2 Health IT and Healthcare Technology
Laura K. Garner-Jones
Chapter 2 Overview
- Overview of Health IT
- Positive impact of Health IT
- Current healthcare technologies
- Patient Data Management Systems (PDMS)
- Challenges with healthcare technology
Introduction
The 21st Century is known as the age of information technology. Healthcare has seen significant progress with technology and innovation over the past 25 years, especially since the Internet has permeated almost every aspect of our personal and work lives. As a result, technology has changed the way we interact with each other and how information is exchanged. In recent years, information technology has been at the forefront of revolutionizing numerous industries, and health care is no exception. The integration of technology into healthcare systems has led to significant advancements, positively impacting patient care and outcomes.
Health Information Technology (Health IT)
Health IT is transforming both direct and indirect patient care. Technologies intended to improve safety, efficiency, and quality are also transforming how we deliver care and the resulting patient outcomes. The way care was delivered ten years ago is quite different than today, and the care we deliver today will look very different in ten years. Examples of Health IT (Office of the National Coordinator for Health Information Technology, n.d.) include:
-
- Electronic Health Records (EHRs)
- Patient portals and Personal Health Records (PHRs)
- Electronic prescribing
More detailed information on EHRs, PHRs, and patient portals will be covered in later chapters, but it is important to realize the impact that Health IT has had on healthcare, healthcare providers, and patients.
Positive Impact of Health IT
Health IT has revolutionized health care, and will continue to do so in the future. Health IT provides support for nurses and other healthcare providers in improving the delivery and outcomes of patient care (Carter-Templeton et al., 2025). Key areas of positive influence include:
Communication & Collaboration: Paper-based health records, which most doctors and hospitals previously used, could only be accessed by one person at a time and at one particular location. Electronic records can be used simultaneously by multiple providers and multiple locations, which is conducive to better communication, collaboration, and coordination of care (Office of the National Coordinator of Health Information Technology, 2013). Health IT has led to enhanced communication among the patient, providers, and the care team. Examples of communication using Health IT include reviewing another provider’s patient notes, making referrals, and conveying critical information to other clinicians (Carter-Templeton et al., 2025). Enhancing communication has resulted in benefits such as informed decision-making, stronger relationships, and decreased delays in care. In addition, patient portals allow patients to contact their providers directly, engaging and empowering them to be directly involved in their health.
Safety: Health IT has led to enhanced patient safety by reducing medication errors, reducing adverse drug reactions, improving compliance with practice guidelines, and enhancing care coordination. Years ago, physicians would write all their orders, which at times were difficult to interpret. Now, computerized provider order entry (CPOE) allows providers to enter medical orders directly into the EHR. Not only has this practice reduced human error in transcribing orders, but it has also been instrumental in catching possible medication order errors, such as prescribing a medication that the patient may be allergic to or a medication that is contraindicated. In addition, barcode medication administration has helped to ensure the right medication for the right patient.
Quality: With the assistance of the EHR, an improvement in quality of care can be realized (Carr et al., 2023). Structured data and information from the EHR can be used to inform practice, like identifying patients who need immunizations or screening tests. Similarly, data and information can be utilized for determining how organizations are meeting quality standards, such as infection rates and falls. Using the data as a baseline measurement, quality improvement initiatives can be instituted, and the data reviewed over time to see if the initiative was effective.
Patient outcomes: Real-time data monitoring and Clinical Decision Support Systems (CDSS) That include things like notifications, alerts, reminders, clinical guidelines, condition-specific order sets, clinical summaries, documentation templates, and diagnostic supports, help healthcare providers with the necessary information to make informed decisions to support patient care. An example of this you may see as a nurse is the notification of a potential early detection of deterioration based on trending vital signs or medical data.
Data utilization: Big data analytics (BDA), the process of analyzing large and complex datasets to uncover patterns, correlations, trends, and other useful information, holds tremendous potential for healthcare and research (Thacharodi et al., 2024). Large amounts of complex medical data are being collected in EHRs (e.g., lab values from tests, diagnostic imaging, sensor devices, and genomics) and other large databases or datasets. The sheer volume of medical and health-related data is increasing exponentially, which allows for the collection, analysis, and interpretation of vast amounts of patient data, enhancing overall clinical decision-making and enabling healthcare providers to deliver more accurate and effective care. Analysis can also identify historical patterns or predict future events, detect trends more quickly, lower research and analysis costs, and has the potential to improve patient outcomes by providing actionable knowledge and identifying data-driven strategies that enhance patient care and safety (Thacharodi et al., 2024).
Operational efficiency: Automation of administrative tasks, such as appointment scheduling, billing, and inventory management, has streamlined operations, reduced errors, and increased efficiency in healthcare facilities.
