6 Electronic Health Records and Clinical Decision Support
Laura K. Garner-Jones
Chapter 6 Overview
- Electronic Health Records (EHR)
- Challenges with EHRs
- Clinical Decision Support Systems (CDSS)
- Nurses bridging the gap
Introduction
As healthcare continues to evolve in the digital age, the role of technology in clinical settings has expanded exponentially. Building on the foundational concepts of Health Information Technology (Health IT) introduced in Chapter 2, this chapter takes a closer look at one of its most transformative tools: the electronic health record (EHR). EHRs have become integral to modern healthcare by digitizing patient information, streamlining documentation, and supporting informed clinical decisions. Their widespread adoption has reshaped the way care is delivered, coordinated, and evaluated. In this chapter, we will explore the core functions of EHRs, their benefits and challenges, and the vital role nurses play in ensuring that EHR systems support safe, efficient, and patient-centered care.
More information on Health IT from the Office of the National Coordinator for Health Information Technology
Electronic Health Records (EHR)
An electronic health record (EHR) is software that’s used to securely document, store, retrieve, share, and analyze information about individual patient care. An EHR is a dynamic and patient-centered digital record system that provides instant and secure access to comprehensive health information for authorized individuals in real-time. EHRs are digital versions of patients’ paper charts and are fundamental to modern healthcare operations. The EHR can include, but is not limited to, medical history, diagnoses, medications, immunizations, allergies, treatments, and various provider documentation. EHRs help providers easily track patients from one point of care to another and document the care each patient receives (Office of the National Coordinator for Health IT, 2020).
Compared with paper records, EHRs have transformed healthcare delivery by facilitating patient care, enhancing care coordination, improving diagnostics, and improving care quality, patient outcomes, and safety. Some automated functions that improve patient care include:
- Electronic prescribing
- Drug-drug interaction checks
- Drug-allergy interaction checks (Office of the National Coordinator for Health IT, 2020).
Moreover, EHR systems streamline practice efficiencies and generate cost savings. EHR systems have transformed how healthcare data is managed and viewed, providing seamless access to patient information whenever and wherever it’s needed in a user-friendly format. This digital transformation in medicine underscores the importance of leveraging technology to optimize healthcare delivery and compensation.
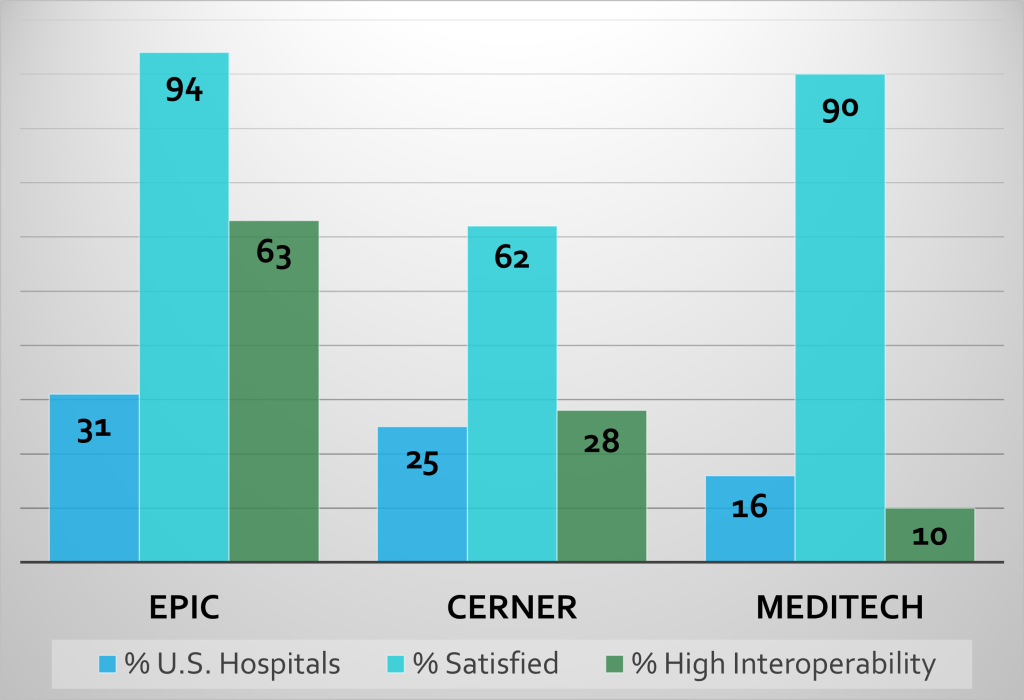
According to the Assistant Secretary for Technology Policy (ASTP), over 75% of office-based clinicians and 96% of hospitals in the United States use a certified EHR (Office of the National Coordinator for Health IT, 2021). That means nearly all practices have an immediate, practical interest in improving the efficiency and use of their EHRs. Additionally, some practices may be considering replacing their current EHR for a number of reasons, such as improving care coordination, reducing administrative burden on healthcare providers, or adapting to an organizational change like a merger with another health system (See Graph 6.1 for the top three EHRs utilized in the U.S.).
