Disability Education in Medical Schools: A Paradigm Shift for Inclusive Care
Hannah Ship; Sahana Shankar; Rochelle Baer; Jeffrey Brosco; Jairo Arana; Damian Gregory; Robert Irwin; Gauri Agarwal; Sabrina Taldone; Sheryl Eisenberg Michalowski; Daniel Quintero; Anna Shah; Frank Woo; Michelle Schladant; and Ashley Falcon
Ship, H., Shankar, S., Baer, R., Brosco, J., Arana, J., Gregory, D., Irwin, R., Agarwal, G., Taldone, S., Eisenberg Michalowski, S., Quintero, D., Shah, A., Woo, F., Schladant, M., & Falcon, A. (2024). Disability education in medical schools: A paradigm shift for inclusive care. Developmental Disabilities Network Journal, 4(2), 132-143. https://doi.org/10.59620/2694-1104.1104
Disability Education in Medical Schools: A Paradigm Shift for Inclusive Care PDF File
Plain Language Summary
People with disabilities often face worse health outcomes because they struggle to access healthcare. Medical professionals do not always have the right training and sometimes have biases. This leads to unfair differences in healthcare.
To tackle this, we created a detailed 4-year medical school curriculum. It has three important sessions spread out over the years. The first session teaches students about working in healthcare teams and focusing on patients. The second session looks at disability culture, biases, and health differences. The third session focuses on communication and letting patients make choices.
We worked closely with people with disabilities to develop this curriculum. Their insights are crucial. We also involved the local disability community through community organizations. In this model, students can choose from optional classes and activities. This enriches their learning experience. Students who have used this curriculum have given positive feedback. They especially liked talking directly with people with disabilities. Research shows that these experiences really help students understand better and become more empathetic.
We hope other medical schools and institutions can use our model. It is important to make sure that people with disabilities get the same level of healthcare as everyone else.
Abstract
Disability education for medical students is often insufficient and can contribute to health disparities for people with disabilities. Our interdisciplinary curriculum development team created a longitudinal 4-year disability education model aimed at improving patient care for people with disabilities. Central to our curriculum are progressive sessions aligned with students’ medical journey, including three required sessions covering interdisciplinary healthcare teams, implicit bias, health disparities, disability culture, shared decision-making, communication, and self-determination. Through the inclusion of people with disabilities, an interdisciplinary curriculum development team, and trainee-driven advocacy, our longitudinal multi-phasic disability education curriculum seeks to mitigate health disparities. Our innovative approach addresses the gap in disability education, fostering more compassionate and inclusive healthcare practices.
Introduction
Background on Need
People with disabilities (PWD) face higher rates of health disparities compared to those without disabilities (Centers for Disease Control and Prevention [CDC], 2022; Kennedy & Swenor, 2023; Krahn et al., 2015). Health disparities are defined as poor health outcomes stemming from avoidable disadvantages, rather than solely from the disability itself. These disparities not only impact the health and well-being of PWD but also place an added burden on healthcare systems and contribute to inequities (Riley, 2012). PWD receive inadequate care from healthcare providers, often because of a lack of knowledge on how to provide appropriate care, resulting in worse health outcomes (McKee et al., 2011; Peiris-John et al., 2021). Given the general lack of sufficient training, coupled with negative biases, healthcare providers play a key role in the barriers to optimal care for PWD (Symons et al., 2009; World Health Organization [WHO], 2022) In fact, there have been many calls to strengthen medical education for healthcare workers in order to address health equity, from organizations ranging from the WHO, the CDC, and the U.S. Surgeon General in the “Call to Action to Improve the Health and Wellness of Persons with Disabilities” (Office of the Surgeon General, 2005; see also, CDC, 2020; Fitzpatrick & Barrett, 2023; WHO, 2022). The U.S. Health Resources and Services Administration (HRSA) recently published a report, “Strengthening the Adult Primary Care Workforce to Support Young Adults with Medical Complexity Transitioning to Adult Health Care Patients,” describing a health system shortage in adult primary providers able to treat people with a combination of chronic conditions, functional limitations, and intellectual and developmental disabilities (Ziemann et al., 2023). This warning about a health system shortage underscores the urgency and relevance of establishing comprehensive disability education for healthcare workers in all fields and specialties.
