strongly correlated to increased quadriceps strength. The p-value of 0.004, which is well below the accepted threshold of 0.05, confirms the statistical significance of this relationship (Fig. 1).
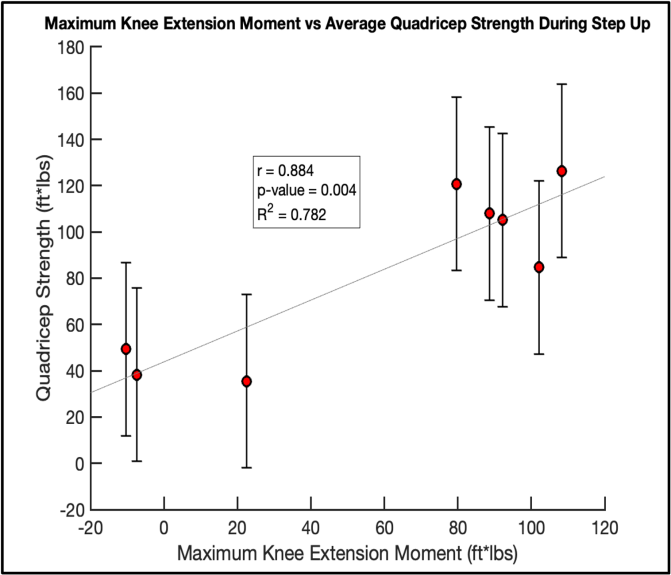
Figure 1. Direct relationship between maximum knee extension moment and maximum quadriceps strength during step-up task. Error bars represent standard deviation of quadriceps strength measurements for each individual patient.
For maximum knee extension power, the results show a positive correlation to quadriceps strength during a step-up task. When ascending the stair, the patients with greater quadriceps strength exerted greater power when straightening their leg. The Pearson correlation coefficient (r) for this relationship was 0.879 (Fig. 2). This correlation coefficient is close to 1, which shows a strong, positive correlation. This indicates that increased knee extension power is strongly correlated to increased quadriceps strength. The p-value for this relationship was 0.004 and supports its statistical significance (Fig. 2).
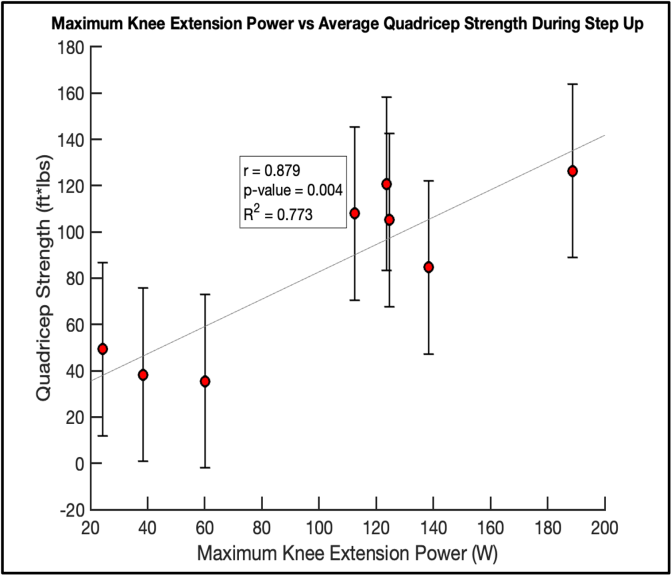
Figure 2. Direct relationship between maximum knee extension power and maximum quadriceps strength during step-up task. Error bars represent standard deviation of quadriceps strength measurements for each individual patient.
For the maximum knee flexion angle, there was a negative correlation to quadriceps strength. As quadriceps strength decreased, the maximum knee flexion angle exerted during the step-down task increased. Patients with weaker quadriceps strength had a greater bend in their knee while descending a stair. The Pearson coefficient for this relationship was calculated to be -0.924 (Fig. 3). According to established guidelines, a correlation coefficient closer to -1 signifies a strong, negative correlation. This correlation coefficient suggests that a greater knee flexion angle is correlated to decreased quadriceps strength during a step-down task. The p-value of 0.001 shows a statistically significant relationship between decreased quadriceps strength and increased knee flexion angle (Fig. 3).
