The Innate Immune System
Objective 10
Compare the lines of defense associated with innate immunity. Identify the key components of the innate immune system and which ones belong to which line of defense. Describe phagocytosis, fever, and inflammation. Describe the components of the complement system and its role in immunity.
 The chemical and physical barriers of the first line of defense include: skin, mucus, mucus-coated hairs, cilia, the lacrimal apparatus, vaginal secretions, sebaceous secretions, and gastric fluids. It also includes reactions such as vomiting, defecation, salivation, urination, perspiration, coughing, sneezing and blinking. Each of these barriers or responses protects the various external openings of the body.
The chemical and physical barriers of the first line of defense include: skin, mucus, mucus-coated hairs, cilia, the lacrimal apparatus, vaginal secretions, sebaceous secretions, and gastric fluids. It also includes reactions such as vomiting, defecation, salivation, urination, perspiration, coughing, sneezing and blinking. Each of these barriers or responses protects the various external openings of the body.
The second line of defense includes a large number of internal defenses. As part of this line, the body produces natural antimicrobial substances like interferons, complement, and iron-binding proteins to decrease microbial growth.
Non-specific phagocytes and natural killer cells are part of this second line.
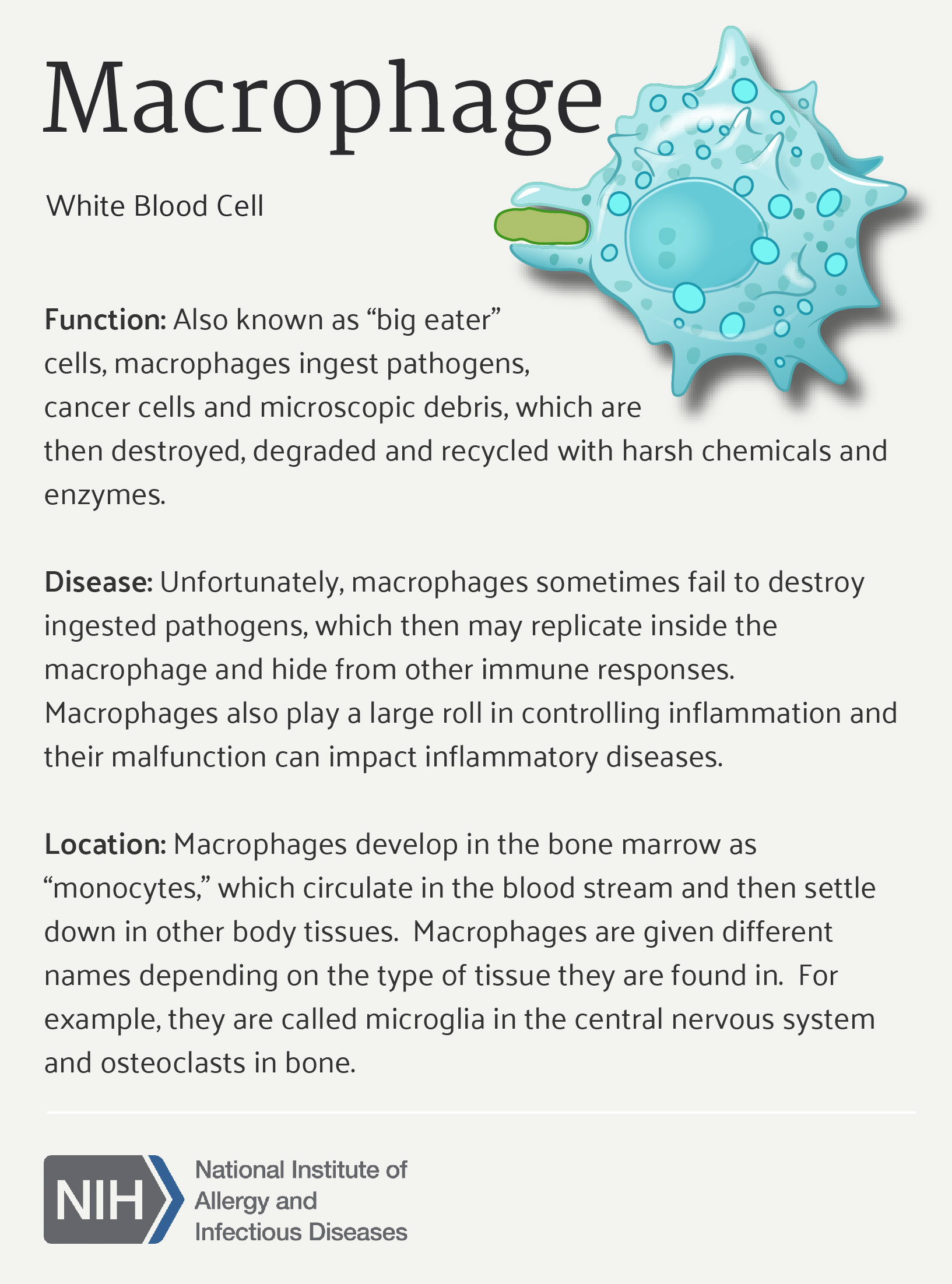
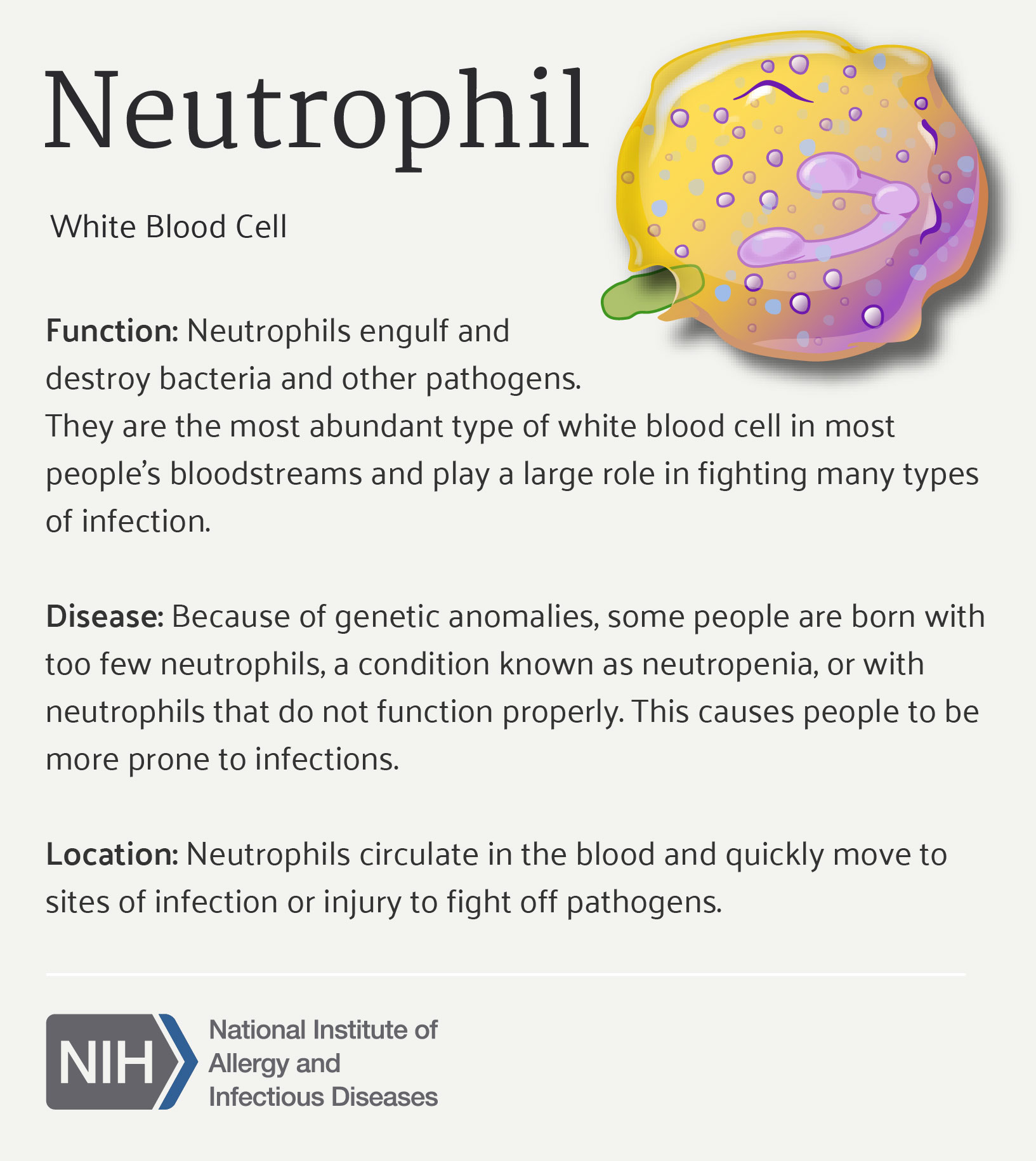 There are two groups of phagocytes in the second line of defense, neutrophils and macrophages. Neutrophils are released in large numbers, very quickly, but their lifespan is relatively short. The bone marrow releases monocytes that enlarge and develop into macrophages as they migrate to the site of infection or injury. These are called wandering macrophages. Other macrophages, called fixed macrophages, may occupy specific tissues and have specific names like Kupffer cells in the liver or microglial cells in the central nervous system.
