What is Evidence-Based Practice?
Credit: Marcie Hopkins, U of U Health
EBP, or evidence-based practice, is a term we encounter frequently in today’s health care environment. But what does it really mean for the health care provider?
By: Barbara Wilson and Mary-Jean (Gigi) Austria
This article originally appeared December 18, 2019. It was updated to reflect current practice July 1, 2025.
July 1, 2025 | 4 minutes
Learning Objectives
After completing this lesson you will be able to:
- Define evidence-based practice (EBP)
- Describe the role of research and EBP in clinical practice
- Discuss the differences between research and EB
Case Study
Shay is a clinical nurse on the Bone Marrow Transplant & Hematology Inpatient Unit. She is assigned four patients, three of which have multiple blood products ordered. Throughout the day, Shay notices the Health Care Assistant (HCA) is “frazzled,” running from room to room to obtain frequent vital signs on these patients. A fall-risk patient in room 25 hits their call light to ask for help to the restroom, but the HCA is busy in room 31 with more vital signs. The patient decides to get up without assistance, and falls. Shay starts to wonder, “Is there a better way to do this?” She also realizes that she has never personally seen a blood transfusion reaction happen on the unit, and asks herself, “How often do transfusion reactions actually happen? Does the evidence support vital signs being done this frequently?”
What is evidence-based practice?
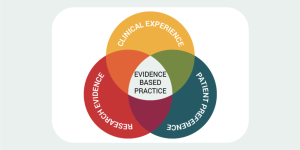
Evidenced-based practice (EBP) is applying or translating research findings in our daily patient care practices and clinical decision-making.
EBP also involves integrating the best available evidence with clinical knowledge and expertise, while considering patients’ unique needs and personal preferences. If used consistently, optimal patient outcomes are more likely to be achieved.
Using EBP means abandoning outdated care delivery practices and choosing effective, scientifically validated methods to meet individual patient needs. Health care providers who use EBP must be skilled at discerning the value of research for their specific patient population.
How to apply EBP in clinical practice
Evaluating all of the available evidence on a subject would be a nearly impossible task. Luckily, there are a number of EBP processes that have been developed to help health care providers implement EBP in the workplace.
The most common process follows these six steps:
1. ASK a question. Is there something in your clinical setting that you are wondering about? Perhaps you wonder if a new intervention is more effective than the one currently used. Ask yourself: What works well and what could be improved? And, more importantly, WHY? Evaluate the processes and workflow that impact, or are impacted by, the identified practice gap. We’ll use a format called PICO(T) (pronounced “pee ko”). Learn more about PICOT questions in the next module.
2. ACQUIRE the current evidence. You’ll do this by conducting a literature search. Your search will be guided by your clinical question.
3. APPRAISE the literature. Or, in other words, sort, read, and critique peer-reviewed literature. Additionally, learn the differences between Quantitative and Qualitative Approaches.
4. APPLY your findings to clinical decision-making. Integrate the evidence with clinical expertise and patient preferences and values. Then make evidence-based recommendations for day-to-day practice.
5. EVALUATE your outcomes. Review data and document your approach. Be sure to include any revisions or changes. Keep close tabs on the outcomes of your intervention. Evaluate and summarize the outcome.
6. DISSEMINATE the information. Share the results of your project with others. Sharing helps promote best practices and prevent duplicative work. It also adds to the existing resources that support or oppose the practice.
Though we may learn how to apply EBP by participating in project-based work, integrating EBP in our daily practice can help us strive to achieve the best possible patient outcomes. It requires us to be thoughtful about our practice and ask the right questions.
It’s important to note that although applying evidence at the bedside can be conducted individually, working collaboratively as a team is more likely to result in lasting improvement.
Before there was evidence…
As health care providers, delivery of patient care should stimulate questions about the evidence behind our daily practice.
For instance, there was a time when neutropenic patients were placed in strict isolation to protect them from developing life-threatening infections. Research findings were evaluated for best evidence and it was noted that using strict isolation precautions did not result in more favorable patient outcomes when compared to proper handwashing procedures coupled with standard precautions—and it seemed that we unnecessarily subjected patients to the negative psychological effects caused by extreme isolation.
As clinicians, we sometimes follow outdated policies or practices without questioning their relevance, accuracy, or the evidence that supports their continued use.
What’s the difference between research and EBP?
There is a common misconception that EBP and research are one in the same. Not true! While there are similarities, one of the fundamental differences lies in their purpose. The purpose of conducting research is to generate new knowledge or to validate existing knowledge based on a theory. Research involves systematic, scientific inquiry to answer specific questions or test hypotheses using disciplined, rigorous methods. For research results to be considered reliable and valid, researchers must use the scientific methods in orderly, sequential steps.
| Research | Evidence Based Practice |
| To generate new knowledge or validate existing knowledge based on theory. | To use best available evidence to make informed patient-care decisions. |
In contrast, the purpose of EBP isn’t about developing new knowledge or validating existing knowledge—it’s about translating the evidence and applying it to clinical practice and decision-making. The purpose of EBP is to use the best available evidence to make informed patient-care decisions. Most of the best evidence stems from research, but EBP goes beyond research and includes the clinical expertise of the clinician and healthcare teams, as well as patient preferences and values.