Workflow: Workflow is defined as a sequence of steps to perform an activity in the clinical environment (Lindsay & Lytle, 2022). Health IT has improved the workload of nurses and other care providers (Arcega et al., 2020). For example, the process of centralizing patient records into EHRs has eliminated time spent searching through paper charts, helped to clarify and streamline the documentation of care, and enabled the setting of electronic reminders for tasks that need to be completed. Such time-saving measures create more time for nurses and providers to spend with patients. In addition, messaging systems allow nurses to quickly send medical updates and questions to the provider without causing interruptions to their workflow.
Patient engagement: Patient portals empower patients to take an active role in managing their health. These tools provide access to medical records, facilitate appointment bookings, and offer educational resources to support informed decision-making.
Security and Privacy: Health IT has improved the security and privacy of patient information through the implementation of robust encryption protocols, access controls, and compliance with regulatory standards.
Healthcare Technology of Today
Healthcare Technology is a broad term referring to any technology (including Health IT) used to improve healthcare delivery, patient care, and research. Technology has improved the accuracy, speed, and accessibility of diagnostics and has the potential to decrease the severity of chronic illnesses due to earlier detection and intervention. Telehealth platforms, for example, leverage technology to remotely monitor and manage chronic conditions. Patients can use wearable devices to track vital signs, and health-care providers can access real-time data to make timely adjustments to treatment plans; these practices enhance accessibility to care, reduce the need for frequent in-person visits, and help manage chronic illnesses more effectively.
Ultimately, healthcare technologies enhance the quality of healthcare, improve patient outcomes and patient safety, and enable healthcare professionals to deliver medical treatments smarter and faster (Alotaibi & Federico, 2017). As healthcare services continue to evolve with the integration of cutting-edge tools and technologies, patients can also benefit from expanded access to care and experience treatment that is increasingly tailored to their individual health needs and preferences, thereby improving their quality of life (Thacharodi et al., 2024).
Telehealth
There are several ways to define telehealth. Alexander et al. (2019) define telehealth as the process of using technology to assess and manage patients. Mayo Clinic (2024) defines telehealth as the use of digital information and communication technologies to manage your health and access remote health care services. Additionally, Medicaid.gov (n.d.) defines telehealth as “…the use of telecommunication and information technology to provide access to health assessment, diagnosis, intervention, consultation, supervision, and information across distance.” Telehealth services have been shown to provide quality, cost-effective care that benefits patients, reduces hospitalizations, and readmissions (Alder, 2024).
Although telehealth may seem to be an entirely new technology, it really is not. Years ago, NASA pioneered telemetry and telemedical technologies in the space program to monitor the life signs of astronauts. Telehealth technology provides an opportunity for virtual healthcare visits and remote monitoring to support rural populations that are often medically underserved or those who need isolation. For example, the only way that many patients were provided a continuity of care when in-person visits were restricted during the COVID-19 pandemic was through virtual visits using telehealth platforms (Bird, 2021).
In addition to improved access, it is estimated that telehealth could save the U.S. healthcare system over $4 billion annually due to the reduction in referrals, streamlined medical evaluations, and better chronic disease management. Currently, chronic disease healthcare costs account for 75% of medical expenses. There is speculation that the financial burden of hospital readmissions for patients with chronic diseases can be curbed by monitoring patients at home, using technology to ensure medication adherence, and providing patients with easier access to providers (Mechanic et al., 2022).
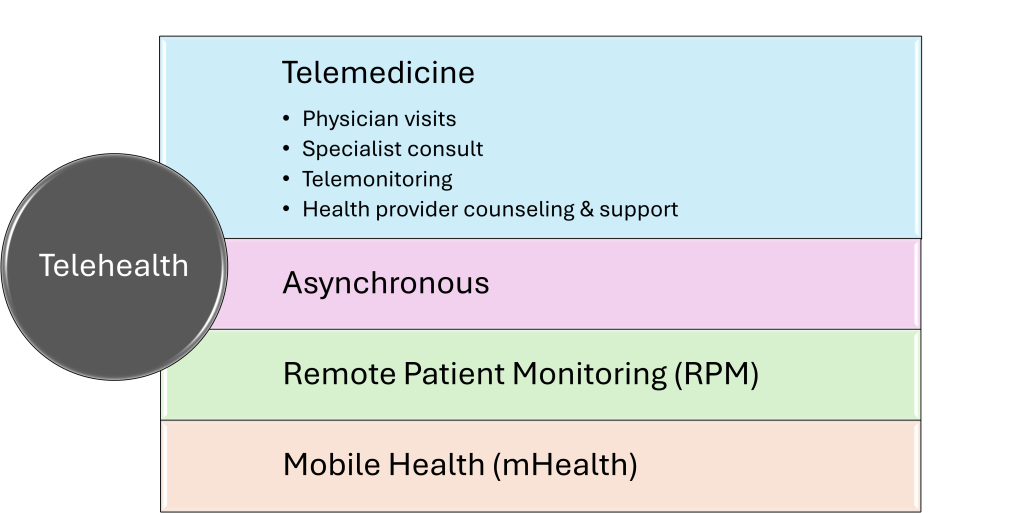
Telehealth Categories and Subcategories (See Graphic 2.1 & Graphic 2.2)
- Telemedicine: The delivery of synchronous healthcare services between the patient and the healthcare provider remotely (American Hospital Association, 2025).