Graph 6.1 – Top Three EHRs utilized in the U.S.
Core Functions of EHRs
EHR systems offer a comprehensive solution to healthcare data management, extending beyond basic clinical information typically found in a provider’s office. Core functions of EHRs include capturing and storing health information such as medical histories, diagnoses, medications, treatment plans, immunization dates, allergies, radiology images, and laboratory and test results. They facilitate real-time, patient-centered records that make information available instantly and securely to authorized users. A significant advantage of EHRs is that they support other care-related activities directly or indirectly through various interfaces, including evidence-based decision support, quality management, and outcomes reporting (Office of the National Coordinator for Health Information Technology (ONC), n.d.c). Additionally, EHRs are designed to streamline the workflow in healthcare settings and enable comprehensive statistical reporting in compliance with health regulations.
The core functions with associated benefits of EHRs are:
-
- Health Information and Data: EHRs collect clinical data regarding patients’ diagnoses, allergies, lab test results, and medications. This foundational function ensures a holistic view of a patient’s health history. Timely access to medical history, test results, and treatment plans enhances decision-making and patient outcomes.
- Result Management: EHRs streamline the organization and accessibility of test and lab results. Timely access to these critical data points aids in informed decision-making by healthcare providers.
- Order Management: EHRs facilitate medical orders, including prescriptions, referrals, and diagnostic tests. By automating order management, EHRs enhance workflow efficiency, decrease costs, and reduce errors. An example of order management is “standing order sets” used for the management of common conditions such as pneumonia, chest pain, and stroke (Alexander et al., 2019).
- Decision Support: EHRs offer evidence-based tools to guide clinical decisions, like clinical practice guidelines and best-practice protocols. These tools improve care quality and patient outcomes by providing relevant information at the point of care. In addition, EHRs facilitate data-driven diagnoses by aggregating clinical information. Real-time alerts and decision support tools aid in early detection and evidence-based interventions.
- Electronic Communication and Connectivity: EHRs bridge gaps and enable secure data exchange between care providers, which enhances collaboration and care coordination across settings. Coordinated care plans, medication reconciliation, and referrals lead to better continuity of care.
- Patient Support: EHRs empower patients through health management tools like patient portals. Patients can actively engage in their care by accessing their health information. Access to personal health records fosters informed decision-making and shared decision processes.
- Administrative Processes and Reporting: EHRs simplify administrative tasks such as billing, scheduling, and documentation. Efficient administrative processes contribute to overall practice management.
- Data Analysis and Reporting for Public Health: EHRs also play a role in quality improvement and population health. EHRs can process large amounts of data and then be analyzed for quality improvement initiatives or reported for public health initiatives like disease surveillance and research.
(Green, 2023; ONC, n.d.a; ONC, n.d.c; ONC, 2020).
