How to Formulate Clinical Questions

Credit: Marcie Hopkins, U of U Health
You have a good idea about what you want to study, compare, understand or change. But where do you go from there? First, you need to be clear about exactly what it is you want to find out. In other words, what question are you attempting to answer?
By Tallie Casucci, Mary-Jean (Gigi) Austria, and Barbara Wilson
Mar. 5, 2021 | 3 minutes
Learning Objectives
After completing this lesson you will be able to:
- Explain the advantage of using the PICO(T) framework.
- Formulate searchable, answerable questions using the PICO(T) framework.
Case Study
Brandon is caring for an adult male who sustained a head injury. He wonders how intracranial pressure might be affected if he elevates the head of the bed slightly (say, 30 degrees) versus having the patient remain supine. Is one intervention more appropriate than the other? How should Brandon phrase his clinical question in an electronic database to produce the best results and find the most evidence-based recommendation
What is PICO(T)?
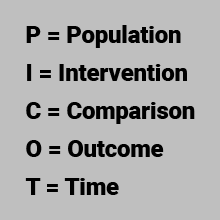
PICO(T) is an acronym to help clinicians formulate a clinical question.
The PICO(T) question framework is a consistent formula for developing answerable, researchable questions. Using PICO(T) guides you in your search for evidence and may even help you be more efficient in the process.
Why does it matter how we phrase a question?
Well, for one thing, there are millions of articles on a variety of topics. You might have access to massive electronic databases, such as PubMed, CINAHL, PsycINFO, Embase, and Scopus. Without a well-built PICO(T) question, it would be like searching in the dark for your flashlight—you know it’s somewhere but don’t know how to get to it.
PICO(T) gives us a consistent, systematic way to identify the components of a clinical issue. By using the PICO(T) format, we can structure the clinical question to help clarify the essential components, which then guides your search for evidence.
How do I use it?
Begin with a clinical problem or question
In our case study, Brandon is caring for an adult male who sustained a head injury. He wonders how intracranial pressure might be affected by elevating the head of the bed to 30 degrees versus remaining supine.
PICO(T) questions can fall into one of several types:
| Questions | Asks |
| Intervention or Therapy | “What is the best treatment or intervention?” |
| Prevention | “How can I prevent this problem?” |
| Diagnosis or Assessment | “What is the best way to assess?” or “What is the best diagnostic test for this patient?” |
| Etiology or Causation | “What contributed to this problem?” |
| Prognosis | “What are the long-term effects of this problem?” |
| Prognosis | “What is the meaning of this experience for patients?” |
Then, plug your question into the PICO(T) framework
Once you ask a clinical question, the PICO(T) format provides an effective framework. Let’s use this PICO(T) question as an example:
“In adult males with a head injury, how does elevating the head of the bed 30 degrees compared with a supine position affect intracranial pressure within the first 24 hours following injury?”
‘P’ stands for patient or population of interest. What are the most important characteristics of the group or patient(s) you are investigating? Defining features may include age, gender, ethnicity, disease processes or medical conditions. In our example, P would be “Adult males with a head injury.”
‘I’ represents the intervention or area of interest. Ask yourself, “What is the main intervention, treatment, exposure or prognostic factor I am considering?” In other words, “What treatment or intervention might be best for the patient? What are the factors you are considering that influence the patient’s prognosis?” In our example, I would be “elevating the head of the bed 30 degrees.” Keep in mind that not every question may have an intervention—particularly questions that focus on meaning or lived experiences.
‘C’ stands for the comparison intervention or group. Ask yourself, “What is the main alternative to compare with the intervention?” This could be a placebo or no disease or absence of a risk factor. Sometimes your question may not have a comparison! In research terms, C refers to the independent or predictor variable—something that influences the outcome variable or dependent variable. Again, using our example, C would be “supine position.” It is what we’re using to compare approaches or strategies.
‘O’ is the outcome. Ask yourself, “What am I aiming to accomplish, measure, improve, or impact? Am I trying to eliminate or relieve symptoms? Reduce the number or severity of adverse effects? Improve functioning?” In this case, our outcome, or dependent variable (in research terms), would be intracranial pressure.
‘T’ represents time. For this last stage you ask yourself, “What is the time it takes for the intervention to achieve an outcome?” Or, “How long are participants observed?” In our question, we wondered about the effect that the position of the head of the bed had on our patient’s intracranial pressure for the first 24 hours following his head injury.