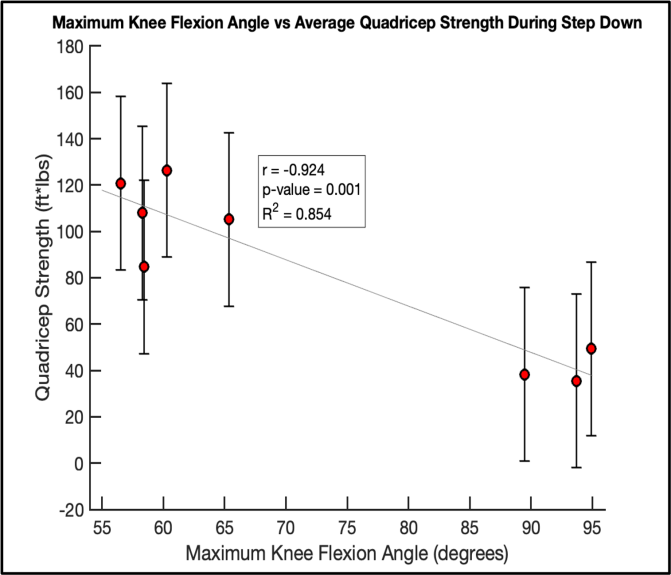
Figure 3. Inverse relationship between maximum knee flexion angle and maximum quadriceps strength during step-down task. Error bars represent standard deviation of quadriceps strength measurements for each individual patient.
Discussion
Osteoarthritis is one of the most prominent causes of global disability and impairment. Knee osteoarthritis (KOA) primarily affects the cartilage and soft tissues surrounding the knee joint, but many patients with this condition also experience muscle weakness. This study aimed to investigate the relationship between knee joint biomechanics and quadriceps strength in patients with KOA. Kinematic data during step-up and stepdown tasks was collected from KOA patients and processed in comparison to knee extensor strength data. The results from this study show strong correlations between multiple biomechanical variables and quadriceps strength. These results reveal valuable information regarding the interaction between joint mechanics and muscle dysfunction, and indicate potential value in using quadriceps strengthening to aid in managing KOA.
As quadriceps strength increased, a corresponding increase in knee extension moment was observed during a step-up task (Fig. 1). The knee extension moment is the rotational force produced by the muscles surrounding the knee joint, primarily the quadriceps, when straightening the leg [13]. Existing research states that KOA patients often have reduced knee extension moments compared to patients without KOA due to joint instability and stiffness [13]. Reduced knee extension moments can negatively impact joint mechanics by inhibiting the ability to fully extend the leg, which subsequently affects gait patterns and increases joint stress [13]. The observed results highlight the crucial role of quadriceps strength in enhancing torque production at the knee joint. The findings in Figure 1 suggest that strengthening the quadriceps may directly improve knee extension moment, potentially mitigating mechanical deficits.
Additionally, increased quadriceps strength was correlated with increased knee extension power during a step-up task (Fig. 2). Knee extension power is defined as the capacity of the muscles surrounding the joint to generate force efficiently during movement [14]. Efficient generation of force is essential for actions such as walking, stair-climbing and standing up from sitting. Current research shows that KOA patients experience deficiencies in knee extension power, in addition to decreased quadriceps strength, which leads to increased pain and reduced functional mobility [14]. Changes in knee extensor strength are not directly connected to the progression of osteoarthritis [14]. However, based on the findings of this study, strengthening the quadriceps could increase power production, and possibly help improve mobility and reduce pain during high demand movements.
Patients with KOA typically have decreased range of motion in knee flexion, likely associated with the quadriceps avoidance strategy, which is an attempt to decrease quadriceps force to alleviate pain and joint loading [15]. Reduced knee flexion angles are common in KOA patients and the degree of severity of KOA is correlated with knee flexion angle [15]. However, the results of this study show an increase in knee flexion angle connected to a decrease in quadriceps strength during a stepdown task. This is likely due to a momentum strategy in that patients with weaker quadriceps are unable to control their descent down the stairs leading to an excessive bend in the knee. Although these results are statistically correlated, the relationship remains unclear and requires further investigation due to contradictions with existing literature.
Although strong correlations are present between various biomechanical variables and quadriceps strength, the results could be limited. The sample size of patients is relatively small, and may not be generally applicable to a larger population with KOA as the patient population in this study were solely male veterans. Other biomechanical variables including frontal plane moment, front plane power, and knee adduction angle did not show strong correlations. Another limitation is the variability among patients with different grades of Kellgren and Lawrence classification of osteoarthritis severity [16]. While each patient had a classification of grade I or higher, indicating that joint space narrowing is present [16], limiting the patient population to include patients with more comparable and severe grades could lead to more relevant results.
The findings of this study provide valuable information on how knee biomechanics and muscle strength can interact in a patient population with KOA. While further investigation should be done regarding these proposed relationships, the use of quadriceps strengthening to manage KOA is a promising strategy. These results suggest that quadriceps strengthening could help stabilize the knee joint, alleviate pain during movement and improve mobility. This would contribute to improved patient outcomes and further research could help refine this potential treatment strategy.
Future work will continue to explore the relationship between knee biomechanics and muscle strength. A key priority is to expand the sample size to include more KOA patients in this study. This expansion will include a greater number of both male and female participants. This would allow for a comprehensive analysis of potential sex-specific differences in the interplay between knee joint biomechanics and muscle strength. Additionally, hip and ankle kinematics from patients with KOA will be analyzed in relation to knee joint biomechanics and muscle strength to identify possible areas of movement compensation and other potential relationships.