Data Analysis Example
An example of data being pulled from an EHR system to improve practice is the Braden Pressure Sore Risk Assessment (BPSRA). Embedding the BPSRA into an admission assessment at a hospital in Florida resulted in an improved pressure rate of 4.8%, half the national average (Alexander et al., 2019).
In summary, EHRs are not only repositories of patient information but also have powerful tools that enhance decision-making, streamline workflows, and ultimately contribute to better patient outcomes.
Challenges with Electronic Health Records
There are many challenges when adopting an EHR. Some unintentional consequences when adopting these systems can be disrupted workflows that increase the clerical burden on the provider by including clerical documentation responsibilities in addition to the clinical documentation. The frequent changes to systems and user interfaces increase the disruption of work and the learning curve associated with each change. In addition, some paper documentation still exists despite organizations utilizing EHRs. For example, complex patient orders like Total Parenteral Nutrition (TPN) and Chemotherapy continue to be provided on paper because of the complexity and uniqueness of each order based on a specific patient’s needs.
Another challenge with EHRs is the cost of maintenance. Once EHRs have been implemented, organizations need technical and personnel support to extract, manage, and analyze the data for quality improvement purposes (Upadhyay & Opoky-Agyeman, 2023), which can be costly.
Documentation Burden
Nursing documentation is similar from patient to patient with little variability. Because of this, EHRs can make nurses work more efficiently. However, the demands of documentation for regulatory and quality reporting have placed additional requirements on nurses and increased documentation time (Carter-Templeton et al., 2025). As EHRs have evolved, there are concerns regarding the burden of documentation for healthcare workers and the contribution of documentation to burnout. As a result, there is a push to decrease documentation burden on healthcare providers, with an initiative being launched to decrease documentation burden by 25% (American Medical Informatics Association, 2023).
Prioritizing the Computer
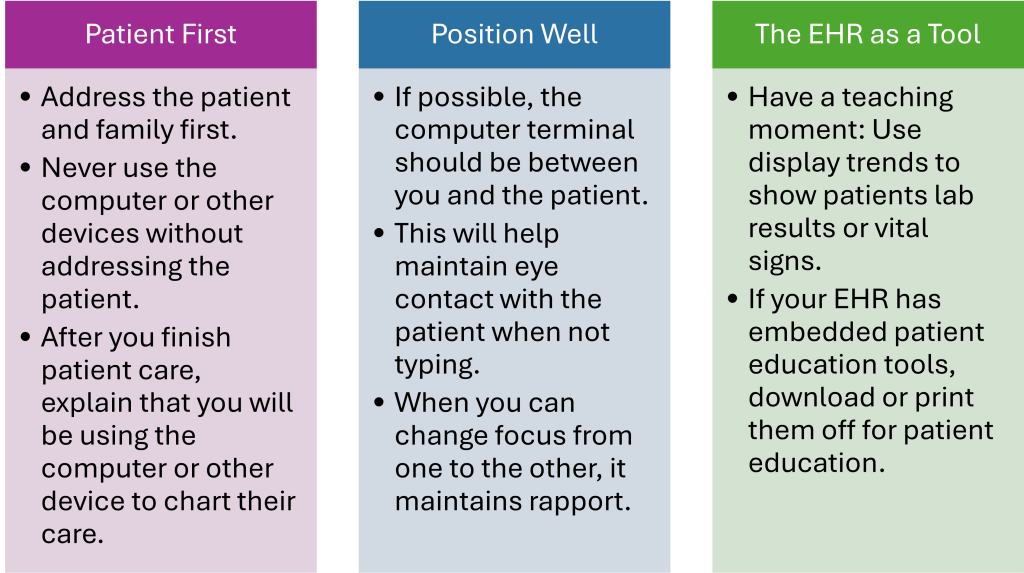
Technology can save time and resources, though it can cause patients to feel like a number (Thorne et al., 2005). The loss of human connection, social cues, and rich conversations negatively impacts care by inadvertently fragmenting care and disconnecting the patient from the healthcare team. How often do patients receive full eye contact during an assessment? You can use tips from Graphic 6.3 to mitigate the impact of technology on nurse-patient interactions.
