Uterine Cycle
Objective 7
Describe the histology, blood supply, and cycle of the uterine wall.
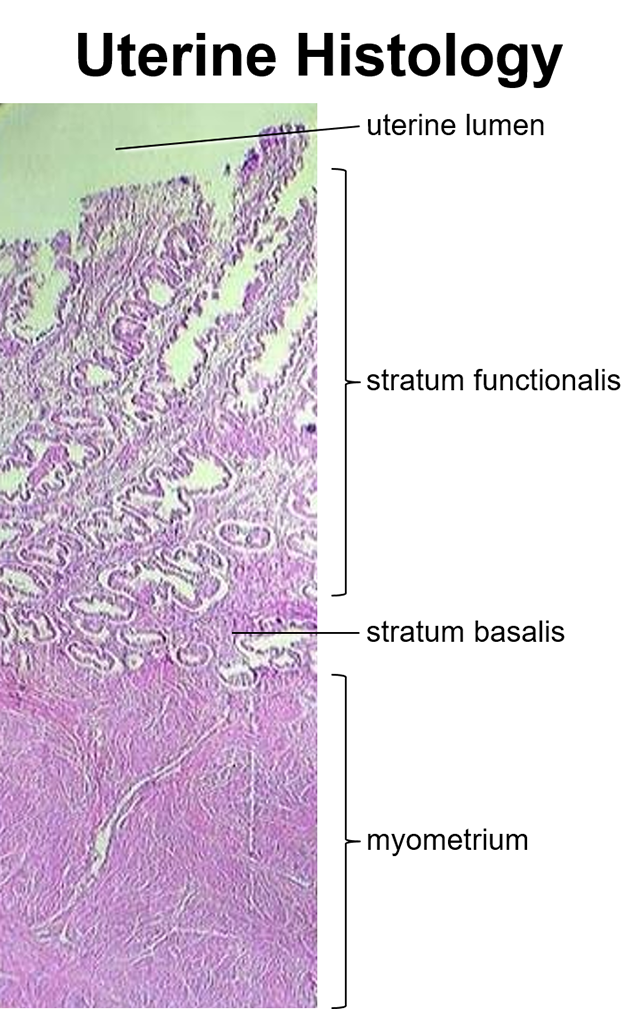
Uterine Histology
 The uterine layers are easy to remember once we puzzle out the word origins. Each of them contains the Greek root μεηπα, (pronounced “metra”), which means “womb” and is closely related to the Latin mater, or “mother.”
The uterine layers are easy to remember once we puzzle out the word origins. Each of them contains the Greek root μεηπα, (pronounced “metra”), which means “womb” and is closely related to the Latin mater, or “mother.”
The inner lining of the womb, then, is called the endometrium; the muscular layer is called the myometrium, and the outer layer (nearest the pelvic cavity) is the perimetrium.
Note that more than 90% of the thickness of the uterine wall is the myometrium, which consists of three layers of smooth muscle. These muscle layers become very important during childbirth.
Remember serous membranes? (Thin, two-layered membranes that secrete small amounts of serous fluid between the layers? Visceral layer and parietal layer? Think pleura, pericardium, and peritoneum.) The perimetrium is the uterine portion of the visceral peritoneum.
The endometrium consists of three layers (beginning with the luminal surface): 1) a layer of simple columnar epithelium, 2) the stratum functionalis (functional layer), and 3) the stratum basalis (basal layer). The epithelium and stratum functionalis are shed during each menstrual cycle, resulting in menstrual flow.
Also note that the uterus has a rich blood supply. Blood flows from the internal iliac arteries into the uterine arteries, then into the arcuate arteries and radial arteries. The radial arteries branch into straight arterioles, which nourish the stratum basalis, and spiral arterioles, which nourish the stratum functionalis and are shed along with the stratum functionalis.
The uterus’ venous drainage is into the uterine veins and then into the internal iliac veins.
The Uterine Cycle
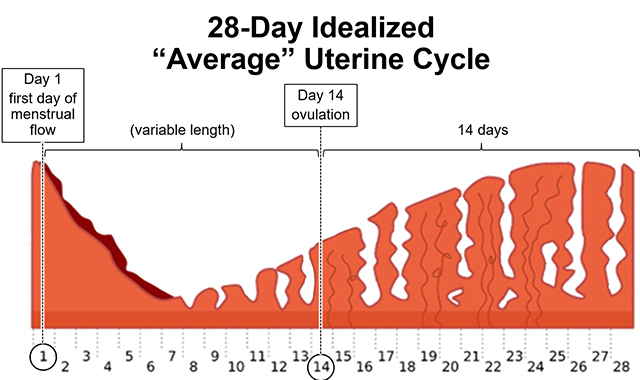
The “average” uterine (menstrual) cycle is 28 days. From this point on, we will base our discussion of the female cycle on this idealized average. As reference points, the first day of menstrual flow is Day 1 and ovulation occurs on Day 14. As many (most?) women might not experience a 28-day cycle, it is important to note that the variation in cycle length occurs between the end of menstrual flow and ovulation. The time from ovulation to the beginning of the next cycle tends to be very consistent — 14 days. More on this later.
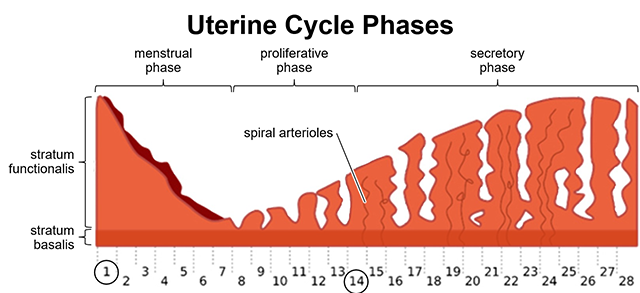
During the menstrual phase of the uterine cycle, the stratum functionalis and its associated blood vessels (spiral arterioles and venules) are lost. After the end of menstrual flow (Day 7 in the idealized timeline), the proliferative phase begins in which the spiral arterioles (and associated venules) are rebuilt to provide nourishment for the regenerating (proliferating) stratum functionalis.
After ovulation (ideally at Day 14), the endometrium enters a secretory phase and the venules and spiral arterioles continue to enlarge; this is in preparation for the implantation of the embryo. If the embryo does implant in the uterine lining, it will occur about Day 21 and will need a rich blood supply in order to build a placenta and feed the embryo. If implantation does not occur, at around Day 26 the endometrial lining will prepare for the next menstrual phase.
Notice that, while the stratum functionalis undergoes major changes during the menstrual cycle, the stratum basalis (darker shading at bottom of diagram) is basically unchanged throughout.
The amount of menstrual flow varies widely. The average is about 36 ml per cycle; more than 80 ml is considered menorrhagia, or abnormal menstrual bleeding. The number of tampons or pads used, while a common question in the clinical setting, is not well correlated with menstrual flow because it is highly dependent on a woman’s preference for tampon/pad change frequency (which tends to be highly variable from one woman to another).
Media Attributions
- U20-034 Endometrium © Nasimudeen, Roshan Dr. adapted by Brad Winterton is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-035 Endometrium Diagram 1 © Speck-Made adapted by Brad Winterton is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-036 Endometrium Diagram 2 © Speck-Made adapted by Brad Winterton is licensed under a CC BY-SA (Attribution ShareAlike) license

