Tubular Reabsorption and Secretion
Objective 5
Compare and contrast glomerular reabsorption and secretion. Describe cells in the proximal convoluted tubule that allow for reabsorption. Explain the concept of transport maximum in tubular reabsorption of substances, particularly glucose. List the approximate amount of reabsorption that occurs of substances that pass through the glomerulus. Describe two mechanisms by which water is reabsorbed. Describe tubular secretion and list substances secreted into the urine. Discuss the effects of the renin-angiotensin-aldosterone system, and ADH on reabsorption.
Remember that 180 L of filtrate is formed in 24 hours, yet the net urine output is 1-2 L. It isn’t hard to understand that the body can’t afford to lose 180 L of fluid/day, so once filtrate is formed, something must be done to keep the fluid volume and vital nutrients but allow excretion of wastes. Glomerular filtration is not selective. This means that anything small enough will pass through the glomerular filtration membrane. The body would like to keep most of what passes. Have you ever had a parent, roommate, or significant other clean out your closet? You come home to bags and bags of potential charitable contributions. A lot of what is being given away you would like back, and so you start going through the bags, reclaiming that which is rightfully yours. This is much like your kidneys. Our bodies need most of the water that passes through the glomerulus, the sodium, glucose, and so forth. In fact, 99% of what passes through the glomerulus must be returned to the blood. The process of reclaiming these substances is called reabsorption.
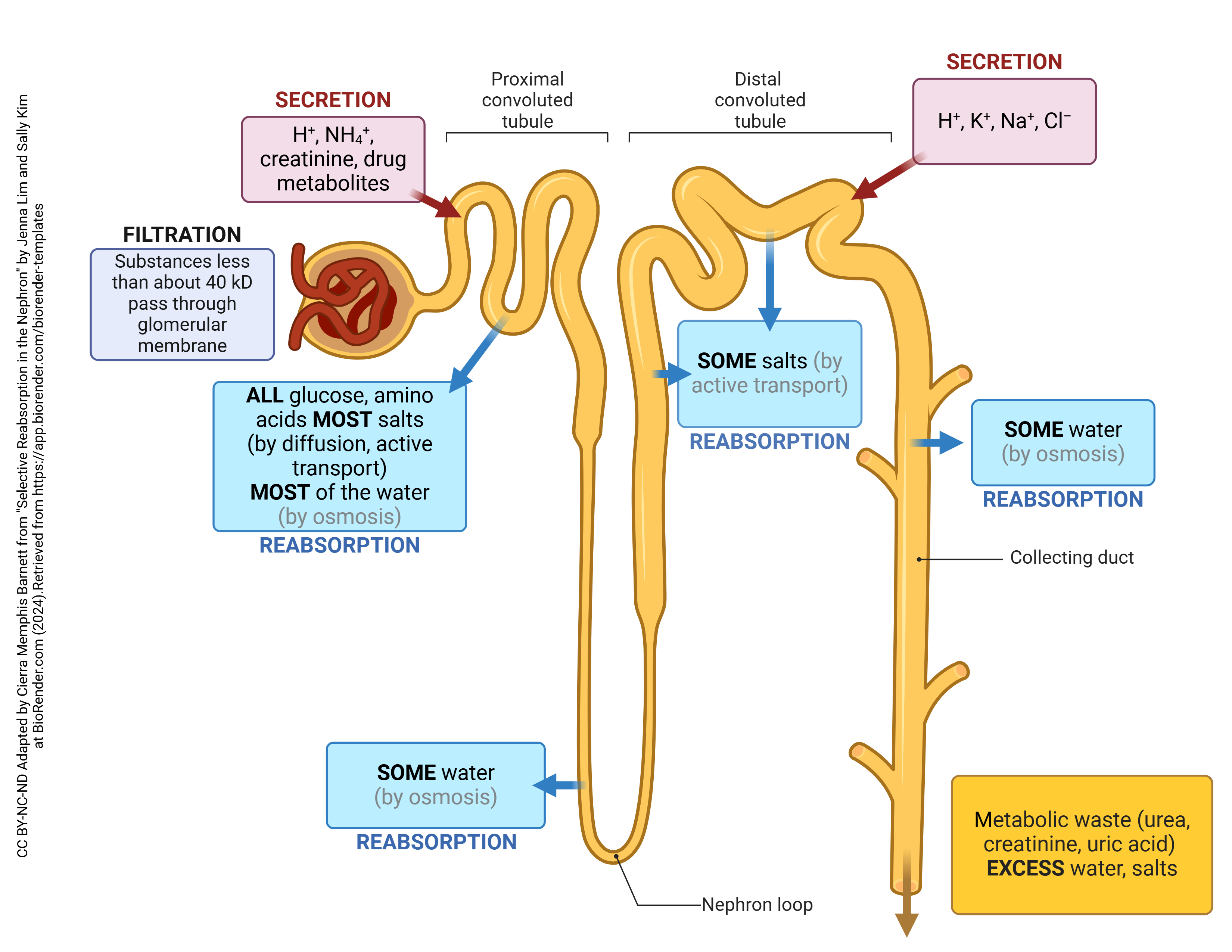
A host of transport mechanisms are utilized to facilitate this massive reabsorption: osmosis, active transport, diffusion, and facilitated diffusion. The majority of solutes and water reabsorption occurs in the proximal convoluted tubule: 65% of the water, sodium and potassium, 100% of the glucose and amino acids, and 50% of the urea. To maximize reabsorption capacity, cells of the proximal convoluted tubule are cuboidal epithelium with prominent microvilli.