Graphic 6.3 – Don’t Let the Computer be an Intruder: Practical Tips
Gaps in Data
Nurses are the primary users of EHRs, responsible for documenting much of the patient information, vital signs, assessments, and interventions. The role of nurses in correctly inputting data within the EHR cannot be understated. Access and accuracy of information in the EHR depend upon provider inputs. For data to be meaningful, it must be accurate, complete, reliable, relevant, and timely. It is vital for nurses and all healthcare providers to prioritize accurate and appropriate data collection and realize the potential impact of the data they enter on a patient’s chart, not only on the patient’s immediate needs but on ongoing patient care.
A good example of the impact of nurses on data input relates to structured and unstructured data within the EHR.
-
- Structured data is documented in a specific location and coded to a standard terminology. Examples of structured data include vital signs, medications, and drop-down box responses. When there is a delay in charting or structured data fields are not utilized, it can lead to gaps in patient information within the EHR, which can alter the analysis of the data and information, and lead to erroneous conclusions.
- Unstructured data is commonly seen in free-text patient notes. These open text areas are for documentation of information that does not fit anywhere else, but usability by the EHR is limited (Hughes et al., 2022). EHRs can store and share the information, but cannot analyze and extract data due to the lack of structure and variability in providers’ terminology. As a result, any free-text patient notes are not included in data mining, which can result in missed insights into trends, an incomplete picture of the patient, and an increased potential for errors due to the missed data.
It is imperative for nurses to realize that the decision to place charting in a structured manner, versus an unstructured manner, improves the EHR’s ability to support nursing, healthcare, and the health of the patient. Utilization of structured charting methods should be the primary means of patient charting; unstructured charting should only be used when necessary. In addition, when charting, nurses should ensure that the EHR is accurate and complete, and that documentation is accomplished in real-time; by doing so, the EHR will be a reliable and relevant source of patient information.
Interoperability
Interoperability is the ability of different Health IT systems and software applications “…to exchange health information and use the information once it is received” (Office of the National Coordinator for Health Information Technology, 2013). Another definition by the Health Information Management Systems Society (2025) defines interoperability as “…the ability of health information systems to work together within and across organizational boundaries in order to advance the effective delivery of health care for individuals and communities.” Simply, interoperability in healthcare refers to the ability of different healthcare information systems and software applications to communicate with each other, exchanging and utilizing information seamlessly. An example of interoperability is when an EHR used at one hospital provides patient information to a different EHR at a different hospital in an effective way.
Interoperability provides several advantages that can significantly enhance patient care and healthcare operations.
-
- Enhanced Patient Care: By facilitating seamless access to critical health information when and where it is needed, interoperability helps clinicians deliver safe, effective, and patient-centered care. This seamless data exchange supports informed decision-making, ultimately leading to improved patient outcomes.
- Empowering Individuals and Caregivers: Interoperability also offers new ways for individuals and caregivers to engage with electronic health information. Through tools like patient portals, patients can take an active role in managing and coordinating their care, accessing pertinent health data that can influence their health decisions and actions.
- Integral to Healthcare Activities: Interoperability has become an essential component of various healthcare activities, ranging from promoting health equity to enhancing the response capabilities during public health emergencies. Its role in integrating diverse health data sources is pivotal, strengthening efforts to improve outcomes across the healthcare spectrum (ONC, n.d.b).
The U.S. healthcare system is characterized by the use of multiple vendors. EHRs that have been developed by different companies have not been designed to connect with each other, especially across different providers, different organizations, and different levels of care. Even when systems do connect, they generally need to use common data formats and terminology, allowing them to understand and process shared data. Unfortunately, medical/nursing terminology may vary, which can leave gaps in the information that a receiving facility receives. This gap in information can lead to compromised care (Hughes et al., 2022; Katz, 2020) and healthcare provider and patient frustration (Katz, 2020).
This lack of connectivity means that when patients visit different healthcare providers, their EHRs may not be readily accessible across systems. Consequently, this can lead to redundancy in testing and gaps in efficiently sharing patient information.
