Toward an Equity-Driven Conceptual Model of COVID-19 Vaccine Decision-Making for People with I/DD
Lydia Ocasio-Stoutenburg; Reese Triana; Shelly Baer; Jairo Arana; Ana Carolina G. Sale; Douglene Jackson; Michelle Schladant; Nastasia Boulos; Grace Dima; and Jeffrey Brosco
Ocasio-Stoutenburg, Lydia; Triana, Reese; Baer, Shelly; Arana, Jairo; Sale, Ana C.; Jackson, Douglene; Schladant, Michelle; Boulos, Nastasia; Dima, Grace; and Brosco, Jeffrey (2023) “Toward an Equity-Driven Conceptual Model of COVID-19 Vaccine Decision-Making for People with IDD,” Developmental Disabilities Network Journal: Vol. 3: Iss. 2, Article 10.
Plain Language Summary
COVID-19 is a public health emergency, causing serious illness in the U.S. Many people with disabilities and people of color have already had barriers accessing healthcare and other things they need. COVID-19 has had an even greater impact on these communities, especially people who are Black, Hispanic/Latino, Native, and people with intellectual and developmental disabilities (I/DD). Even though the COVID-19 vaccine is effective and safe, not everyone has access to the vaccine or has trust in it. In this paper, we discuss how we developed a model for vaccine decision making for people with I/DD. We reviewed research and talked with communities to help us understand what affects vaccine decisions. The findings show how complex the decisions are, especially since people with I/DD do not always make health decisions on their own. Many factors like history, communication, and the news affect people’s vaccine decisions. Because barriers still exist for people with I/DD, fairness and trust can help people feel supported in their decisions. This model can help public health and policymakers learn what works to build confidence and better support people’s needs.
Abstract
COVID-19 presented a public health emergency in the U.S., resulting in severe illness, hospitalizations, high mortality rates, and long-term adverse health care conditions. Several studies examined the disparities in transmission rates, barriers to care, and negative health outcomes for persons with disabilities, particularly people with intellectual and developmental disabilities (I/DD). While data revealed similar trends among Black, Hispanic or Latino/a/x/e, Native, Indigenous, and Asian people, outcomes are compounded for people of color with I/DD. Several historical, pervasive, systemic, structural, and attitudinal barriers have constrained healthcare access and adequate treatment, instigating feelings of distrust among those in systems of care. Although vaccination is effective in minimizing adverse outcomes, COVID-19 vaccine policies and rollouts have also followed inequitable patterns in distribution and accessibility. To better address the concerns and needs of communities, a multidisciplinary team at a University Center of Excellence in Developmental Disabilities (UCEDD) engaged in a generative, multistep, systematic process to explore factors that influence vaccine confidence among people with I/DD, their families, and support circles, particularly people of color with IDD. Garnering data and input from multiple sources, we uncovered several complexities around vaccination, which include (a) accessibility; (b) context, history, and sociocultural concerns; (c) policies; (d) communication and media; and (e) a continuum of vaccine confidence and supported decision-making. Findings from these efforts underscore the centrality of equity and trust, with implications for practitioners, institutions, policymakers, and public health strategists. Furthermore, our model can serve as a useful framework for people invested in promoting healthcare equity in vaccination for people with I/DD and with multiple marginalized identities.
Introduction
A novel coronavirus, SARS-CoV-2, known as COVID-19, introduced a global public health crisis, responsible for a significant number of acute illnesses, disruptions to multiple areas of well-being, complex long-term health conditions, and deaths. The total number of COVID-19 cases in the U.S. has reached 94.5 million according to the most recent estimates from the Centers for Disease Control (CDC), with over 1.04 million reported deaths (CDC, 2022). While this continues to be an urgent situation at the broader level, the pandemic has also shed light on a complex array of persisting systemic health inequities that disproportionately impact the disability community, especially people with an intellectual and developmental disability (I/DD), communities of color, and people of color with I/DD.
COVID-19: Population, Community, and Individual Impacts
People with disabilities (PWD) represent approximately 1 in 4 persons in the U.S. Research studies examining the health experiences and outcomes for PWD in the population have revealed significant health inequities, disparate care, and adverse outcomes prior to the outbreak of COVID-19. For example, 1 in every 3 PWD have an unmet health care need or do not have a healthcare provider (CDC, 2022). The reality is even more concerning for persons with I/DD, who are more likely than other PWD or people without disabilities in the population to have additional unmet healthcare needs, such as unemployment, underemployment, food insecurity, and inequitable housing (CDC, 2022; National Institute of Minority Health and Health Disparities [NIMHD], 2022). Since the onset of the pandemic, studies have reported how individuals with I/DD are more likely to experience hospitalizations because of COVID-19-related complications, barriers to care, long-term adverse health outcomes, and death (Administration for Community Living [ACL], 2021; Chakraborty, 2021; Gleason et al., 2021; Landes et al., 2021). Data has also reported that individuals with I/DD also have fewer options for housing and are also more likely to reside in congregate settings, which raises exposure rates to COVID-19 and limits access to adequate care (Larson et al., 2020; National Council on Disability [NCD], 2021). Further magnifying the risks of infection for people with I/DD, studies have shown that many direct support professionals (DSPs) and staff who provide care in these settings may be unvaccinated against COVID-19 (Unroe et al., 2021). The NCD’s annual report in 2021 entitled, The Impact of COVID-19 on People with Disabilities, outlined COVID-19’s disparate impact on the lives of PWD, with an even greater number of adverse outcomes for people with I/DD.
Similar to people with I/DD, people of color and especially people of color with I/DD have also experienced high rates of COVID-19 transmissions as well as inequities in COVID-19 treatments and outcomes, magnifying the disparities in care predating the pandemic (Davis & Mendez, 2022; NIMHD, 2022; Underhill & Johnson, 2021). Data on intersectionality experienced among Black, Hispanic, or Latino/a/x/e, and Native communities with I/DD has revealed even greater inequities in COVID-19 transmission rates, care, and outcomes (ACL, 2021; Chakraborty, 2021). Further compounding this issue are the immediate and long-term impacts of COVID-19, which are still being researched. Many of the impacts of the pandemic on long-term health, as well as the impacts on other life domains such as recreation, education, employment, social and emotional well-being, community integration, and mental health are still under investigation (NCD, 2021). To many, returning to post-pandemic life means returning to confinement, to low-paying jobs, or to no job at all. The new normal can certainly mean going back to the status quo or something even worse. The new normal can be an opportunity to right the wrongs PWD face. These problems reflect an ongoing failure to consider PWD as equal members of the community, with equal human and civil rights—a fundamental issue of ableism with potentially catastrophic consequences for PWD in the COVID-19 pandemic and beyond. Studies show the social and mental health impacts on PWD across the lifespan during the pandemic, whose connection to community, support services, medical and therapeutic care, and agencies that sustain coordination of care were disrupted.