Transport proteins are present on the surfaces of cells to actively reabsorb many of the solutes. Each type of transporter has a limit to how fast it can reabsorb a particular solute. This upper limit is called the transport maximum (Tm). If the level of a solute exceeds the transport maximum, the excess will be excreted into the urine.
Individuals with diabetes who do not keep their blood glucose level under 200 mg/dL can exceed the renal transport maximum for glucose. This will result in the loss of glucose into the urine, a condition called glucosuria.
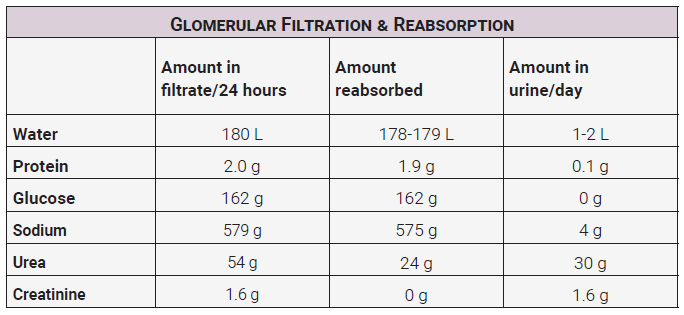
Notice from this table that most of the small proteins that pass through the glomerulus get reabsorbed. One hundred percent of the glucose should be reabsorbed. This means that any amount of glucose in the urine is abnormal. Most of the sodium is reabsorbed. About half of the urea, a waste product from protein breakdown, is reabsorbed. Note that none of the creatinine, a waste product from muscle breakdown, is reabsorbed.
Of the 180 L of water that passes through the glomerulus each day, all but 1-2 L is reabsorbed.
The reabsorption of water is controlled in two different ways:
- Obligatory reabsorption of water occurs as water follows solutes. All of the water reabsorption from the filtrate occurs because of osmosis, so as solutes are reabsorbed, water is “obliged” to follow. Because most of the tubules of the nephron are permeable to water, this can occur almost anywhere, however most water reabsorption takes place in the proximal convoluted tubule. Obligatory reabsorption accounts for 90% of total water reabsorption.
- Facultative reabsorption of water occurs because the body is trying to respond to a specific need. Again, this will occur due to osmosis, but the mechanism is facilitated through the use of antidiuretic hormone (ADH) that acts on cells in the distal convoluted tubule and especially the collecting ducts. Facultative reabsorption accounts for 10% of total water reabsorption.
Tubular secretion is the process of removing a substance from the blood and secreting it into the tubular lumen to be excreted with the urine. This process occurs throughout the nephron. Secreted substances include H+, K+, NH4+, creatinine, and some drugs. The secretion of H+ helps to control the blood pH, and the secretion of other substances helps eliminate wastes.