The problem is two-fold:
- Health IT systems need to have the capability of moving clinical information from one system to another, and
- Health IT systems need to speak the same language (standardized terminology), or it may leave gaps in the crossover of data.
Efforts to improve interoperability are therefore utilizing a two-prong approach: The use of Health Information Exchanges (HIEs) and making a concerted effort to standardize healthcare terminology and language.
Health Information Exchange (HIE)
Health Information Exchange (HIEs) provide a solution to interoperability, but it is a work in progress (Katz, 2020). “Health Information Exchange, or HIE, provides the capability to electronically move clinical information among disparate healthcare information systems and maintain the meaning of the information being exchanged. The goal of health information exchange is to facilitate access to and retrieval of clinical data to provide safe, timely, efficient, effective, and equitable patient-centered care” (Health Information Management Systems Society, 2025).

According to the Office of the National Coordinator for Health Information Technology (2017, 2020), HIEs allow healthcare professionals and patients a means to access and share secure medical information electronically, improving the speed, quality, safety, and cost of patient care. HIE benefits include:
-
-
- HIEs can improve patient safety by ensuring that all providers are involved in a patient’s care and have access to the full medical history; their primary care physician, specialists, and visits to the emergency department and outpatient radiology center.
- HIEs make the patient’s health record more complete, so relevant data and information from the ED visit can be accessed by the primary care physician, and the specialist does not have to repeat laboratory tests, because he has access to the primary physician’s examination and laboratory information.
- HIEs also encourage efficient care by enabling digital follow-up instructions to be emailed to patients and prescriptions to be sent directly to pharmacies.
- HIEs reduce the amount of time patients spend filling out paperwork and briefing their providers on their medical history, allowing more time for discussions about health concerns and treatments, which has the potential to improve decision-making, reduce costs, improve health outcomes, and improve the care the patients receive.
- Sharing of patient information also allows providers to avoid readmissions, medication and medical errors, improve diagnoses, and provide safer, more effective care tailored to patients’ unique medical needs.
-
There are a variety of HIEs at the national, regional, and state levels. Progress is being made, but there are significant challenges and barriers, especially because the issues are so complex (Hughes et al., 2022).
Examples of HIEs:
Standard Terminology
An additional barrier that contributes to gaps in the exchange of medical information, when using HIEs, is a lack of standardized language.
Computer systems must share a common language for providers and healthcare organizations to fully use the data that is produced. When different EHR systems use the same definitions and structures, it facilitates interoperability (Hughes et al., 2022). When the common language/terms are different, “mutual understanding” is not possible, which leads to gaps in information.
A real-world example of different terminology that can be used by different EHR systems is in regards to lung sounds. One EHR can use the term “rattles,” while another EHR uses “rales,” and yet another uses “crackles.”
Efforts to standardize terms by non-profit groups and governmental agencies have been ongoing for many years, but currently, there is no agreed-upon standardized terminology, including nursing documentation terminology (Carter-Templeton et al., 2025).
Clinical Decision Support Systems (CDSS)
In 2009, the HITECH Act mandated the use of technology to increase patient safety and reduce costs. Clinical Decision Support Systems (CDSS) is one of the methods used to meet this legislation. CDSS encompasses a range of tools and technologies that leverage electronic health data to guide clinical decision-making.
Integrated within electronic health records (EHRs), CDSS tools provide timely, evidence-based prompts, alerts, and recommendations to healthcare providers, clinical teams, patients, and administrators. These tools are designed to support best practices and improve patient outcomes by enhancing the decision-making process at the point of care (Sutton et al., 2020; McBride & Tietze, 2023).
CDSS tools enhance safety by identifying potential medication errors, dosage issues, contraindications, and allergies. They also alert providers to critical conditions, such as low blood glucose levels or abnormal Modified Early Warning Scores (MEWS), that require immediate attention (Sutton et al., 2020). In addition to safety, CDSS improves efficiency by simplifying access to health data and presenting it in actionable formats like graphs, tables, or trend analyses. However, if these tools are poorly designed or not aligned with clinical workflows, they can lead to usability issues, workflow disruptions, and alert fatigue—reducing their overall effectiveness (Sutton et al., 2020).