While it is necessary to require curricula on disability in medical education, barriers include a lack of space in the mandatory curriculum and faculty expertise in disability. In fact, longitudinal medical education curriculum in disability remains rare in medical schools, and only a few institutions, including the Ohio State University and the University of Miami Miller School of Medicine, have “expanded these didactics to longitudinal medical education curricula in disability to further increase and sustain knowledge, clinical skill, and cultural competency with people with disabilities” (Ratakonda et al., 2022, p. 1013). Advocates who are passionate about making changes to medical school curricula face many barriers, including gaining institutional support, finding time within the mandatory curriculum, and including community partners for an accurate representation of the community’s priorities. In this paper, we discuss our curriculum development process and how we convened an interdisciplinary curriculum team to creatively integrate disability content into the existing curricula to serve as a blueprint for others looking to replicate these efforts.
Brief Curriculum Overview
Our interdisciplinary curriculum development team created a longitudinal 4-year disability education model aimed at improving patient care for PWD. Central to our curriculum are progressive sessions aligned with students’ medical journey, including three required sessions covering interdisciplinary healthcare teams, implicit bias, health disparities, disability culture, shared decision-making, communication, and self-determination. Additionally, our curriculum is enriched by collaborations with the Leadership Education in Neurodevelopmental and related Disabilities (LEND) program and the Mailman Center, recognized as a University Center for Excellence in Developmental Disabilities (UCEDD). These partnerships contribute valuable insights and real-world perspectives, further enhancing the depth and authenticity of our educational approach.
Gaining Institutional Buy-In
Student Advocacy
A key driver in the development of the new longitudinal curriculum included the roles of trainees that spearheaded the development of the disability curriculum. Today’s trainees are passionate about causes and communities that may not have been historically well-represented in medical curricula (Eckleberry-Hunt et al., 2018). Through advocacy, trainees hope to help cultivate a curriculum that is more representative of the patient population they will all one day serve. Medical students were empowered to contribute to the sessions and to administratively direct the team of interdisciplinary health professionals. The involvement of several trainees helped to incorporate a medical student perspective and connect the curriculum with other institutions and advocacy groups.
Faculty Champions and Leadership Support
Strong leadership and institutional support were required to implement changes to the curriculum that represents the trainee perspective. Our institution benefitted from the guidance of a dedicated faculty champion, who was at the time overseeing the “Medicine as a Profession” curriculum. Even before implementing significant changes, our medical school had already introduced a session dedicated to disability medicine, featuring engaging panels involving PWD. However, a curriculum overhaul at our medical school in 2020 provided an opportunity for further expansion, led by our committed faculty champion. The engagement of leadership in disability medicine ensured institutional support, removing barriers to incorporating three separate sessions.
Curriculum Development Team
Team Composition
The curriculum was developed by an interdisciplinary team of health professionals, who volunteered their efforts based on expertise and passion. This included professions such as nurse practitioner, social worker, biostatistician, medical physician, health law practitioner, PWD, and medical student. This composition allowed for a comprehensive and authentic representation of perspectives that could be integrated into the medical curriculum.
Interdisciplinary Benefits
Furthermore, the sustainability of our curriculum is fortified by the involvement of a diverse team and trainees. While the initial curriculum was established under strong leadership, the transition in leadership and potential changes in any program have not hindered its continuity. Our strategy emphasizes self-sufficiency, passing down the advocacy and guardianship responsibilities of the materials through multiple cycles, and ensuring enduring relevance and evolution.
The interdisciplinary curriculum development team naturally gravitated toward sessions aligned with their expertise. The first session, “Interdisciplinary Health Professions,” was created by those on the team with more of a background in Physical Medicine and Rehabilitation. The second session, “Disability and Health Disparities,” by self-advocates and backgrounds in Medicine-Pediatric work; while the third session, “Communication in Special Settings,” by those with background in Deaf culture and the intersection of language and shared decision making. We found it best to allow individual passions to drive the content, within the reigns of the medical school institutional objectives. Curricular methods and learning objectives were decided in these groups, and then shared amongst leadership for oversight, ensuring diversification and progression across sessions.