- Physician visits
- Specialist consultation: Telestroke, teleED, teleICU
- Telemonitoring: Virtual nursing, telesitting
- Health provider counseling & support: Mental health counseling, dietary coaching, speech, PT, OT, cardiac rehab, respiratory assessment/ventilator management
- Asynchronous: Also known as “store-and-forward.” Providers review information asynchronously to diagnose or treat an issue (Telehealth.HHS.gov, 2024).
- Remote Patient Monitoring: “…the transmission of an individual’s personal health and medical data to the healthcare provider in a different location for diagnosis and treatment (Carter-Templeton et al., 2025).
- Mobile Health (mHealth) applications: Transmission of health information and services via mobile technology (Carter-Templeton et al., 2025).
Graphic 2.1 – Four Categories of Telehealth
Telemedicine
Telemedicine is the first subcategory of telehealth and is a health service that is provided through audio and/or video technology. Telemedicine enables healthcare providers to offer office visits, specialty consultations, and patient monitoring without being present physically and, as a result, can lower healthcare costs and improve provider/patient satisfaction (Thacharodi et al., 2024). In addition, telemedicine can improve healthcare access and patient outcomes, especially in rural or remote areas. There are four subcategories of telemedicine: Physician visits, specialist consultation, telemonitoring, and health provider counseling and support (See Graphic 2.2).
Graphic 2.2 – Four Subcategories of Telemedicine
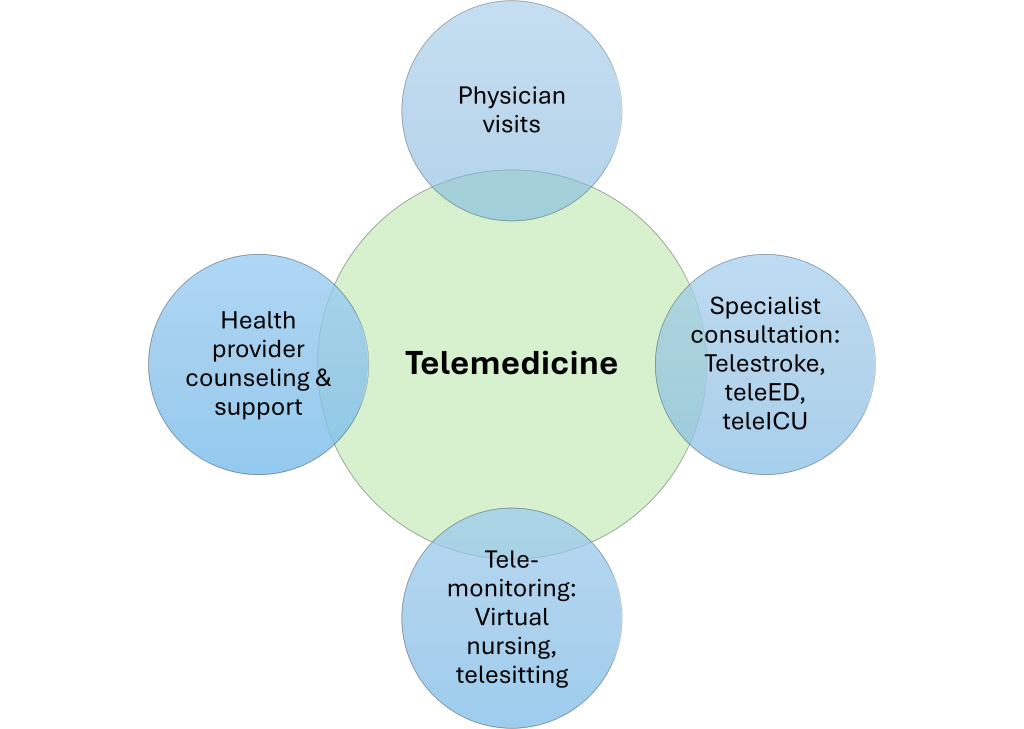
Physician Visits
Utilizing telemedicine, through the use of electronic communications and software, allows patients to see their provider without the need for an in-person visit. Telemedicine physician visits can make healthcare more accessible and affordable. Patients can conveniently access care from their current location, eliminating the need to travel, take time off work, or arrange childcare, thereby reducing associated costs.