The COVID-19 Vaccine: An Urgent Response
Vaccination is an important healthcare advancement in response to outbreaks that threaten the general health and well-being of individuals (Dubé et al., 2013). Coupled with other safety measures, vaccination is among the most effective means of controlling infection rates at the population level, while also promoting individual-level immunity to viruses that could be deadly (Ehreth, 2003). The classification of COVID-19 as a pandemic by the World Health Organization (WHO, 2020) called for an urgent and unprecedented response for protection at the population level, through the development of the vaccine coupled with shelter-in-place orders, and other nonpharmaceutical interventions (Rodrigues & Plotkin, 2020). The approval of the COVID-19 vaccines developed by pharmaceutical companies by the U.S. Food and Drug Administration was but one step; the next was to determine the best pathway for dissemination to the public.
A Health Care Equity Framework
The complexities of these phenomena call for attention to the disparities in health care prior to the pandemic in order to understand how a public health crisis can have differential effects on populations. Stratifications in care and systemic barriers were magnified since the COVID-19 outbreak. Equity-focused research has called for attention to the pandemic outcomes, while also examining pre-pandemic conditions, to avoid the errors of assigning causality to group affiliation (Khazanchi et al., 2020). Braveman and Gruskin (2003) provided an important emphasis on distinguishing healthcare inequities from inequalities, as the latter tends to encompass a deterministic view of adverse healthcare outcomes that fail to account for systemic barriers and can target discrimination toward individuals and communities, reinforcing the pervasiveness of stigmatization. These researchers further defined health care equity as the explicit removal of inequitable barriers, policies, and practices that disproportionately impact populations (Braveman & Gruskin, 2003). In the context of COVID-19, such a framing is essential for understanding how inequities have been magnified because of already existing systemic barriers, discrimination, and inaccessible supports (Davis & Mendez, 2022; NIMHD, 2022).
This development of the model also embraces the conceptualization of intersectionality, as originally put forth by Crenshaw (1989) to understand the phenomenon of magnified oppressions based on holding multiple identities that have been historically marginalized. Furthermore, Tawara Goode, executive director of the Georgetown University National Center for Cultural Competence (NCCC) has expanded health care inequity definition by Braveman and Gruskin (2003) to follow Crenshaw’s conceptualization of intersectionality, focusing on the urgent need to address racial equity for persons with I/DD (Goode, 2019).
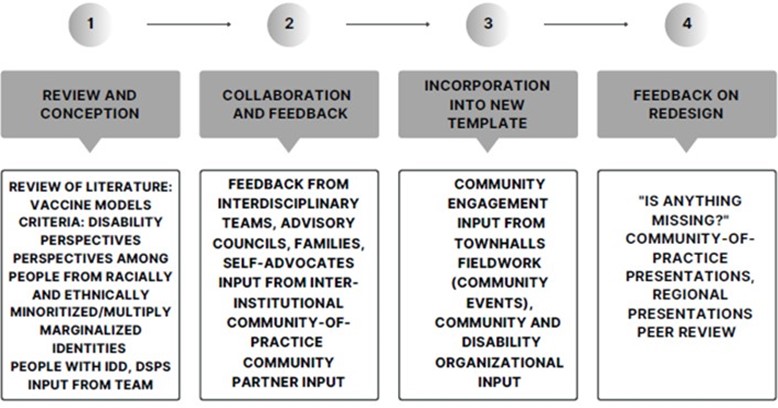
Toward an Equity-Driven Comprehensive Model
The focus of our team’s efforts was to examine the multiplicity and complexities of contributing factors and incorporate them into an equity-driven conceptual model for understanding vaccination decision-making. To capture the range of information and their nuances, we synthesized and incorporated findings from the literature, feedback from our community-academic partnerships and interdisciplinary teams, and infused a contextual understanding.
Methods
Setting and Context
This inquiry is part of a year-long initiative to address COVID-19 transmission at a University Center for Excellence in Developmental Disabilities (UCEDD) in a large southeastern region of the U.S. The ACL, funded by the U.S. Department of Health and Human Services, provided grant support to multiple entities to bolster vaccination efforts, including UCEDDs, who serve individuals with disabilities, their families, and communities. While many PWD and individuals with I/DD reside in long-term care settings, they may live in community residences, with family members, or may live alone, receiving support from their DSPs. A community-centered, capacity-building, interdisciplinary, and collaborative approach has been shown to be more effective in minimizing COVID-19 transmission than a universalist approach, particularly with populations where systemic barriers, inequities in access to healthcare, and disparate health outcomes persist (Underhill & Johnson, 2021; Wrigley-Field et al., 2021). As such, our goal was to work within our center, as well as through community-academic partnerships with neighboring communities representing culturally and linguistically diverse groups that have been historically and economically disenfranchised (Ocasio-Stoutenburg et al., 2023). The goals of our initiatives, entitled For Communities with Communities, were to bolster access to COVID-19 information, provide essential connections to vaccination sites, and increase disability-responsive supports. These communities are comprised of residents who may identify as (a) Black (African American, Caribbean and/or Haitian), (b) non-Hispanic White, and (c) Hispanic or Latino/a/x/e.