Furthermore, our institution is fortunate to have cultivated strong relationships with the local disability community through the LEND program at our institution’s child development center. Collaborating with LEND faculty not only enriches the curriculum with real-world insights and opportunities, but also establishes a foundation for ongoing engagement, bridging the gap between academics and the experiences of PWD. This is also important for the guardianship and updates of the curriculum as time progresses and language or insights may change. For institutions that may struggle with formally integrating a mandatory curriculum, partnerships through LEND and other university and community organizations are an essential starting point to formally connect with PWD and enrich the development and allyship of trainees. As one of 60 LEND programs in the nation, these elements can be duplicated at other medical schools (LEND, 2023)
As mentioned above, these partnerships provide structure for the local involvement of PWD. Past research linking the greater burdens of disease faced by PWD, in part because of unmet healthcare needs, shows the harm that can come about for PWD when healthcare systems fail to learn from the lived experiences of their PWD and to adapt accordingly (Okoro et. al, 2018). To ensure that the content of this medical school curriculum was an authentic representation of what was important to PWD, the priorities of this curriculum were driven by the lived experiences of PWD. PWD were instrumental in the planning and execution of the curriculum. They shared critical expertise that is often lacking among professional medical educators, providing a rich resource for curriculum content. For example, all the activities for medical students in the prework consisted of direct representations of the lived experiences of PWD. Like many other components of the curriculum, these activities were proposed by team members with lived experience, such as a TED talk on “The Beauty of Disability” delivered by a person with a disability on our curriculum committee and an article guiding healthcare providers on delivering unexpected news to parents of an infant with Down Syndrome (Baer, 2011).
Longitudinal, Multiphasic Curriculum
Three Phases
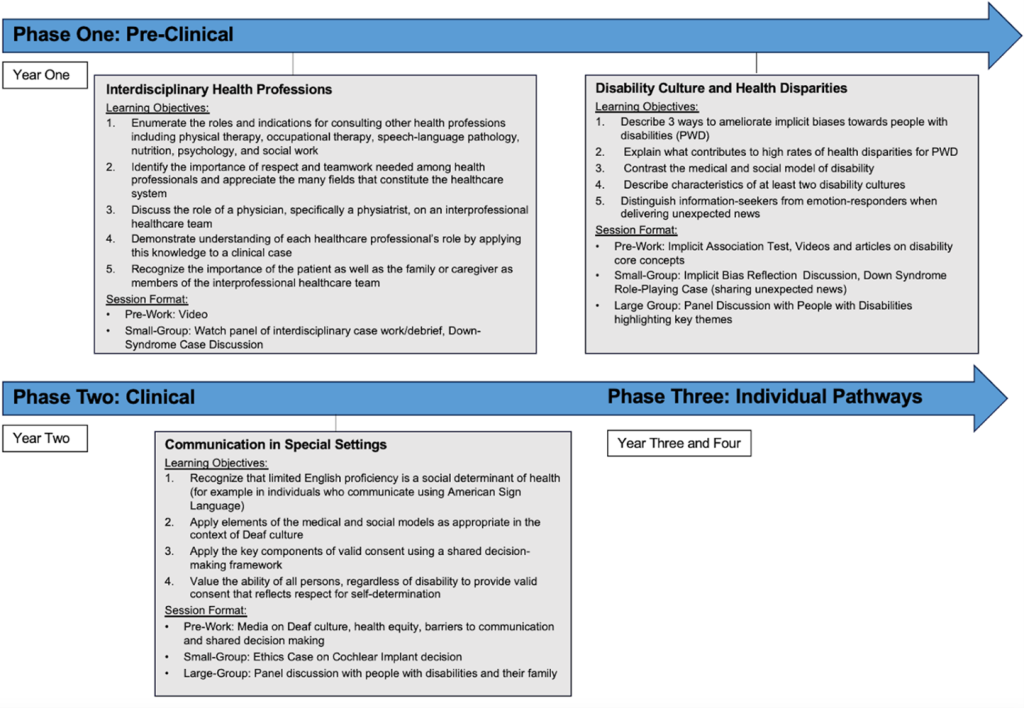
A new medical school curriculum entitled “NextGenMD” was created at the medical school with three phases (Figure 1). This includes Phase One, the pre-clinical education phase, which focuses on disease states and medical academics. Phase Two is the clinical phase, where medical students experience the clinical education environment through rotations through different specialties. Last, students experience Phase Three, Individual Pathways, in which students can specialize their education focus through more rotations and research courses.