Telemedicine can significantly reduce health disparities in rural areas with limited physician access. Approximately 20% of the U.S. population resides in rural areas, yet only 9% of physicians serve these areas (Mechanic et al., 2022). Telemedicine is extremely popular with patients, improving patient satisfaction scores for providers (Alder, 2024) and decreasing exposure to contagious diseases such as influenza or COVID-19. Ultimately, telemedicine is extremely effective at reaching patients where they are, encouraging collaborative visits, and decreasing risk. These conclusions are supported by the research that indicates that patients who participate in telemedicine visits experience lower hospitalization rates (Campion et al., 2023; Pande et al., 2015; Peters et al., 2021) and show a reduction in “convenience” emergency department visits (Alder, 2024).
Watch this short video to see how telemedicine is being utilized in caring for those experiencing homelessness.
Specialist Consultation
Additionally, telemedicine provides enhanced access to specialized providers, regardless of geographical constraints, while also minimizing wait times for appointments, lowering exposure to potential health risks, and increasing patient engagement and adherence to treatment (Vicente et al., 2022).
Telehealth involving specialist consultation is an important and evolving aspect of healthcare. Approximately 50% of acute care hospitals in the U.S. engage in this type of telemedicine. Remote stroke care, or “TeleStroke”, is commonly used in emergency departments without in-house neurology stroke experts. Endorsed by the American Heart Association, it has improved millions of patients’ access to emergent stroke care. In some cases, a nurse may use peripheral medical equipment (e.g., digital stethoscopes, otoscopes, ultrasounds) physically with the patient, while the consulting medical provider conducts a remote evaluation. Other examples of specialist consultation include TeleTrauma, TeleBurns, TeleDermatology, and TeleICU, just to name a few (Jen et al., 2023).
Telemonitoring
The practice of monitoring aspects of a patient’s health from a remote location is called telemonitoring. Telemonitoring has proven to be effective at monitoring both acute and chronic conditions. Research has shown telemonitoring to be particularly useful in improving patient outcomes for heart failure, stroke, COPD, asthma, and hypertension (Noah et al., 2018). By closely monitoring the patient’s data, providers can identify changes in a patient’s condition more quickly and alter the plan of care accordingly.
Virtual nursing is a growing form of telemonitoring that goes beyond collecting patient data by incorporating direct patient contact. Using video conferencing technology, it allows for real-time nursing evaluation, interaction, redirection, and education. Virtual nursing can include a single nurse and patient interaction, like in teletriage or nursing visits for the purpose of coaching or education. More commonly, however, virtual nursing includes nurses or nursing support personnel in a team approach. This hybrid approach places the virtual nurse or nursing staff as a means of support for the bedside nursing team or to provide telesitting (see telehealth example below).
Telemonitoring: Virtual Nursing Example
Providence, a healthcare organization in Texas, was experiencing workforce shortages, high turnover, an aging population, and decreased nurse satisfaction. In an effort to mitigate these issues, they implemented a virtual healthcare model that partners a virtual nurse with a bedside nurse and nursing assistant. Called “co-caring,” this model utilizes virtual nurses in handling admissions, education, and discharges. In evaluating the virtual nursing results, the new graduate nurse turnover rate dropped by 73% and 55% for all staff. Other benefits were a reduced need for travel nurses, shorter patient stays, and higher nurse satisfaction. Providence is expanding the program due to its multi-faceted success (Singer, 2024).
Gain insight into the role of a virtual nurse through this brief day-in-the-life video
Health Provider Counseling & Support
Patient visits provided by healthcare providers other than physicians are becoming increasingly more common. Dietary coaching, cardiac rehab, triage, and respiratory follow-up evaluations have been conducted virtually. Other examples include:
-
-
- Virtual counseling: Mental health counseling in the comfort of the patient’s home.
- Telerehabilitation: A form of telemedicine where occupational therapists, physical therapists, or speech therapists can assess the patient’s home rehab progress.
- Telehospice: Real-time psychological support for patients and caregivers (McGonigle & Mastrian, 2025).