Review of Existing Models
At the onset of our initiatives to mitigate COVID-19 transmission and promote accessibility in our community in 2021, we searched the literature for a conceptual model to encompass the factors that influence vaccine decision-making. Although our initial search was to find models to account for the specific considerations related to the COVID-19 pandemic, we expanded the search to include models that described any population-level vaccination strategies, including those outside of the U.S. Excluding models that were not applicable, we narrowed our findings to eight, included within five publications. A summary of these studies’ contributing factors is found in Table 1. None of the models explicitly included equity or disability perspective. The model by Dubé et al. (2013) was selected because it included many of the considerations found in the literature and discussed among our team, while also being the most adaptable for incorporating additional concepts. This model also best suited our goal to deliver information in an accessible manner to the public.
| Authors | Model Strengths, Focus, and Contributing Perspectives |
|---|---|
| Dube et al. (2013) | Cultural and religious views influencing vaccine hesitancy. The role of media consumption on vaccine decision-making. Trust as a key factor. |
| Kaufman et al. (2017) | Focus on communication strategies. The role of multiple actors influencing individual decision-making. Multidirectional pathways are involved. |
| Ozawa et al. (2016) | Multiple, complex interactions among systems that influence trust. The role vaccinations play in adding stability to health care systems. Series of causal feedback loops as the design. |
| Adamu et al. (2020) | Interlinkage of systems as a focus; COVID-19 with routine childhood immunizations. A combined systems-level and implementation science approach. |
| Mahmud et al. (2021) | Causality diagram, illustrating the complexity of mediating social and structural factors. Several confounding variables which explain variations in vaccine uptake by race and ethnicity. |
Garnering Feedback to Inform the Model
Our next step was to garner some interdisciplinary and community feedback on our developing model. We presented our project and the draft of the model across five interprofessional collaboratives (IPCs) within our center, which were comprised of practitioners across disciplines, community leaders, self-advocates, and family members. Several of these individuals were PWD and/or parents of children and adults with I/DD. In addition, we presented the model to our UCEDD’s community advisory council. Across each group, we asked the question, “Is there anything missing from this model that would be important to understanding vaccine decision-making for people with I/DD?” Members shared the concerns they encountered in their practices as well as in the communities in which they engaged. Finally, we presented this model to communities of practice at other UCEDDs across the U.S. and tribal territories, as well as locally within our community-academic partnerships. Frequent discussions with our partners across COVID-19 coalitions included other UCEDD center leaders, self-advocate leaders, community residents, community builders, and organizational leaders.
Findings
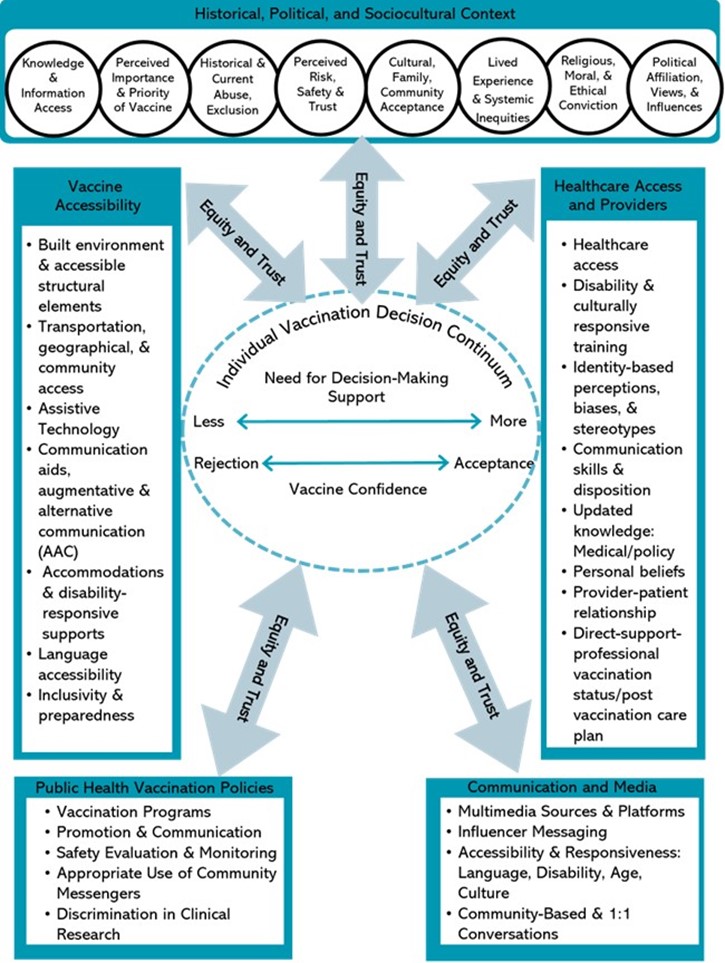
The adapted model can be found in Figure 1, whose major concepts focus on the following areas (a) Accessibility Barriers; (b) Historical, Political and Socio-Cultural Context; (c) Health Professionals Decision-Making; (d) Public Health and Vaccination Policies; and (e) Communication and Media. At the very center of this model, along a continuum, is the (f) Decision-Making about the Vaccine. Within each of these domains, the input from multiple sources is infused.
Accessibility Barriers
Decisions concerning rollout of the vaccine introduced additional challenges that have in turn had a negative impact on outreach, which include perceptions about the vaccine, misinformation, access barriers, and the delays in prioritization which followed patterns of inequity (Coustasse, et al., 2021; Momplaisir et al., 2021; NIMHD, 2022; Rodigues & Plotkin, 2020; Underhill & Johnson, 2021). The disability movement has legitimate questions about prioritization of persons with disabilities and their support networks to vaccinations, accessibility of vaccination processes, related information and venues, and provision of vaccines based on free and informed consent of all persons with disabilities. Sites (where vaccinations are delivered) should be made physically accessible, with live guidance and assistance provided for those who need it. Free or low-cost targeted programs for accessible transportation should also be provided where necessary. Furthermore, several responses both reflected and perpetuated discriminatory attitudes and perceptions.
Accessibility Barriers Among PWD
Acknowledging the aforementioned higher rates of COVID-19 transmission and negative health outcomes among PWD, studies revealed several structural and systemic barriers preventing accessibility to the vaccine. The initial phase of the vaccine dissemination in 2021 prioritized immunization among health care personnel, staff, and employees at long-term care facilities, with lag in eligibility for PWD (Iadarola et al., 2022; Painter et al., 2021). Variation in state policies regarding rollout in the subsequent phases of dissemination resulted in many PWD continuing to be left behind. The National Immunization Survey Adult COVID Module (NIS-ACM) was administered between May and June 2021 to assess vaccination status and perceptions among PWD. This survey reported the lower rates of COVID-19 vaccination among PWD as compared with individuals without disabilities (Ryerson et al., 2021). While a commonly attributed reason for lowered vaccination rates is often vaccine hesitancy or refusal, the unvaccinated respondents with disabilities expressed their intent to receive the vaccine and were more likely to perceive the vaccine as an important protective measure against COVID-19 infection than their counterparts without disabilities (Ryerson et al., 2021). Furthermore, respondents with disabilities cited accessibility barriers as the primary reasons for their unvaccinated statuses. Additional studies have described barriers that are both structural and systemic in nature. The NCD, for example, reported on the number of people with I/DD living in congregate and group settings who were unable to get to a vaccination site because of transportation and other accessibility barriers, thereby increasing their exposure and vulnerability to COVID-19 (NCD, 2021).