Note. The new NextGen curriculum is divided into three phases: Phase one pre-clinical, Phase two clinical, and then Phase three individual pathways for specialization. The three Mandatory disability education sessions are the “Interdisciplinary Health Professions” session in Phase one, the “Disability Culture and Health Disparities” session at the end of Phase one, and the “Communication in Special Settings” session in the middle of Phase two.
Mandatory Curriculum, Elective Curriculum, and Extracurricular Activities
The 4-year innovative framework compromises three crucial components: mandatory curriculum, elective modules, and extracurricular activities—all designed to engage medical students throughout their program. Central to our curriculum’s design are three required sessions that explore key themes critical to competent disability care. This includes “Interdisciplinary Health Professions,” “Disability Culture and Health Disparities,” and “Communication in Special Settings.”
For the first session, the Phase One Interdisciplinary Health Professions session, key themes included person-centered medicine, interdisciplinary health teams, and caregivers as members of interdisciplinary health teams. The pre-session material includes a pretest, an introductory pre-learning video on the roles of different health professions, and the responsibilities of team members such as physiatrists, physical therapists, occupational therapists, speech-language pathologists, nutritionists, psychologists, and social workers. The Small-group session includes the viewing of an additional video and debriefing of an interdisciplinary team case. Students can engage in a case discussion on a patient with Down Syndrome and the opportunities for team work to better support the patient’s holistic needs.
The subsequent Phase One Disability Culture and Health Disparities session introduces core disability concepts, including the medical vs. social model, implicit bias, and health disparities. The session included prework, small-group learning, and a large-group panel. Specifically, the prework started with the Harvard Implicit Association Test on Disability (Moon, 2011). Students were given a series of articles and videos on disability, which included hearing directly from PWD. The small-group session included a pretest assessment, a facilitated discussion on the implicit bias test, and a role-playing case on delivering unexpected news with the case of new Down Syndrome diagnosis. The large-group discussion was led by PWD who debriefed the small-group and prework activities, shared their stories with specific disability themes, and provided opportunities for discussion.
Phase Two, Communication in Special Settings, builds upon the concepts described by the disability culture session including disability culture and the social model to exemplify the need for language justice, shared decision making and respect for patient self-determination. The prework included three videos, one article, and one optional research article. One of the prework videos was created by the curriculum team as a community needs assessment. This features interviews with people who are Deaf or hard of hearing, Deaf law advocates, and experts in the field discussing language justice, and Deaf health equity (Ship, 2021). The small-group session included a facilitated discussion on an ethical case describing a clinical discussion with two parents who are Deaf and their decision in obtaining a cochlear implant for their child. The large-group panel featured several members of the Intellectual Disability and Developmental Disability (IDDD) communities and their family members discussing their experiences interacting and communicating with healthcare teams.
Alongside these mandatory sessions, we have elective curricular activities and extracurricular activities. At the end of each mandatory session, students were given resources for further learning, including a website that described elective and extracurricular opportunities at the medical school. The elective curricula are curricula in which students can elect to, often during Phase Three. This includes the LEND program, the Physical Medicine and Rehabilitation sub-internship, and the Developmental-Behavioral Pediatrics elective.
On the other hand, extracurricular activities exist outside of the medical school transcripts. A variety of extracurricular activities exist including, The Debbie Project, Progression Across Transition in Healthcare (PATH) clinic, Student Emerging Leaders Program (SELP), Self-Advocate Leadership Training (SALT) Program, and Disability Awareness and Sensitivity in Healthcare (DASH). The Debbie Project is a medical school organization that provides opportunities for students to volunteer with typically and atypically developing children in a school and organizes programming where medical students can learn about disability and learn American Sign Language. Students involved with the PATH clinic have participated in the development of a clinic for adults with intellectual and/or developmental disabilities. SELP is a leadership program for high school students who have a special interest in disability and health, including students with disabilities and siblings or family members of someone with a disability. SALT is a leadership program for self-advocates. Students who participate in SELP and SALT have developed programming and led sessions. DASH initiatives that students have been involved in include the creation of a health passport and an educational video on healthcare provider best practices with respect to disability.