-
Asynchronous
The asynchronous telehealth includes “store and forward” technology, or the storage of medical information such as test results, lab reports, imaging, and medical documentation. Healthcare providers can gather the data, upload it, share it, and leave the data for review by other providers using secure messaging (Alder, 2024). In addition, secure messaging can allow healthcare providers to send photos or text messages to other healthcare providers, or from patients to healthcare providers. An example of asynchronous telehealth is the sharing of digital images between healthcare providers, medical specialists, and radiologists. Collaboration and treatment plans can be easily accomplished, no matter where the providers are located (Alder, 2024).
Remote Patient Monitoring (RPM)
Remote Patient Monitoring (RPM) allows the direct transmission of a patient’s clinical measurements to their healthcare provider from a distance, utilizing monitoring tools including electrocardiography devices, heart rate monitors, maternity care monitoring, pediatric monitoring, pulse oximeters, and smart scales (Welkin Health, 2020). RPM allows the monitoring of patients outside the traditional settings, like in the home (Carter-Templeton et al., 2025). In addition, RPM allows for data collection and sharing with providers to help inform diagnosis and interventions. The benefits extend to patients as well. RPM enables patients to take a more proactive approach to their health and take greater control over health outcomes while also sharing important data with their providers (Kavukat, 2024). RPM is especially effective in chronic disease management, like patients with diabetes. Data from connected glucose monitors and insulin delivery systems provide glucose control information directly to providers, who can intervene sooner if needed.
Mobile Health (mHealth)
Mobile Health (mHealth) is defined as “the use of mobile and wireless technologies to promote health” (HealthIT.gov, 2019). mHealth falls under the telehealth umbrella, and can include technology used by patients alone, and technology used by patients and healthcare providers in collaboration. mHealth can enhance diagnosis, help prevent diseases, improve treatments, and increase accessibility (Carter-Templeton et al., 2025).
Smartwatch and fitness tracker applications, for instance, use biosensors to monitor heart rate, respiration rate, oxygen saturation, activity, sleep patterns, and ECG readings. In addition, these applications/devices can be used to monitor fitness and wellness as well as store patient health information, and provide patient reminders (Smuck et al., 2021). mHealth will be discussed in detail in Chapter 5.
Patient Data Management Systems (PDMS)
Patient Data Management Systems (PDMS) is a comprehensive software solution designed to manage and organize patient-related data within healthcare facilities. PDMS automatically retrieves data from bedside medical equipment, such as vital sign machines, ventilators, and intravenous (IV) pumps. The integration of PDMS and telemonitoring creates a more comprehensive and seamless health-care management approach. Patient data collected through telemonitoring devices can be directly fed into the PDMS, providing healthcare providers with a holistic view of the patient’s health status. This integration promotes data-driven decision-making, enhances care coordination, and supports more personalized and proactive healthcare interventions. Benefits of PDMSs include their integration with clinical decision support systems that enhance clinical decision-making, a decrease in charting time, an increase in time to spend with the provider, a reduction in medical errors, and improved clinical outcomes. Some examples of PDMSs are Smart Beds and Smart Pumps.
Smart Beds
A smart medical bed is a highly innovative hospital bed with additional technical features that support best practice for patient care. Available features depend on the type of bed purchased; however, most smart beds include fall prevention features like bed alarms, motion-activated night-lights, reminders for healthcare providers if wheels are not locked or the bed alarm is not set, and verbal commands, available in multiple languages, that will tell the patient not to get up until help arrives. Other features include pressure-redistribution functions that help to redistribute weight over bony prominences, turning supports, and “microclimate” surface technology that reduces body heat and absorbs excess moisture, which can reduce the prevalence of pressure ulcers and skin breakdown.
Data captured from smart beds can be used to improve patient care. For example, data on which settings were activated, how long the bed alarm had been sounding, and when the patient had moved prior to the fall are available for review. The data may also be used to prevent falls: for example, by analyzing the patient’s movements to determine which bed alarm setting would be most appropriate. By utilizing special sensors, smart beds can also capture vital sign data: pulse, respiration rate, and temperature. If abnormalities are noted, the healthcare team is alerted. Smart beds can also capture patient weight; they can even be programmed to subtract the weight of the bed linens to ensure accuracy.
Smart Pumps
A smart pump is an intravenous infusion device that combines computer technology and drug libraries to limit the potential for medication errors. Embedded software provides a drug library that stores concentrations, dosing, and dose limits for each medication, automatically populating the pump settings or alerting the nurses if the dose exceeds a predetermined limit, reducing the likelihood of medication errors. Smart pumps that integrate with the EHR and barcode medication administration systems are becoming more common. Two-way communication between the smart pump and the EHR enables the pump to feed information (such as volume infused and rates of titratable drugs) back to the EHR, reducing the need for the nurse to manually input this information into the chart.