In February 2021, our center held monthly meetings for disability self-advocates who convened as alumni of a leadership training program. Selecting COVID-19 vaccination as their topic of choice, self-advocates were concerned about the inequitable distribution of the vaccine, emphasizing how PWD were not prioritized. With subsequent meetings after the rollout of Phase 1a and 1b, which would include PWD, self-advocates continued to describe persisting accessibility barriers, including a lack of transportation to vaccination sites, long lines at the pop-up sites, and a lack of accommodations across individuals’ physical, sensory, social, emotional, or behavioral needs. This may include personnel training, reducing barriers in the built environment, or permitting support animals at sites.
Accessibility Barriers Among People With I/DD
Although strategies have been implemented over time to promote access to COVID-19 vaccine though funding and strategic efforts to support the disability community, many barriers persist for PWD, particularly for persons with I/DD. State protection and advocacy organizations, for example, have offered services to cover these gaps, which include support for individuals experiencing physical and mobility barriers at vaccination sites and clinics. However, as Ryerson et al. (2021) explained, while health care providers at vaccination sites are mandated to remove any physical barriers per the Americans with Disabilities Act (ADA, 1990), there are few provisions for people with I/DD, people requiring sensory supports, people requiring ASL support, or an interpreter for people who are Deaf or hearing impaired.
Accessibility Barriers Among Communities of Color
In addition to the concerns for people with I/DD, several concerns have been raised about vaccination among communities of color and people of color with I/DD, who have been disproportionately impacted by COVID-19. Despite the higher rates of transmissions and negative health outcomes, data collected from the initial rollout showed that Black and Hispanic or Latino/a/x/e communities were less likely to receive the COVID-19 vaccine than their White counterparts (Ndugga et al., 2022; Underhill & Johnson, 2021).
Engagement in discussions in biweekly communities of practice (CoP) meetings with other UCEDDs across the country allowed for cross-center sharing of insights and perspectives, as well as strategies for understanding. Several other centers described the inaccessibility of the vaccine within rural communities, despite the high rates of COVID-19 infection among Native populations residing in tribal lands across the country. “We are losing our elders,” was a comment shared in one of the CoP meetings regarding the loss of life in the Native communities to COVID-19, including Native persons with disabilities, for whom healthcare and access barriers were already an identified challenge.
Existing systemic barriers were also identified by the groups within our community members who are a part of our community-academic partnerships. Biweekly discussions with our partners in a COVID-19 coalition, which included residents, community builders, and organizational leaders, provided insights on the concerns over pre-pandemic disparities that had gone unresolved, for which vaccine access had followed. For example, the community residents in one historically Black community described initial funding from the state’s Department of Health at the height of the pandemic to provide local community pop-up sites, which had closed down over time. Attendees of these meetings expressed concerns among working residents about not having the ability to take days off to deal with post-vaccination symptoms, and a lack of adequate health insurance coverage if they were to become ill. Members from our Hispanic or Latino/a/x/e communities, many of whom were from Mexico, Honduras, Guatemala, and other countries, described their access barriers to vaccination, since many sites required proof of residency, restricting access for many migrant families. Many of the migrant families within the Haitian communities expressed similar concerns about these policy barriers. Additionally, linguistic barriers were also expressed by many of the migrant families, who spoke various Indigenous languages.
Access Barriers Among People of Color with I/DD
What are the concerns among people of color with I/DD? As previously mentioned, while there are few studies that capture the perspectives on COVID-19 vaccination among persons with I/DD, there are even fewer studies to date that focus exclusively on the perspectives among Black, Hispanic or Latino/a/x, and Native communities with I/DD. In the aforementioned national survey by Iadarola et al. (2022), concern about being used as a medical experiment was highly cited as a reason for vaccine hesitancy among the Black and Hispanic groups, representing 96% and 91% of these respondents, respectively, as compared with their White (76%) and Asian (67%) counterparts in the study. In addition, 95.6% of Black respondents in the sample cited mistrust of the government as a primary reason for vaccine concern, consistent with the literature on the concerns within the Black community overall.
Historical, Political, and Sociocultural Perspectives
Several concerns have been raised about vaccination among PWD, communities of color, and people of color with I/DD who have been disproportionately impacted by COVID-19. While some studies have reported a general feeling of trust in the COVID-19 vaccine among PWD as a protection against the virus, other studies have reported vaccination hesitancy. This was a particular concern among people of color. Studies have reported how people of color were hesitant because of the timing in which the vaccine was developed, worried about the side effects post-vaccination, and had even greater concerns about the unknown effects of the vaccine long-term (Jimenez et al., 2021; Momplaisir et al., 2021). Such concerns were echoed within our community advisory councils, where representatives and family members expressed how they knew of people who had suffered side effects. These reports had increased hesitancy within the community.
Mistrust of the medical community was also reported among studies within the Black community. A historical mistrust, because of maltreatment and medical experimentation on people of color, has been highly cited as a reason for vaccine hesitancy (NIMHD, 2022; Underhill & Johnson, 2021). In addition, studies also reported a current mistrust of the sociopolitical climate, which led to a lack of trust in the government-issued interventions (Jimenez et al., 2021; Momplaisir et al., 2021; Underhill & Johnson, 2021). Focus group participants in a qualitative study by Momplaisir and colleagues cited their current mistrust of government as a reason for their hesitancy.
The literature providing descriptive data about vaccination decisions among persons with I/DD is scant, with even fewer studies capturing perceptions about the vaccine among this population. One survey conducted between January and February 2021 among two UCEDDs in New York, in partnership with the state’s Developmental Disabilities Planning Council, sought to explicitly focus on the vaccination status and perceptions among persons with I/DD. Inclusion criteria for this survey was identification as a person with I/DD, a family member of a person with I/DD, or a person who works with people with I/DD (Iadarola et al., 2022). The representative sample (n = 875) included four groups identified by racialized or ethnic descriptor as Asian, Black, Hispanic, or White. Across the sample, one of the most cited reasons for vaccine concerns was the newness of the vaccine, represented by 67% of Asian respondents, 93% of Black respondents, 100% of Hispanic respondents, and 95% of White respondents (Iadarola et al., 2022). In addition, participants in this study described the potential side effects of the vaccine as a main concern, represented by 67% of Asian respondents, 97.8% of Black respondents, 100% of Hispanic respondents, and 97.3% of White respondents.