There are two groups of phagocytes in the second line of defense, neutrophils and macrophages. Neutrophils are released in large numbers, very quickly, but their lifespan is relatively short. The bone marrow releases monocytes that enlarge and develop into macrophages as they migrate to the site of infection or injury. These are called wandering macrophages. Other macrophages, called fixed macrophages, may occupy specific tissues and have specific names like Kupffer cells in the liver or microglial cells in the central nervous system.
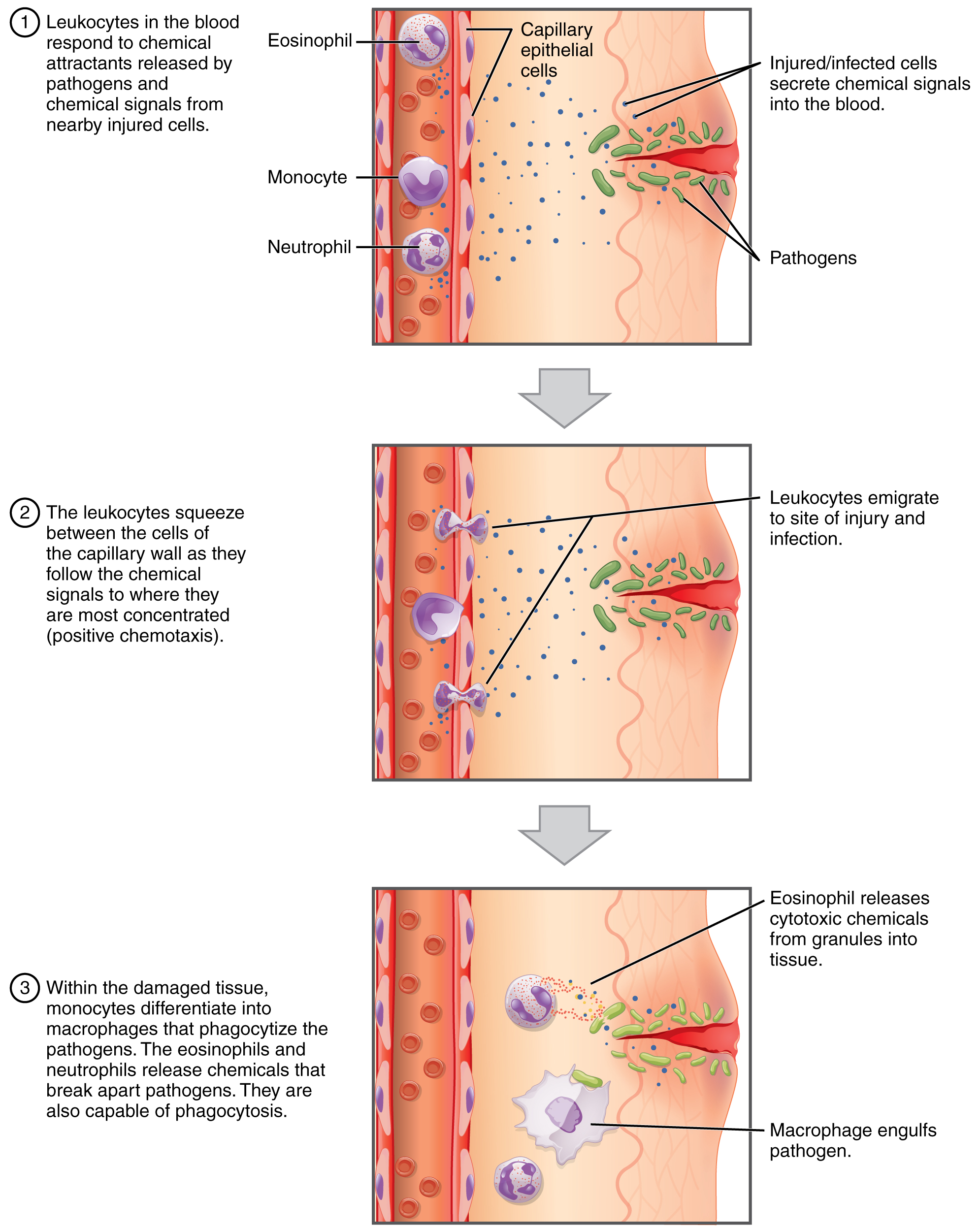
In a similar way, phagocytic cells are attracted to the chemical signals given off by foreign microbes or cells and will move towards them in a process called chemotaxis. Once the membrane of the phagocytic cells comes in contact with the thing to be eaten it will stick to it.
After this adherence, the phagocytic cell will bring the thing in through endocytosis. Digestive enzymes and other chemicals inside phagocytic cells help to break the cell into pieces, effectively digesting and killing it. The final step that a phagocytic cell can perform is to express a piece of the destroyed cell on its surface to alert other immune cells of threat it is responding to. Antigen presentation is an important connection between the innate and adaptive immune responses.