These additional opportunities, the elective curriculum, and the extracurricular opportunities provide easy access for further learning and immersion into the disability community. This approach is consistent with efforts in undergraduate and graduate education to allow learners to go in-depth on topics relevant to their interests and careers (Kim et al., 2023). Through the inclusion of mandatory curricular sessions, elective curricular offerings, and extracurricular activities, we share a wide range of disability education approaches, allowing for institutions to pick and choose educational activities that best fit their situation. This is especially relevant for institutions that have difficulty gaining institutional support or time within the mandatory curriculum. Given that these additional activities are not mandatory, recruitment and promotion strategies to encourage participation are utilized through student organizations and student communication outlets.
Alignment with Medical Training
The curriculum development team decided on three sessions to best provide students with longitudinal exposure and to best place material where it could be integrated into the traditional medical education for sustainability. Our longitudinal curriculum allows students to engage with disability content progressively over an extended period. This extended exposure fosters a deeper understanding of the themes of inclusion, culture, and self-determination surrounding disability care and promotes better retention of knowledge. Each session builds upon the one before, expanding upon the prior teachings to shed light on a deeper perspective. Furthermore, these mandatory sessions were created to strategically align with the students’ medical journey, allowing students to organically connect disability-related content to various medical disciplines, which they can then integrate into their clinical practice (Figure 1). For instance, the “Communication in Special Settings” session is administered during medical students’ clinical rotations, allowing them to experience daily patient-physician interactions and better understand the significance of shared decision-making, self-determination, and valid consent. Creatively repurposing elements from the existing general medical curriculum allowed us to seamlessly integrate disability-focused content. In this process, we found that weaving disability themes directly into the traditional medical curriculum (e.g., within a discussion of valid consent) was an effective strategy to ensure disability content inclusion.
Design Strategies
Our team utilized several design strategies when devising this curricular design. The curricular methods were shaped based off the parent course, in this case, the “Medicine as A Profession course format: 1 hour of allotted time for student prework and 3 hours of time for the small-group or combined large-group course. Most undergraduate medical school programs now have a similar formatting for education on aspects of social medicine. Our team prioritized personalized videos highlighting local resources and communities, direct panel interactions with PWD, and activities allowing students to directly apply their knowledge (role-play, small group discussions). Of note, standardized patients were not used, but were considered. While this is a strong technique for student learning, we wanted to ensure that only PWD would be cast to act as the patients with disabilities.
Evaluation Methodology
Assessments
The evaluation strategy for the curriculum includes post-session surveys assessing students’ increased confidence following the first session, as well as retrospective pre/post-session surveys for subsequent sessions. Additionally, both the initial and subsequent sessions included quizzes aligning with the curricular content. We found retrospective pre/post-session surveys insightful, allowing students to reflect on their learning experiences after the sessions, and avoid possible prospective self-reporting and social desirability biases.
Early Outcomes
A key finding from the results included the strong positive feedback students reported from their experiences in large group panels in both the Disability Culture and Communication in Special Settings sessions. Such comments include: “getting to see the stories firsthand and ask questions really allowed for a brilliant exchange of knowledge” that was “incredibly impactful” and “positively impacted me and many of my peers.” In fact, students’ main complaints included not having the opportunity and time to engage more with the panel participants. This aligns with current disability education research that upholds direct interaction with PWD as the best form of disability culture education (Pettigrew et al., 2011).