Like other technologies, smart pumps produce data that may be captured, stored, and analyzed. Drug libraries, for instance, detail the lower and upper bounds that govern each medication’s safe infusion rate. If a hard stop is overridden, data can be collected to determine the date, time, nurse, and reason selected for the override. In the event of a medication error, data can be reviewed to determine if the drug library was used to program the pump, if the correct medication was selected from the drug library, and if the pump was programmed correctly. Vital signs, such as continuous capnography of respirations and pulse-oximetry, can be collected when patient-controlled analgesia is used. These data can be automatically populated in the EHR, and the care team can be alerted to the potential for adverse reactions, such as narcotic-induced respiratory depression.
Challenges with Healthcare Technology
There can also be drawbacks to technology in healthcare. Balancing the high cost of technology with the benefits is significant for the entire healthcare system. Initial training of the nursing workforce with ongoing competency is costly, compelling leadership to find ways to contain these high costs. One of the core challenges with technology is retaining the human element in practice (Huston, 2013). In addition, technology can bring about fear of the unknown when a new treatment is touted to cure a disease beyond what is normally possible.
The Human Element

Healthcare as we know it today is heavily reliant on technology. Nursing care has quickly adjusted to the use of advanced technology within healthcare, and nursing care is now more technology-based (Arcega et al., 2020). Healthcare innovation has isolated nurses and other healthcare staff from interacting with patients in a number of ways, such as with self-registration check-in stations. As much as technology can save time and be more cost-effective, the loss of the personal touch can negatively impact healthcare.
Innovation increases the risk of losing sight of the core values that are inherent in the nursing profession (Lee et al., 2018). It can be challenging to find the time to nurture the human connection with patients, coworkers, and other support staff. Technology is a healthcare delivery tool and should not get in the way of building relationships and providing compassionate care to patients. Human touch also provides positive experiences for patients and nurses alike, making patients “feel human again” (Arcega et al., 2020).
Nurses need to find creative, personal ways outside of technology to show caring and compassion, especially in stressful work environments like healthcare settings.
Unrealistic Expectations
Medical breakthroughs, technological advances, and experimental treatments can also give patients a false sense of security that diseases can be cured (Lee et al., 2018). For example, patients may struggle to know when it is the right time to end cancer treatments. Innovative treatments can offer endless treatment options, requiring nurses to assist patients with these important decisions. Expressing care and compassion independent of technology can help foster authenticity and meaningful connections between nurses, patients, and families.
Conclusion
As healthcare continues to evolve in the digital age, technology has become an indispensable component of patient care, clinical workflows, and healthcare operations. From electronic health records to remote patient monitoring, from clinical decision support systems to smart pumps and telehealth innovations, Health Information Technology (Health IT) is transforming how care is delivered, managed, and experienced. Nurses, positioned at the forefront of patient interaction, are not only key users of these technologies but also vital contributors to their successful implementation and evolution.
Health IT and healthcare technologies’ benefits are numerous, but the integration of healthcare technology is not without its challenges. Issues such as a loss of human connection and unrealistic expectations about technology’s capabilities underscore the importance of maintaining a balance between innovation and compassion. Nurses must remain vigilant in preserving the human element of care, ensuring that empathy, presence, and individualized attention remain central to the healing process.
References
- Alder, S. (2024, May 3). Types of telehealth. The HIPAA Journal. https://www.hipaajournal.com/types-of-telehealth/
- Alexander, S., Frith, K. H., & Hoy, H. (2019). Applied clinical informatics for nurses. Jones & Bartlett Learning.
- Alotaibi, Y. K., & Federico, F. (2017). The impact of health information technology on patient safety. Saudi Medical Journal, 38(12), 1173. https://doi.org/10.15537/smj.2017.12.20631
- American Hospital Association. (2025). Fact sheet: Telehealth. https://www.aha.org/system/files/media/file/2025/02/Fact-Sheet-Telehealth-20250207_0.pdf
- Arcega, J., Autman, I., De Guzman, B., Isidienu, L., Olivar, J., O’Neal, M., & Surdilla, B. (2020). The human touch: Is modern technology decreasing the value of humanity in patient care? Critical Care Nursing Quarterly, 43(3), 294-302. https://doi.org/10.1097/CNQ.0000000000000314
- Bird, H. (2021). A now-or-never moment for telehealth? Healthcare Financial Management Association. https://www.hfma.org/topics/hfm/2021/may/now-or-never-moment-telehealth-demand-remains-strong-technology-healthcare-industry.html
- Campion, F. X., Mathur, A., & Konczewski, B. (2023, July). The impact of telehealth on hospitalization of skilled nursing facility patients during the COVID-19 pandemic. Telehealth and Medicine Today. https://doi.org/10.30953/thmt.v8.416
- Carr, L. H., Christ, L., & Ferro, D. F. (2023). The electronic health record as a quality improvement tool: Exceptional potential with special considerations. Clinics in Perinatology, 50(2), 473. https://doi.org/10.1016/j.clp.2023.01.008
- Carter-Templeton, H., Alexander, S., & Frith, K. (2025). Applied clinical informatics for nurses (3rd ed.). Jones & Bartlett Learning.