Common types of CDSS tools include:
-
-
Computerized alerts and reminders (health reminders, drug-to-drug and drug allergy checks)
-
Condition-specific order sets
-
Embedded clinical guidelines (McBride & Tietze, 2023)
-
Focused patient-data reports and summaries
-
Documentation templates
-
Diagnostic support
-
Contextually relevant reference information
-
Modern CDSS systems increasingly incorporate artificial intelligence (AI) and machine learning (ML) to strengthen their capabilities. These technologies use patient-specific data for advanced analytics, enabling predictive modeling that can forecast potential medical events before they occur. By analyzing trends and patterns within EHR data, AI-driven CDS tools can assist in both individual patient care and broader organizational decision-making (Centers for Disease Control and Prevention, 2022).
Challenges with CDSS: Alert Fatigue
 Alerts are a critical part of EHRs because they can prompt healthcare providers with important and timely information that may need to be addressed. However, these alerts must be accurate and useful; when they are not, providers will override them. Wang et al. (2022) found that 92% of all alerts were dismissed, 73% of alerts were dismissed in 3 seconds or less, and 13.2% of alerts were dismissed in under 1 second. “Habitual dismissal” can lead to missing important alerts, thereby negatively impacting patient safety. A balance between increased safety due to alerts and healthcare provider alert fatigue is an important element in CDSS (Holmgren et al., 2023).
Alerts are a critical part of EHRs because they can prompt healthcare providers with important and timely information that may need to be addressed. However, these alerts must be accurate and useful; when they are not, providers will override them. Wang et al. (2022) found that 92% of all alerts were dismissed, 73% of alerts were dismissed in 3 seconds or less, and 13.2% of alerts were dismissed in under 1 second. “Habitual dismissal” can lead to missing important alerts, thereby negatively impacting patient safety. A balance between increased safety due to alerts and healthcare provider alert fatigue is an important element in CDSS (Holmgren et al., 2023).
The pop-up alert must be targeted and provide valuable information to the healthcare provider. If the alerts are frivolous and the provider is overwhelmed by the number of interruptions, they can make errors by becoming complacent and overriding all alerts. An alert that may lead to alert fatigue is aspirin, which is a common prophylactic medication used for stroke and heart attack, but will often cause an alert flag with many different types of drugs. Choosing to have an alert/flag for aspirin may be counterproductive.
Nurses: Bridging the Gap
Usability is the extent to which a product can be used by specified users to achieve specified goals with effectiveness, efficiency, and satisfaction in a specified context of use (National Institute of Standards and Technology, 2017). Health technology must be intuitive and adapted to the users. It must be easy, safe, useful, and motivating for users to use the technology, or the user will develop workarounds or not use it as it was intended. Nurses are essential to the successful adoption, implementation, and continuous improvement of healthcare technology. As end-users, nurses have unique insights into real-world functionality, usability, and workflow needs (McGonigle & Mastrian, 2025).
Nurses should:
-
- Get involved in EHR initiatives to ensure they meet the needs of both patients and clinicians. Nurses provide essential insights into usability and workflow, which help create EHRs that are intuitive, safe, and efficient.
- Be accountable for your documentation, tell the story of your care through data entry.
- If you have problems or a great idea on how to improve the EHR, bring it up with your manager or nurse informatic specialist. Understand what is possible and commit to being a part of the solution.
- Becoming super-users and participating in workflow assessments, training, and optimization initiatives.
It will be nurses’ relationship with and mindset about EHR systems that will play the greatest role in improving the nursing EHR experience. This is a journey, not a destination. As long as EHRs are here, work will continue to evolve to maximize usability and complement nursing practice. Nurses must learn to embrace technology as the newest valued member of the care team. Technology is no longer a tool at the bedside; it is a working member of the organization. And like any team member, it needs to be correctly incorporated, communicated with, and updated for optimal contribution (Iuppa, 2022).