Context matters with regards to vaccine decisions, as people and communities are situated within social, historical, cultural, economic, and political realms (Dubé et al., 2013; Kumar et al., 2016). Research has emphasized how vaccine decision-making should be understood as part of both broader and local social contexts. Individual vaccine decision-making is greatly impacted by systemic realities that exist on a macrolevel as well as the daily microlevel experiences, which may include family histories and health care experiences (Dubé et al., 2013). Dubé et al. referenced several key concepts developed by other researchers studying vaccination, while also emphasizing the shifting role of the patient-as-consumer.
Streefland and collaborators use the expression “local vaccination cultures” to characterize how “shared beliefs about disease aetiology, ideas about the potency and efficacy of modern medicine and views on the need for preventive measures” as well as “local health services experiences and vaccination settings” influence the individual decision about vaccination…vaccine hesitancy may be a consequence of the focus of health promotion on lifestyle and individual action and the growth of “consumerism” in health-care, which means patients’ involvement in their own health decisions. (p. 1765)
An example of understanding context is illustrated in the case of Gawande (2004 as cited in Patton, 2015), who described vaccine hesitance among Muslim mothers to vaccinate their children against polio. Although polio is a deadly, yet preventable illness with a well-developed vaccine, mothers in these communities were vaccine resistant because of their concern about a plot they had learned about in their community to use vaccinations to render their boys sterile. Although these were individual decisions, the mothers had been subjected to marginalization and discrimination, which generated understandable fear, given the sociopolitical context in which they lived. Understanding context in vaccination decisions is important.
Understanding the resistance to vaccination nor other health practices, and developing approaches to overcome that resistance, requires and in-depth understanding of the cultural, social, and political systems within a particular context. (Patton, 2015, p. 9)
In summary, the social, political, and sociocultural considerations are varied and complex. As illustrated in Figure 2, both the equity of actions and trust are significant factors influencing the magnitude of each contributor to vaccine decisions. The historical and current climate may affect the decisions of people with I/DD, as do their perceptions of the vaccine, government-issued interventions, and trust of health care professionals. A person’s own moral and religious convictions, as well as that of their family, community, and culture may also influence their decision-making. Finally, while some PWD might perceive the vaccine as important, this may look different for people with I/DD or people experiencing intersectionality with other historically marginalized identities and lived experiences, such as people of color with I/DD. People with I/DD and their communities’ trust of authority may be constrained because of historical and current practices.
Healthcare Barriers and Healthcare Professionals Decision-Making
As mentioned in the literature, studies have described the prioritization of health care professionals and direct care professionals for receiving the vaccine in the initial phases. However, as studies have noted, the dissemination pathway from the states to providers, to the population at large has been a complex and convoluted one. These have affected individual’s decision-making due to persisting systemic health care barriers which include service providers decisions, their communication, knowledge and perceptions about the vaccine, and their lack of prioritization and training to support the needs of PWD. We expand the concept of healthcare providers for people with I/DD beyond physicians and nurses, to include DSPs, home health and care attendants, mental health support personnel, and those providing recreational and therapeutic care (Ocasio-Stoutenburg et al., 2023).
Persisting health care barriers have been cited in the literature as a major cause of concern that affected individual’s comfort level with the COVID-19 vaccine (CDC, 2021; NCD, 2021). As stated PWD have already been existing health care disparities, which are even greater for persons with I/DD (NCD, 2021). Such disparities included inadequate COVID-19-related healthcare, including low prioritization for hospitalization stays and life-saving treatments, a significant reduction in the number of DSPs to provide continuous care during the pandemic, and few to no alternatives to congregate living, which exacerbated disease transmission and death (NCD, 2021).
Note. Adapted from Dubé et al. (2013).
Similarly, some systemic reasons contributing to vaccine hesitancy among Black and Hispanic or Latino/a/x communities have been the devastation and loss in their communities during the pandemic and the existing gaps in health care coverage and services (Jimenez et al., 2021; Momplaisir et al., 2021). Participants in a qualitative study by Momplaisir et al., of whom 89% identified as Black, reported the inflated cost of insurance, disparate health care coverage, as well as already having the COVID-19 virus as reasons for their vaccine hesitancy.
Within our communities of practice, perspectives were shared by PWD about the challenges of the shift to telehealth, which had both reduced the quality and number of healthcare visits for many. Thus, the state’s initial requirement for a doctor’s note in order to receive the vaccine in the initial phase presented significant barriers and delays for many PWD. One contributing reason was how provider training and knowledge about disability continues to be a gap in healthcare delivery service for PWD, which existed prior to the pandemic and magnified throughout.
Perceptions about the vaccine may have been varied among healthcare professionals and DSPs alike. Reports indicated that PWD often rely on the expertise of healthcare professionals, who may or may not have had positive opinions about the COVID-19 vaccine. This situation is even more connected to provider perspectives and decisions about their own vaccination for people with I/DD. While they often rely on their DSPs for decision making, the DSP’s may often be hesitant about receiving the vaccine and hold an unvaccinated status, thereby increasing the risk for people with I/DD (Ryerson et al, 2021; Unroe et al., 2021).
Dubé et al. (2013) described the patient-provider interaction as the “cornerstone” for generating and sustaining vaccine confidence. These researchers highlighted the role of healthcare professionals’ own confidence regarding their concerns about their patients’ responses to vaccination, noting how “vaccine confidence can induce strong emotional responses in health professionals leading to worries that trust in the relationship with patients can be endangered” (p. 1767). Healthcare providers may also be subjected to a number of external pressures, which include being attentive to the development and timing of the vaccines, while also remaining updated with the schedules and recommendations, which may lead to their reluctance to engage in vaccine-related discussions with patients (Dubé et al., 2013; Kumar et al., 2016). This was particularly complex with the COVID-19 vaccine development, further compounded for PWD (Rodrigues & Plotkin, 2020; Ryerson et al. 2021).
Public Health and Vaccination Policies
Public health has played a significant role in communication with the public at large. Understanding how quickly and widely inaccurate and misleading information about the vaccine and its safety can be disseminated to the public has been a particular challenge for clinicians, public health strategies, providers, policymakers, disability and community organizations, as well patients themselves. Dubé et al. (2013) emphasized how entities communicating public health information should become strategic in tailoring messaging to meet the needs of the population in ways that extend beyond the traditional “knowledge deficit model of communication” as well as using “new tools such as social media and to be proactive rather than reactive to vaccination scares” (p. 1767). Organizations for PWD and key influencers must be properly resourced and leveraged as partners in the roll-out of information campaigns, for instance by reaching out to communities that have experienced the greatest amount of marginalization—people of color with I/DD—while ensuring that messaging is clear, inclusive, and accessible.