- Centers for Disease Control. (2023). Health information technology use among adults: United States, July–December 2022. National Center for Health Statistics. https://www.cdc.gov/nchs/products/databriefs/db482.htm
- Cleveland Clinic. (2022, November 21). Improving the electronic health record experience for nurses: Embracing new technology to alleviate documentation burdens. https://consultqd.clevelandclinic.org/improving-the-electronic-health-record-experience-for-nurses
- Health Information Management Systems Society. (2025). Interoperability in healthcare. https://legacy.himss.org/resources/interoperability-healthcare
- HealthIT.gov. (2019, May 31). Leverage APIs and other health IT. HealthIT – The ONC Patient Engagement Playbook. https://www.healthit.gov/playbook/pe/chapter-6/
- Hughes, R., Hooper, V., Kennedy, R., Cummins, M. R., Lake, E. T., & Carrington, J. M. (2022, April 18). Interoperability explained. American Nurses Association: My American Nurse. https://www.myamericannurse.com/interoperability-explained-ehr/
- Huston, C. (2013). The impact of emerging technology on nursing care: Warp speed ahead. The Online Journal of Issues in Nursing, 18(2). http://doi.org/10.3912/OJIN.Vol18No02Man01
- Katz, B. (2020). Connecting care for patients: Interdisciplinary care transitions and collaboration. Jones & Bartlett Learning.
- Kavukat, T. (2024, December 17). 8 emerging trends in healthcare technology for 2025. RXNT. https://www.rxnt.com/8-emerging-trends-in-healthcare-technology-for-2025/?srsltid=AfmBOoqCeSWa4tX4x2mShA_R08FprYyZhSf4kIxhnG6gc5oQq3W8ODcW
- Lee, V., Reilly, R., Laux, K., & Robitaille, A. (2018). Compassion, connection, community: Preserving traditional core values to meet future challenges in oncology nursing practice. Canadian Oncology Nursing Journal, 28(3), 212-216. http://www.canadianoncologynursingjournal.com/index.php/conj/article/view/914
- Lindsay, M. R., & Lytle, K. (2022). Implementing best practices to redesign workflow and optimize nursing documentation in the electronic health record. Applied Clinical Informatics, 13(3), 711-719. https://doi.org/10.1055/a-1868-6431
- Mayo Clinic. (2024, September 5). Telehealth: Technology meets healthcare. https://www.mayoclinic.org/healthy-lifestyle/consumer-health/in-depth/telehealth/art-20044878
- McGonigle, D., & Mastrian, K. G. (2025). Nursing informatics and the foundation of knowledge (6th ed.). Jones & Bartlett Learning.
- Mechanic, O. J., Persaud, Y., & Kimball, A. B. (2022). Telehealth systems. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459384/
- Medicaid.gov (n.d.). Telehealth. Retrieved July 12, 2025: https://www.medicaid.gov/medicaid/benefits/telehealth
- National Institute of Standards and Technology. (2017). Glossary: Usability. https://csrc.nist.gov/glossary/term/usability
- Noah, B., Keller, M. S., Mosadeghi, S., Stein, L., Johl, S., Delshad, s., Tashjian, V. c., Lew, d., Dwan, J. T., Jusufagic, A., & Spiegel, B. M. R. (2018). Impact of remote patient monitoring on clinical outcomes: An updated meta-analysis of randomized controlled trials. NPJ Digital Medicine, 1, 20172. https://doi.org/10.1038/s41746-017-0002-4
- Office of the National Coordinator for Health Information Technology. (n.d.). Health IT: Advancing America’s healthcare. Retrieved July 11, 2025: https://www.healthit.gov/sites/default/files/pdf/health-information-technology-fact-sheet.pdf
- Office of the National Coordinator for Health Information Technology. (2013). The path to interoperability. U.S. Department of Health and Human Services. https://www.healthit.gov/sites/default/files/factsheets/onc_interoperabilityfactsheet.pdf
- Office of the National Coordinator for Health Information Technology. (2017). HIE benefits. U.S. Department of Health and Human Services. https://www.healthit.gov/topic/health-it-and-health-information-exchange-basics/hie-benefits
- Office of the National Coordinator for Health Information Technology. (2020). What is HIE? U.S. Department of Health and Human Services. https://www.healthit.gov/topic/health-it-and-health-information-exchange-basics/what-hie
- Pande, R. L., Morris, M., Peters, A., Spettell, C. M., Feifer, R., & Gillis, W. (2015). Leveraging remote behavioral health interventions to improve medical outcomes and reduce costs. The American Journal of Managed Care, 21(2), e141–e151. https://pubmed.ncbi.nlm.nih.gov/26065105/