Ultimately, empowering nurses to go beyond the role of end-users and take leadership roles in healthcare technology promotes innovation, improves patient outcomes, and ensures that technology solutions are both effective and practical.
Conclusion
EHRs are much more than digital filing systems; they are dynamic platforms that support clinical decision-making, improve care coordination, and promote patient safety. However, the success of these systems depends not only on the technology itself but also on how well it is integrated into clinical practice. Challenges such as documentation burden, gaps in data, lack of interoperability, and inconsistent terminology must be actively addressed. Nurses, who are often the primary users of EHR systems, play a critical role in shaping their effectiveness. By participating in EHR design, optimization, and education efforts, nurses can help ensure that health IT solutions truly enhance, rather than hinder, patient care. Embracing technology as a collaborative member of the healthcare team empowers nurses to lead improvements that will define the future of care delivery.
References:
- Alexander, S., Frith, K. H., & Hoy, H. (2019). Applied clinical informatics for nurses. Jones & Bartlett Learning.
- Carter-Templeton, H., Alexander, S., & Frith, K. (2025). Applied clinical informatics for nurses (3rd ed.). Jones & Bartlett Learning.
- Centers for Disease Control and Prevention. (2022). Electronic clinical decision support tools: Safer patient care for opioid prescribing. https://www.cdc.gov/opioids/healthcare-admins/ehr/index.html
- Green, J. (January, 2023). What are the core functions of EHR? EHR in Practice. https://www.ehrinpractice.com/ehr-core-functions.html
- Health Information Management Systems Society. (2025). Interoperability in healthcare. https://legacy.himss.org/resources/interoperability-healthcare
- Holmgren, A. J., McBride, S., Gale, B., Mossburg, S. (2023, March 29). Technology as a tool for improving patient safety. Patient Safety Network. https://psnet.ahrq.gov/perspective/technology-tool-improving-patient-safety
- Hughes, R., Hooper, V., Kennedy, R., Cummins, M. R., Lake, E. T., & Carrington, J. M. (2022, April 18). Interoperability explained. American Nurses Association: My American Nurse. https://www.myamericannurse.com/interoperability-explained-ehr/
- Iuppa, N. (2022, November 21). Improving the electronic health record experience for nurses. Cleveland Clinic. https://consultqd.clevelandclinic.org/improving-the-electronic-health-record-experience-for-nurses
- Katz, B. (2020). Connecting care for patients: Interdisciplinary care transitions and collaboration. Jones & Bartlett Learning.
- Leventhal, R. (2021, June 9). The top EHR vendors by hospital market share. Healthcare Innovation. https://www.hcinnovationgroup.com/finance-revenue-cycle/health-it-market/news/21226099/the-top-ehr-vendors-by-hospital-market-share-klas
- McBride, S., & Tietze, M. (2023). Nursing informatics for the advanced practice nurse: Patient safety, quality, outcomes, and interprofessionalism. Springer Publishing.
- McGonigle, D., & Mastrian, K. G. (2025). Nursing informatics and the foundation of knowledge (6th ed.). Jones & Bartlett Learning.