Additional research studies on COVID-19 have highlighted the inequity in vaccine distribution as a reason for lower vaccination rates reflected in the data, rather than the community- and individual-level vaccine hesitancy. Underhill and Johnson (2021) described how the pattern of initial distribution followed a trajectory resulting in what public health scholars have referred to as the “inverse equity hypothesis” to emphasize the inequities that impact some groups disproportionately. This framing considers how the resources and interventions applied through a population approach are typically taken up by the members of the population for whom it is most accessible, to the detriment of historically disenfranchised populations. Similar to the concerns addressed in the NCD (2021) annual report, these scholars emphasized how the universal vaccination efforts followed this pattern by failing to consider equity, which had the consequence of furthering the inequities experienced by communities who were already experiencing COVID-19 transmission and mortality to a greater degree (Underhill & Johnson, 2020). This provides some perspective for understanding how PWD, especially persons with I/DD, communities of color, and people of color with I/DD continue to experience disparate access to the very strategies designed to minimize these outcomes (NCD, 2021; NIMHD, 2022). As Underhill and Johnson explain, the “progress of vaccination in the United States has been complex, with heterogeneous state distribution programs prioritizing equity, including racial equity, differently” (2021, p. 55). Similarly, the 2021 report by the NCD highlighted the discriminatory underpinnings of the policies and practices having disproportionate impacts on people with I/DD, noting,
The pandemic also exposed extreme disability bias, failures in modifying policies to accommodate the needs of people with disabilities, and gaps in disability data collection and antidiscrimination laws that need to be rectified before the next pandemic or public health emergency. (NCD, 2021, p. 1)
Communication and Media
Accurate and timely information, as well as responsiveness are critical, especially in a public health crisis where communication plays an essential role. While several studies that have reported on vaccine hesitancy in the Black community, several studies have also described Black communities as information-seeking through news and media outlets, highly engaged in discussion about COVID-19, and more proactive in COVID-19 mitigation efforts, which include masking, as compared with their White counterparts (Jimenez et al., 2021; Mitchell & Jurkowitz, 2020).
Media has also played a significant role in shaping perceptions about vaccination. While media outlets can be used as a channel for providing evidence of the safety and effectiveness of vaccines, it has also provided an opportunity for anti-vaccination activists and organizations to disseminate contradictory messaging. It is prudent to consider that both types of messaging can influence vaccine decision-making, especially through preferred and accessible channels, which may be news or social media platforms.
Receiving conflicting information has been consistently reported across our communities of practice, who have discussed hearing varied reports about the safety of the vaccine. Many PWD and their families in our local communities have access to a number of outlets as sources of information, which include traditional media sources, such as news and radio, as well as social media sites. Community coalition members also shared how residents are often trustful of local clergy and community group chats for the updated COVID-19 vaccine information. In our national UCEDD communities of practice, partners emphasized the value of one-on-one conversations to discuss the vaccine to minimize the barriers in communication between people and medical or institutional personnel and to foster trust. Specific outreach needs to be conducted to ensure that persons with disabilities know of the availability of vaccinations, and all information campaigns are inclusive and accessible to PWD, while also presented in ways that are responsive to age, context, and culture.
Decision-Making About the Vaccine: An Autonomy Continuum
Review of the literature, as well as our community and interprofessional engagements, uncovered several factors contributing to the layers of complexity concerning COVID-19 vaccine decision-making. One contributing factor is that vaccination against COVID-19 is both a public and personal health enterprise. While health and safety protections rely upon individual decision-making, the cumulative health decisions of individuals have an impact on the health of the entire population. Thus, population health strategies have been implemented in an attempt to reduce transmission while also recognizing the disparities for communities (Wrigley-Field et al., 2021). However, as Underhill and Johnson (2021) emphasized, applying universalist approaches across patterns of inequity have led to disparities in access and magnified the preexisting disparities in health outcomes and healthcare, especially for people with I/DD.
Even though vaccination may be considered a personal decision, adding another layer of complexity to vaccine decision-making is the fact that individuals with I/DD may or may not have full autonomy over their healthcare decisions. Many rely on family members, caregivers, or DSPs (Ryerson et al., 2021). Nearly 1 in 5 persons with I/DD reside in congregate settings, where DSPs and other staff may influence decision-making (Larson et al., 2020). Still, there are systemic, institutional, and political decisions that impact their access to care, as well as how care is delivered. Therefore, although it is important to centralize the autonomy of the individual with I/DD over their vaccination decisions, this may involve several other influential persons and entities in their lives, including the DSPs (Iadorola et al., 2022). As illustrated in Figure 2, the supported decision making for people with I/DD exists along a continuum, with more or less support from people within the individual’s support circles (e.g., family members, healthcare professionals, and DSPs). Furthermore, the confidence in vaccine decision-making among people with I/DD also resides along a continuum, ranging from full rejection toward acceptance (Kumar et al., 2016). The dashed border around this central concept underscores the confluence of the multiple external factors, which are mediated through equity and trust, in a bidirectional fashion.
Discussion
As evidenced in the adapted vaccine model, perceptions about vaccines are varied and complex. Considering the systemic inequities that preceded and were magnified by the pandemic, concerns about the vaccine among PWD, and especially people with I/DD and people of color with I/DD, our team sought to develop a comprehensive conceptual model which would (a) incorporate insights from the literature and (b) contribute community, family, and interprofessional perspectives. The contributions, process, and resultant model in Figure 1 highlight the consistent and inextricable roles of both equity and trust, significant mediators throughout the decision-making process.
The growing interest in vaccination as a public health response has resulted in the development of different tools and strategies to enhance vaccination confidence while considering the factors that compromise vaccine accessibility. Many experts have responded to public concerns, proposing ways to counter vaccine hesitancy at the population level, including attempts to improve transparency and communication to the public on policy-level decisions regarding vaccination programs, providing education, disseminating information to the public and health providers about the rigorous process leading to approval of new vaccines, and diversified post-marketing surveillance of vaccine-related events. However, the consideration of vaccine equity, which should be central, has historically been left out of the policy decisions, failing to address already existing disparities and concerns, and perpetuating new ones. In the most recent revisions of strategic planning across large funding entities, equity has become a top priority for developing COVID-19 vaccine and other policies. It should be noted, however, that this has only begun to scratch the surface of a long history of healthcare inequity that has disproportionately impacted generations of populations (Braveman & Gruskin, 2003; Underhill & Johnson, 2021).