Sustaining and Improving
Community Partnerships
Our institutional partnerships, particularly through programs like LEND and collaborations with other university and community organizations, have played a pivotal role in creating a meaningful connection between our medical school and PWD. These partnerships have enriched our students’ exposure to diversity and provided valuable insights into the lived experiences of PWD. To ensure the continued success of our disability education initiatives, we aim to continue to focus on sustaining, improving, and adding to our community partnerships. Moving forward, we plan to implement initiatives that strengthen the impact of our partnerships, such as organizing joint events, educational workshops, or panels where students can interact directly with PWD. Not only does this enhance the diversity of lived experience to which our students are exposed, but this also ensures that the curricular content remains relevant and responsive to the evolving needs of the disability community. Research shows that mere awareness of implicit bias is insufficient; meaningful exposure to PWD is more effective in changing behavioral outcomes (Gino & Coffman, 2021). By actively nurturing these partnerships, we aspire to create a mutually beneficial environment that not only supports our educational goals but also contributes to the broader objective of fostering inclusivity within the healthcare community.
Ongoing Assessments
It can be difficult to demonstrate success in education, especially related to skills in empathy and cultural humility. Furthermore, without a randomized control trial or standardized patients over a long interval, it is very difficult to demonstrate long-term retention or changes in practice. However, we continue to assess the curriculum yearly to ensure we meet the highest standards of education and inclusivity. Our teams have also begun studying and assessing the effectiveness of nonmandatory offerings as well (e.g., the educational videos shown in DASH). Our assessment strategy extends beyond quantitative metrics, considering qualitative data that captures the impact on students’ attitudes, perceptions, and behaviors towards disability care. This holistic approach allows us to adapt the curriculum in real-time, ensuring that the content remains current, engaging, and aligned with the evolving landscape of healthcare. We aim to expand the assessment strategy by tracking students’ attitudes and behaviors longitudinally after graduation to provide valuable insights into the long-term impact of the curriculum.
Conclusion
Call to Action
We stand at a crucial juncture in medical education, where the imperative for inclusive and patient-centered practices demands immediate attention. It is dependent upon medical educators and healthcare institutions to champion inclusivity within healthcare.
Summary
Overall, the disability education curriculum developed at our institution can serve as a blueprint for other medical schools looking to update their curricula. Central to this model is a longitudinal, multiphasic curriculum comprising mandatory sessions, elective modules, and extracurricular activities. The three mandatory sessions, “Interdisciplinary Health Professions,” “Disability Culture and Health Disparities,” and “Communication in Special Settings” serve as the cornerstone. We emphasize the importance of weaving disability themes directly into the traditional medical curriculum, using existing structures for seamless integration and ensuring community involvement for direct engagement with diverse, lived experiences. Furthermore, our curriculum development team, including people with lived experience, ensures a comprehensive representation of perspectives.
In providing patient-centered, inclusive medical education, we hope to nurture a generation of healthcare providers who possess a deep appreciation for the needs and rights of PWD. We hope that our blueprint will encourage medical educators, policymakers, and other healthcare institutions to champion inclusivity within healthcare, whether through updated medical education curricula, policy changes, or enhanced clinical pathways. Beyond its impacts on population health, an inclusive culture and robust disability education can provide the added benefits of improved patient-provider relationships, enhanced cultural competence, and greater patient satisfaction (Georgetown University Health Policy Institute, 2003). By promoting disability education, we hope to address health disparities and improve care for PWD across the healthcare system.