- National Institute of Standards and Technology. (2017). Glossary: Usability. https://csrc.nist.gov/glossary/term/usability
- Office of the National Coordinator for Health Information Technology. (n.d.a). Impact of EHRs on Care. HealthIT.gov. Retrieved April 15, 2024, from https://www.healthit.gov/topic/health-it-and-health-information-exchange-basics/benefits-ehrs
- Office of the National Coordinator for Health Information Technology. (n.d.b). Interoperability. HealthIT.gov. Retrieved April 15, 2024, from https://www.healthit.gov/topic/interoperability
- Office of the National Coordinator for Health Information Technology. (n.d.c). What are the advantages of electronic health records? HealthIT.gov. Retrieved April 15, 2024, from https://www.healthit.gov/faq/what-are-advantages-electronic-health-records
- Office of the National Coordinator for Health Information Technology. (2013). The path to interoperability. U.S. Department of Health and Human Services. https://www.healthit.gov/sites/default/files/factsheets/onc_interoperabilityfactsheet.pdf
- Office of the National Coordinator for Health Information Technology. (2017). HIE benefits. U.S. Department of Health and Human Services. https://www.healthit.gov/topic/health-it-and-health-information-exchange-basics/hie-benefits
- Office of the National Coordinator for Health Information Technology. (2020). What is HIE? U.S. Department of Health and Human Services. https://www.healthit.gov/topic/health-it-and-health-information-exchange-basics/what-hie
- Office of the National Coordinator for Health Information Technology. (2021). National trends in hospital and physician adoption of electronic health records. https://www.healthit.gov/data/quickstats/national-trends-hospital-and-physician-adoption-electronic-health-records
- Sutton, R. T., Pincock, D., Baumgart, D. C., Sadowski, D. C., Fedorak, R. N., & Kroeker, K. I. (2020). An overview of clinical decision support systems: Benefits, risks, and strategies for success. NPJ Digital Medicine 3(17). https://doi.org/10.1038/s41746-020-0221-y
- Thorne, S., Kuo, M., Armstrong, E-A., McPherson, G., Harris, S.R., & Hislop, T.G. (2005). “Being Known”: Patients’ perspectives of the dynamics of human connection in cancer care. Psycho-Oncology, 14, 887–898. http://doi.org/10.1002/pon.945
- Upadhyay, S. & Opoku-Agyeman, W. (2023). Implementation levels of electronic health records and their influence on quality and safety. Online Journal of Nursing Informatics (OJNI), 26(3), https://www.himss.org/resources/online-journal-nursing-informatics
- Wang, L., Goh, K. H., Yeow, A., Poh, H., Li, K., Yeow, J. J. L., Tan, G., Soh, C. (2022, February 16). Habit and automaticity in modical alert override: Cohort study. Journal of Medical Internet Research 24(2):e23355. https://doi.org/10.2196/23355.
OER Resources Utilized in this Section:
- Bowen, C., Carey, B., Palozie, J., & Reinholdt, M. M. (2024, October 16). Medical-surgical nursing. https://openstax.org/details/books/medical-surgical-nursing. Licensed under a Creative Commons Attribution 4.0 International (CC BY) license,
- Gurung, S. (2024). Managerial information systems in healthcare. PressBooks. https://pressbooks.cuny.edu/profgurung. Licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
- Murphy, J. (2022). Transitions to professional nursing practice. https://courses.lumenlearning.com/suny-delhi-professionalnursing/ Licensed under Creative Commons Attribution 4.0 International License
- Ochs, J., Roper, S. L., & Schwartz, S. M. (2024, May 15). Population health for nurses. https://openstax.org/details/books/population-health Licensed under a Creative Commons Attribution 4.0 International (CC BY) license.
- Valaitis, K. (2023). Exploring the U.S. healthcare system. University of West Florida. Pressbooks. https://pressbooks.uwf.edu/ushealthcaresystem/ Licensed under a Creative Commons Attribution 4.0 International License
Health IT is a term that is used for the electronic health systems that healthcare professionals and patients use to store, share, and analyze health information.
The ability of different Health IT systems and software applications to exchange health information and use the information once it is received.
Provides the capability to electronically move clinical information among disparate healthcare information systems and maintain the meaning of the information being exchanged.
A technology tool that provides healthcare providers with knowledge and person-specific information to enhance decision-making.
Artificial intelligence (AI) is the intelligence of machines or software, as opposed to the intelligence of human beings or animals.
"Machine learning is a branch of artificial intelligence (AI) and computer science which focuses on the use of data and algorithms to imitate the way that humans learn, gradually improving its accuracy" (IBM, n.d.)
IBM. (n.d.). What is machine learning? Retrieved: October 31, 2023. https://www.ibm.com/topics/machine-learning