Numerous barriers to vaccination have been identified through our efforts, which are at the individual and institutional level. At the individual level, hesitation can result from the concern about side effects; beliefs regarding the efficacy, safety, and usefulness of vaccines; and conflicting messaging about the safety of the vaccines. In addition, there are social and historical barriers that influence individual decisions, which include mistrust of the motives behind the vaccine, historical and current mistrust of providers, medical institutions, and systemic inequities that communities continue to experience. With a history of discrimination and maltreatment of PWD as well as PWD who are at the intersection of historically marginalized racial and ethnic groups, such as Black, Hispanic or Latino/a/x/e, and Native populations, the concerns are heightened. Barriers experienced may be both explicit and nuanced, individual, and systemic. For example, the requirement of a healthcare provider’s recommendation to be vaccinated in the initial phase of vaccination rollout presented significant barriers for individuals without a primary healthcare provider. In addition, the person is then reliant upon the providers’ evaluation to determine whether their disability needs qualify them as a priority for the vaccine. This in itself may introduce barriers because of the gaps in training on the priority and needs of PWD.
Healthcare professionals and DSP may also have significant concerns about the vaccine’s safety and usefulness themselves. As these individuals are in a role where they are both influential on an individual and community level, this has an impact on vaccine outcomes. Healthcare and DSP are also situated within a complex array of political, social, economic, and cultural influences. On another level, the attitudes among health care professionals who operate within systems and networks can either facilitate or impede vaccine access. Certainly, viewing the healthcare risks for COVID-19 in PWD can lead to the prioritization of vaccine access for this population. However, it may also lead individuals to consider this as specialty care rather than standard care.
Conclusion
Taken together, the perceptions among individuals with I/DD, their families, communities, healthcare providers, DSP, agencies, and systems introduce barriers to vaccination. These barriers are often presented as discrete and measurable variables, without regard to the “processes and pathways” leading to vaccination refusal as well as to the broader sociocultural context within which these barriers are rooted. As mentioned, many well-intended efforts may fail to consider equity and trust throughout the interventions. As Braveman and Gruskin (2003) noted, promoting health care equity is removing the policies and practices that may disproportionately impact many people’s lives.
Serious concerns have been raised about how PWD, especially people with I/DD, and people of color with I/DD, access vaccinations. Self-advocates continue to put forth legitimate questions about the prioritization of PWD and their support networks for vaccinations. Other concerning areas are accessibility of vaccination processes, related information and venues, and provision of vaccines based on free and informed consent of all PWD. This raises questions about the gatekeeping in healthcare policy under the ADA and Section 504 for reasonable accommodations. Furthermore, the dissemination and accessibility concerns underscore the underlying bioethical considerations. Who becomes a priority in a healthcare emergency? Certainly, the development of a conceptual model endeavored to consider equity and to incorporate access barriers as well as the concerns of PWD, especially people with I/DD, communities of color, and people of color with I/DD. As our lives and healthcare needs become more complex, so does our need for interdependence. Trust is an essential factor in people feeling secure in their care and that their needs will be met. Thus, our efforts at addressing the needs of our most vulnerable populations should take precedence, by incorporating their needs and preferences into our policy development, with equity as a guidepost. We offer this adapted conceptual model for building vaccine confidence provides as a framework to better understand, respond, and develop strategies to minimize barriers and promote healthcare equity for persons with I/DD.
References
Adamu, A. A., Jalo, R. I., Habonimana, D., & Wiysonge, C. S. (2020). COVID-19 and routine childhood immunization in Africa: Leveraging systems thinking and implementation science to improve immunization system performance. International Journal of Infectious Diseases, 98, 161–165. https://doi.org/10.1016/j.ijid.2020.06.072
Americans With Disabilities Act of 1990, 42 USC § 12101 et seq. (1990). https://www.ada.gov/pubs/ adastatute08.htm
Administration for Community Living (ACL). (2021, March 29). Partnership with CDC to increase access to COVID-19 vaccines. https://acl.gov/news-and-events/announcements/partnership-cdc-increase-access-covid-19-vaccines
Braveman, P., & Gruskin, S. (2003). Defining equity in health. Journal of Epidemiology & Community Health, 57(4), 254-258.
Centers for Disease Control and Prevention. (2022). COVID data tracker. https://covid.cdc.gov/covid-data-tracker
Chakraborty, J. (2021). Social inequities in the distribution of COVID-19: An intra-categorical analysis of people with disabilities in the US. Disability and Health Journal, 14(1), 1-5.
Coustasse, A., Kimble, C., & Maxik, K. (2021). COVID-19 and vaccine hesitancy: A challenge the United States must overcome. The Journal of Ambulatory Care Management, 44(1), 71-75.
Crenshaw, K. (1989). Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum, 139.
Davis, A., & Mendez, D. D. (2022). Applications of an equity framework in COVID-19 vaccine trial and distribution planning. Health Equity, 6(1), 55-58.
Dubé, E., Laberge, C., Guay, M., Bramadat, P., Roy, R., & Bettinger, J. A. (2013). Vaccine hesitancy: An overview. Human Vaccines & Immunotherapeutics, 9(8), 1763-1773. https://doi.org/10.4161/ hv.24657
Ehreth, J. (2003). The global value of vaccination. Vaccine, 21(7), 596–600. https://doi.org/10.1016/ S0264-410X(02)00623-0
Gleason, J., Ross, W., Fossi, A., Blonsky, H., Tobias, J., & Stephens, M. (2021). The devastating impact of Covid-19 on individuals with intellectual disabilities in the United States. NEJM Catalyst Innovations in Care Delivery, 2(2), 1-12. https://doi.org/10.1056/CAT.21.0051
Goode, T. A (2019). Resource guide to respond to disparities in intellectual and developmental disabilities: Services and supports. Washington, DC: Georgetown University National Center for Cultural Competence, Center for Child and Human Development.