References
Baer, S. (2011, October). The Beauty of Disability [Video]. TEDxMIA. https://www.youtube.com/watch?v=xX1Job6O60E
Centers for Disease Control and Prevention (CDC). (2020). Disability and health information for health care providers. https://www.cdc.gov/ncbddd/disabilityandhealth/hcp.html
Centers for Disease Control and Prevention (CDC) (2022). Health equity for people with disabilities. https://www.cdc.gov/ncbddd/humandevelopment/health-equity.html
Eckleberry-Hunt, J., Lick, D., & Hunt, R. (2018). Is medical education ready for generation Z? Journal of Graduate Medical Education, 10(4), 378-381. https://doi.org/10.4300/jgme-d-18-00466.1
Fitzpatrick, S., & Barrett, D. (2023). Disability inclusion in medical education: Towards a quality improvement approach. Medical Education, 57(1), 17-20. https://doi.org/10.1111/medu.14952
Georgetown University Health Policy Institute. (2003). Cultural competence in health care: Is it important for people with chronic conditions? https://hpi.georgetown.edu/cultural/
Gino, F., & Coffman, K. (2021). Unconscious bias training that works. https://www.hbs.edu/faculty/Pages/item.aspx?num=61119
Kennedy, J., & Swenor, B. (2023). It’s time for the NIH to formally designate people with disabilities as a US health disparity population. Disability and Health Journal, 16(3), 1-4. https://doi.org/10.1016/j.dhjo.2023.101468
Kim, S., Jeong, H., Cho, H., & Yu, J. (2023). Extracurricular activities in medical education: An integrative literature review. Bio Med Central Medical Education, 23(1), 9198-9206. https://doi.org/10.1186/s12909-023-04245-w
Krahn, G. L., Walker, D. K., & Correa-De-Araujo, R. (2015). Persons with disabilities as an unrecognized health disparity population. American Journal of Public Health, 105(Suppl 2), S198-206. https://doi.org/10.2105/ajph.2014.302182
Leadership Education in Neurodevelopmental and Related Disabilities (LEND). (2023). https://mchb.hrsa.gov/training/projects.asp?program=9
McKee, M. M., Barnett, S. L., Block, R. C., & Pearson, T. A. (2011). Impact of communication on preventive services among deaf American Sign Language users. American Journal of Preventative Medicine, 41(1), 75-79. https://doi.org/10.1016/j.amepre.2011.03.004
Moon, T. R. (2011). Project Implicit: Implicit association test. https://implicit.harvard.edu/implicit/takeatest.html
Office of the Surgeon General. (2005). The Surgeon General’s call to action to improve the health and wellness of persons with disabilities. In Office on Disability (Ed.). Office of the Surgeon General. https://www.cdc.gov/ncbddd/disabilityandhealth/pdf/whatitmeanstoyou508.pdf
Okoro C.A., Hollis, N.D., Cyrus A.C., Griffin-Blake, S.(2018). Prevalence of disabilities and health care access by disability status and type among adults — United States, 2016. Morbidity and Mortality Weekly Report, 67(32), 882–887. http://dx.doi.org/10.15585/mmwr.mm6732a3
Peiris-John, R., Jain, N. R., Hogan, A., & Ameratunga, S. (2021). Educating health science students about disability: Teachers’ perspectives on curricular gaps. Disability Health Journal, 14(1), 100985. https://doi.org/10.1016/j.dhjo.2020.100985
Pettigrew, T. F., Tropp, L. R., Wagner, U., & Christ, O. (2011). Recent advances in intergroup contact theory. International Journal of Intercultural Relations, 35(3), 271-280. https://doi.org/10.1016/j.ijintrel.2011.03.001
Ratakonda, S., Argersinger, D. P., Auchus, G. C., McGowan, C., Ship, H., Wang, D. R., & McKee, M. M. (2022). A call for disability health curricula in medical schools. Trends in Moleculal Medicine, 28(12), 1012-1015. https://doi.org/10.1016/j.molmed.2022.08.004
Riley, W. J. (2012). Health disparities: Gaps in access, quality and affordability of medical care. Transactions of the American Clinical and Climatological Association, 123, 167-172. http://www.ncbi.nlm.nih.gov/pmc/articles/pmc3540621/
Ship, H. (2021). Hearing and listening: Health equity, deaf culture, and communication for healthcare professionals. https://youtu.be/TD5VrsaEWMw
Symons, A. B., McGuigan, D., & Akl, E. A. (2009). A curriculum to teach medical students to care for people with disabilities: Development and initial implementation. Bio Med Central Medical Education, 9, 78. https://doi.org/10.1186/1472-6920-9-78
World Health Organization. (2022). Global report on health equity for persons with disabilities. Geneva: World Health Organization. https://www.who.int/publications/i/item/9789240063600
Ziemann M., Salsberg E., McManus M., White P., Schmidt A. (2023). Strengthening the adult primary care workforce to support young adults with medical complexity transitioning to adult health care. George Washington University. https://gottransition.org/resource/?strengthening-adult-primary-care-workforce-medical-complexity-hct