- Peters, G. M., Kooji, L., Lenferink, A., van Harten, W. H., & Doggen, C. J. M. (2021, September). The effect of telehealth on hospital services use: Systematic review and meta-analysis. Journal of Medical Internet Research, 23(9), e25195. https://doi.org/10.2196/25195
- Singer, D. (2024, March). Providence to expand co-caring model that adds virtual nurses to the team. Catholic Health Association of the United States. https://www.chausa.org/news-and-publications/publications/catholic-health-world/archives/march-2024/providence-to-expand-co-caring-model-that-adds-virtual-nurses-to-the-team
- Smuck, M., Odonkor, C. A., Wilt, J. K., Schmidt, N., & Swiernik, M. A. (2021). The emerging clinical role of wearables: Factors for successful implementation in healthcare. NPJ Digital Medicine, 4(1), 45. https://doi.org/10.1038/s41746-021-00418-3
- Thacharodi, A., Singh, P., Meenatchi, R., Tawfeeq Ahmed, Z. H., Kumar, R. R. S., V, N., Kavish, S., Maqbool, M., & Hassan, S. (2024). Revolutionizing healthcare and medicine: The impact of modern technologies for a healthier future—A comprehensive review. Health Care Science, 3(5), 329-349. https://doi.org/10.1002/hcs2.115
- University of St. Augustine for Health Sciences. (2023, December 15). What is virtual healthcare? https://www.usa.edu/blog/what-is-virtual-healthcare/
- Vicente, M. A., Fernandez, C., Guilabert, M., Carrillo, I., Martin-Delgado, J., Mira, J. J. (2022, November). Patient engagement using telemedicine in primary care during COVID-19 pandemic: A trial study. International Journal of Environmental Research and Public Health, 19(22). https://doi.org/10.3390/ijerph192214682
- Welkin Health. (2020). Remote patient monitoring devices: Your ultimate guide. https://welkinhealth.com/remote-patient-monitoring-devices/
Media Attributions:
- HRSATube. (2023, March 24). How telehealth helps providers deliver care [Video]. YouTube. https://www.youtube.com/watch?v=VHmnN7NFwHE
- Nurse Holding Elderly Patient’s Hand by Portaldelsur ES. Flickr. Licensed through Creative Commons BY-NC-SA 2.0.
- WXYZ – TV Detroit I Channel 7. (2024, February 8). Trinity Health implements virtual nurse program to address nurse shortage [Video]. YouTube. https://www.youtube.com/watch?v=5Ub2qOl22GA
OER Resources Utilized in this Section:
- Bowen, C., Carey, B., Palozie, J., & Reinholdt, M. M. (2024, October 16). Medical-surgical nursing. https://openstax.org/details/books/medical-surgical-nursing. Licensed under a Creative Commons Attribution 4.0 International (CC BY) license,
- Murphy, J. (2022). Transitions to professional nursing practice. https://courses.lumenlearning.com/suny-delhi-professionalnursing/ Licensed under Creative Commons Attribution 4.0 International License
- Ochs, J., Roper, S. L., & Schwartz, S. M. (2024, May 15). Population health for nurses. https://openstax.org/details/books/population-health Licensed under a Creative Commons Attribution 4.0 International (CC BY) license.
- Valaitis, K. (2023). Exploring the U.S. healthcare system. University of West Florida. Pressbooks. https://pressbooks.uwf.edu/ushealthcaresystem/ Licensed under a Creative Commons Attribution 4.0 International License
Health IT is a term that is used for the electronic health systems that healthcare professionals and patients use to store, share, and analyze health information.
A technology tool that provides healthcare providers with knowledge and person-specific information to enhance decision-making.
The use of telecommunication and information technology to provide access to health assessment, diagnosis, intervention, consultation, supervision, and information across distance.
The delivery of synchronous healthcare services between the patient and the healthcare provider remotely.
The practice of monitoring aspects of a patient’s health from a remote location.
Also known as “store-and-forward." Providers review information asynchronously to diagnose or treat an issue.
The transmission of an individual's personal health and medical data to the healthcare provider in a different location for diagnosis and treatment.
Transmission of health information and services via mobile technology.
A comprehensive software solution designed to manage and organize patient-related data within healthcare facilities.