Iadarola, S., Siegel, J. F., Gao, Q., McGrath, K., & Bonuck, K. A. (2022). COVID-19 vaccine perceptions in New York State’s intellectual and developmental disabilities community. Disability and Health Journal, 15(1), 1-8. https://doi.org/10.1016/j.dhjo.2021.101178
Jimenez, M. E., Rivera-Núñez Z, Crabtree, B. F., Hill, D., Pellerano, M. B., Devance, D., Macenat, M., Lima,D. Alcaraz, E. M., Ferrante, J. M., Barrett, E., Blaser, M. J., Panettieri R. A., & Hudson, S. V. (2021). Black and Latinx community perspectives on COVID-19 mitigation behaviors, testing, and vaccines. JAMA Network Open, 4(7), 1-11. https://jamanetwork.com/journals/jamanetwork open/fullarticle/2781957
Kaufman, J., Ames, H., Bosch-Capblanch, X., Cartier, Y., Cliff, J., Glenton, C., Lewin, S., Mulowiwa, A. M., Oku, A., Oyo-Ita, A., Rada, G., & Hill, S. (2017). The comprehensive ‘Communicate to Vaccinate’ taxonomy of communication interventions for childhood vaccination in routine and campaign contexts. BMC Public Health, 17(1), 1-11. https://doi.org/10.1186/s12889-017-4320-x
Khazanchi, R., Evans C. T., & Marcelin J. R. (2020). Racism, not race, drives inequity across the COVID-19 continuum. JAMA Network Open 3(9), e2019933. https://jamanetwork.com/journals/jama networkopen/fullarticle/2770954
Kumar, D., Chandra, R., Mathur, M., Samdariya, S., & Kapoor, N. (2016). Vaccine hesitancy: Understanding better to address better. Israel Journal of Health Policy Research, 5(1), 1-8.
Landes, S. D., Turk, M. A., & Wong, A. W. (2021). COVID-19 outcomes among people with intellectual and developmental disability in California: The importance of type of residence and skilled nursing care needs. Disability Health Journal. 14(2), 1-5. https://pubmed.ncbi.nlm.nih.gov/33309535/
Larson, S. A., Eschenbacher, H. J., Taylor, B., Pettingell, S., Sowers, M., & Bourne, M. L. (2020). In-home and residential long-term supports and services for persons with intellectual or developmental disabilities: Status and trends through 2017. Minneapolis: University of Minnesota, Research and Training Center on Community Living, Institute on Community Integration.
Mahmud, S. M., Xu, L., Hall, L. L., Puckrein, G., Thommes, E., Loiacono, M. M., & Chit, A. (2021). Effect of race and ethnicity on influenza vaccine uptake among older US Medicare beneficiaries: A record-linkage cohort study. The Lancet Healthy Longevity, 2(3), e143-e153.
Mitchell, A., & Jurkowitz, M. (2020). Black U.S. adults follow many COVID-19 news topics more closely, discuss the outbreak more frequently. https://policycommons.net/artifacts/616406/black-us/ 1597056/
Momplaisir, F., Haynes, N., Nkwihoreze, H., Nelson, M., Werner, R. M., & Jemmott, J. (2021). Understanding drivers of coronavirus disease 2019 vaccine hesitancy among Blacks. Clinical Infectious Diseases, 73(10), 1784-1789.
National Council on Disability. (2021). The impact of COVID-19 on people with disabilities. https://ncd.gov/ progressreport/2021/2021-progress-report
National Institute of Minority Health and Health Disparities. (2022). COVID-19 Information and Resources. https://www.nimhd.nih.gov/programs/covid-19/
Ndugga, N., Hill, L., Artiga, S., & Haldar S. (2022). Latest data on COVID-19 vaccinations race/ethnicity. Kaiser Family Foundation. https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-by-race-ethnicity/
Ocasio-Stoutenburg, L, Hernandez, J., & Jackson, D. J. (2023) Beyond representation: Partnerships, intersectionality, and the centering of the disability, family, and community lived experience. Developmental Disabilities Network Journal, 3(1), 105-131. https://digitalcommons.usu.edu/ ddnj/vol3/iss1/10
Ozawa, S., Paina, L., & Qiu, M. (2016). Exploring pathways for building trust in vaccination and strengthening health system resilience. BMC Health Services Research, 16 (Suppl 7), 132-141. https://doi.org/10.1186/s12913-016-1867-7
Painter, E. M., Ussery, E. N., Patel, A., Hughes, M. M., Zell, E. R., Moulia, D. L., Scharf, L. G., Lynch, M., Ritchey, M. D., Toblin, R. L., Murthy, B. P., Harris, L. Q., Wasley, A., Rose, D. A., Cohn, A., & Messonnier, N. E. (2021). Demographic characteristics of persons vaccinated during the first month of the COVID-19 vaccination program — United States, December 14, 2020–January 14, 2021. Morbidity and Mortality Weekly Report, 70(5), 174–177. https://www.cdc.gov/mmwr/ volumes/70/wr/mm7039a2.htm?s_cid=mm7039a2_w
Patton, M. Q. (2014). Qualitative research & evaluation methods: Integrating theory and practice. SAGE publications.
Rodrigues, C., & Plotkin, S. A. (2020). Impact of vaccines: Health, economic and social perspectives. Frontiers in Microbiology, 11, 1526. https://doi.org/10.3389/fmicb.2020.01526
Ryerson, A. B., Rice, C. E., Hung, M. C., Patel, S. A., Weeks, J. D., Kriss, J. L., Peacock, G., Lu, P. J., Asif, A. F., Jackson, H. L., & Singleton, J. A. (2021). Disparities in COVID-19 vaccination status, intent, and perceived access for noninstitutionalized adults, by disability status – national immunization survey adult COVID module, United States, May 30-June 26, 2021. Morbidity and Mortality Weekly Report, 70(39), 1365–1371. https://doi.org/10.15585/mmwr.mm7039a2
Underhill, K., & Johnson, O. C. (2021). Vaccination equity by design. Yale Law Journal Forum, 131, 53-88.
Unroe, K. T., Evans, R., Weaver, L., Rusyniak, D., & Blackburn, J. (2021). Willingness of long-term care staff to receive a COVID-19 vaccine: A single state survey. Journal of the American Geriatrics Society, 69(3), 593–599. https://doi.org/10.1111/jgs.17022
World Health Organization. (2020, March 11). WHO Director-General’s opening remarks at the media briefing on COVID-19. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020
Wrigley-Field, E., Kiang, M. V., Riley, A. R., Barbieri, M., Chen, Y. H., Duchowny, K. A., Matthay, E.C., Van Riper, D., Jegathesan, K., Bibbins-Domingo, K., & Leider, J. P. (2021). Geographically targeted COVID-19 vaccination is more equitable and averts more deaths than age-based thresholds alone. Science Advances, 7(40), 1-14. https://doi.org/10.1126/sciadv.abj2099