While additional research should be conducted to confirm and expand upon the findings of this study, it has the potential to enhance existing therapies of KOA. The use of strength training as a method of KOA management could not only help minimize pain and improve physical function, but could also reduce reliance on more invasive treatments. This ultimately could improve understanding of the condition as a whole, and enhance the quality of life of patients with KOA.
Acknowledgement
Thank you to Dr. Jesse Christensen and The Gait Lab at the VA Salt Lake City Health Care System, affiliated with the University of Utah. Additionally, thank you to the Undergraduate Research Opportunities Program.
Bibliography
Centers for Disease Control and Prevention, “Osteoarthritis,” Centers for Disease Control and Prevention, June 12, 2023. [Online]. Available: https://www.cdc.gov/arthritis/osteoarthritis/index.html. 5
A. H. Alnahdi, J. A. Zeni, and L. Snyder-Mackler, “Muscle impairments in patients with knee osteoarthritis,” Sports Health, vol. 4, no. 4, pp. 284–292, Jul. 2012, doi: 10.1177/1941738112445726.
M. V. Hurley, D. L. Scott, J. Rees, and D. J. Newham, “Sensorimotor changes and functional performance in patients with knee osteoarthritis,” Ann. Rheum. Dis., vol. 56, no. 11, pp. 641–648, Nov. 1997.
S. C. O’Reilly, A. Jones, K. R. Muir, and M. Doherty, “Quadriceps weakness in knee osteoarthritis: the effect on pain and disability,” Ann. Rheum. Dis., vol. 57, no. 10, pp. 588–594, Oct. 1998, doi: 10.1136/ard.57.10.588.
C. Egloff et al., “Biomechanics and pathomechanisms of osteoarthritis,” Swiss Med. Wkly., Jul. 19, 2012, doi: 10.4414/smw.2012.13583.
C. Slemenda, “Quadriceps weakness and osteoarthritis of the knee,” Ann. Intern. Med., vol. 127, no. 2, p. 97, Jul. 15, 1997, doi: 10.7326/0003- 4819-127-2-199707150-00001.
G. A. Hawker, “Osteoarthritis is a serious disease,” Clin. Exp. Rheumatol., vol. 37, Suppl. 120, no. 5, pp. 3–6, 2019.
R. Sen and J. A. Hurley, “Osteoarthritis,” in StatPearls [Internet] . Treasure Island, FL: StatPearls Publishing, 2024. [Online]. Available: https://www.ncbi.nlm.nih.gov/books/NBK482326/.
L. E. Diamond, T. Grant, and S. D. Uhlrich, “Osteoarthritis year in review 2023: Biomechanics,” Osteoarthritis and Cartilage, vol. 32, no. 2, pp. 138–147, 2024.
Y. Suzuki et al., “Assessing knee joint biomechanics and trunk posture according to medial osteoarthritis severity,” Scientific Reports, vol. 13, no. 1, p. 19186, 2023, doi: 10.1038/s41598-023-46486-1.
S. Farrokhi, C. A. Voycheck, J. A. Gustafson, G. K. Fitzgerald, and S. Tashman, “Knee joint contact mechanics during downhill gait and its relationship with varus/valgus motion and muscle strength in patients with knee osteoarthritis,” The Knee, vol. 23, no. 1, pp. 49–56, 2016.
A. M. Murray, A. C. Thomas, C. W. Armstrong, B. G. Pietrosimone, and M. A. Tevald, “The associations between quadriceps muscle strength, power, and knee joint mechanics in knee osteoarthritis: A cross-sectional study,” Clin. Biomech., vol. 30, no. 10, pp. 1140–1145, 2015.
T. Fukaya, H. Mutsuzaki, and K. Mori, “Relations between external moment and movement of the knee joint during the stance phase in patients with severe knee osteoarthritis,” J. Orthop., vol. 16, no. 1, pp. 101–104, Jan. 2019, doi: 10.1016/j.jor.2018.12.014.
K. M. Calder, S. M. Acker, N. Arora, K. A. Beattie, J. P. Callaghan, J. D. Adachi, and M. R. Maly, “Knee power is an important parameter in understanding medial knee joint load in knee osteoarthritis,” Arthritis Care Res. (Hoboken), vol. 66, no. 5, pp. 687–694, May 2014, doi: 10.1002/acr.22223.
Y. Kuroyanagi, T. Nagura, H. Matsumoto, T. Otani, Y. Toyama, and Y. Suda, “Weight-bearing flexion angle correlates significantly with severity of knee osteoarthritis,” Knee, vol. 16, no. 5, pp. 371–374, Oct. 2009, doi: 10.1016/j.knee.2009.01.003.
M. D. Kohn, A. A. Sassoon, and N. D. Fernando, “Classifications in brief: Kellgren-Lawrence classification of osteoarthritis,” Clin. Orthop. Relat. Res., vol. 474, no. 8, pp. 1886–1893, Aug. 2016, doi: 10.1007/s11999-016-4732-4.