Effects of Hormones on Tubular Reabsorption
Renin-Angiotensin-Aldosterone System (RAAS)
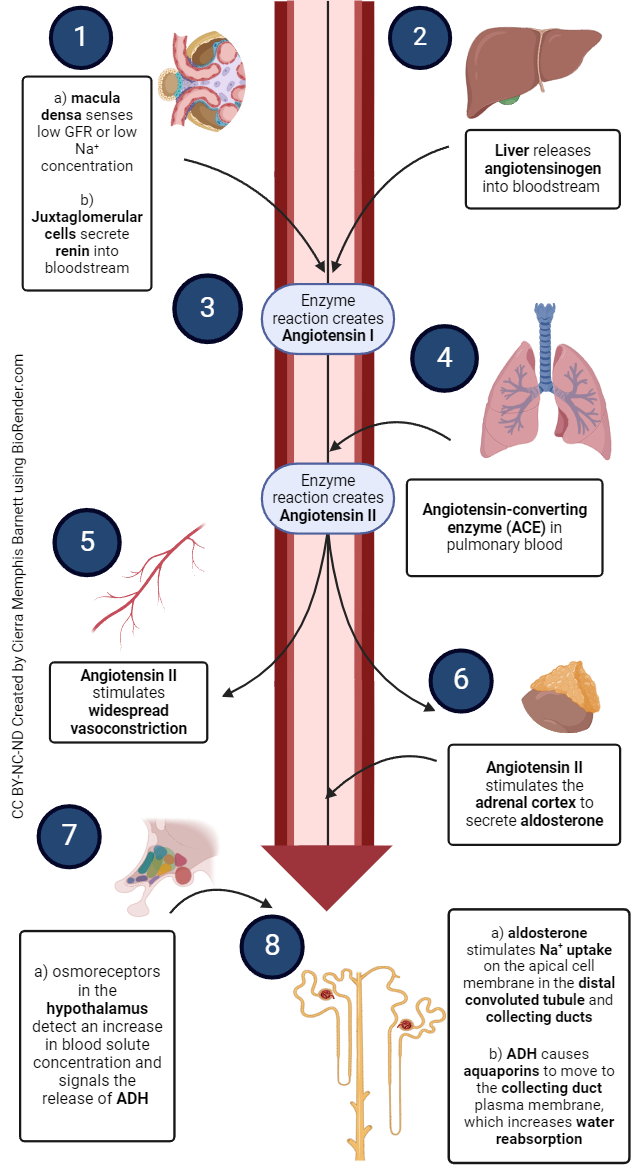
The RAAS was introduced in unit 14. Remember that the goal of this system is to raise blood pressure. Effectors of this system are angiotensin II and aldosterone. A decrease in blood pressure causes decreased pressure in the afferent arterioles.
As a response, juxtaglomerular cells secrete the hormone renin. Renin converts angiotensinogen to angiotensin I. Angiotensin converting enzyme converts angiotensin I to angiotensin II
Angiotensin II causes vasoconstriction, including the afferent arterioles, enhances sodium, chloride, and water reabsorption, and stimulates the adrenal cortex to secrete aldosterone.
Aldosterone signals cells in the collecting ducts to reabsorb more sodium, chloride, and water and secrete more potassium.
Renal Influence of Antidiuretic Hormone (ADH)
Osmoreceptors in the hypothalamus detect an increase in blood solute concentration
The posterior pituitary responds by secreting ADH. ADH stimulates the insertion of water-channel proteins (aquaporin-2) in cells of the collecting duct. In an upcoming objective we’ll learn how the kidney goes to great lengths to establish a concentration gradient in the renal medulla. Under the influence of ADH, water flows by osmosis into the higher concentration of the medulla and then into blood vessels. Conveniently, levels of ADH increase at night when sleeping. Nice so that we don’t have to get up all night and pee!
Media Attributions
- U19-021 Glomerular Filtration and Reabsorption Table © Price, Travis is licensed under a CC BY-SA (Attribution ShareAlike) license
- U19-011 Reabsorption in the Nephron v3 © Cierra Memphis Barnett | BioRender is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U19-022 Effects of Hormones on Tubular Secretion © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license