Fever & Inflammation
When the hypothalamus shifts the body’s thermostat to increase temperature, we call it fever. Fever is part of our non-specific internal defenses. Fever is often thought of as a bad thing, and from a patient-comfort point of view, that probably is correct. But, to fight off disease, fever is a good thing. An increase in body temperature speeds up chemical reactions, increases antimicrobial activity, and sequesters (hides) nutrients essential for bacterial growth. Remember those boring chemistry labs in high school? What did you do if you wanted to speed up a reaction? You heated it up!
Inflammation is a big part of our non-specific internal defenses. The process of inflammation has three stages:
- vasodilation and increased vascular permeability,
- emigration of phagocytes from the blood to the tissue, and
- tissue repair.
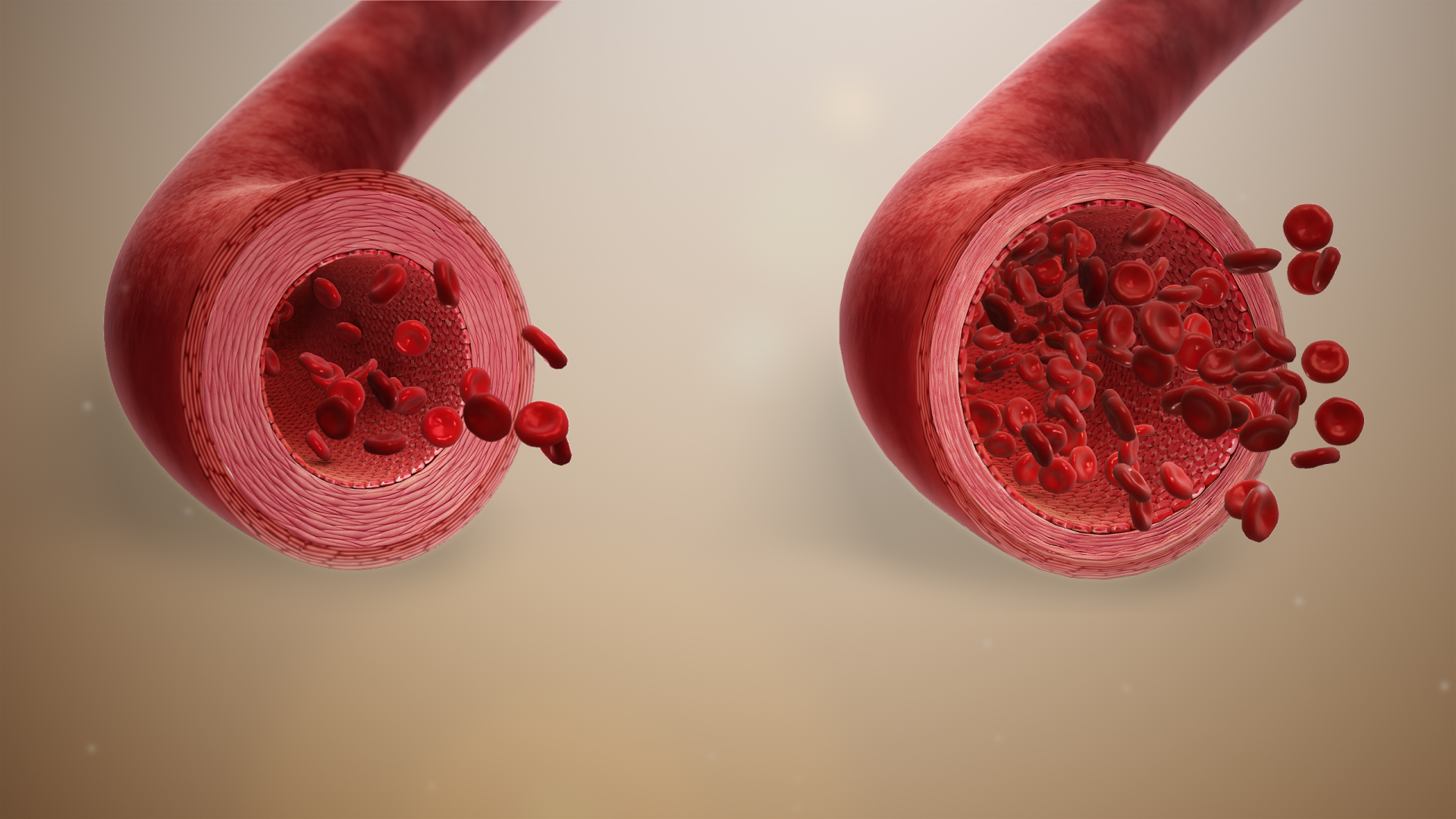
The stimuli that could trigger inflammation include burns, chemical exposure, heat, cold, or trauma. Regardless of why it starts, the inflammatory response is always the same. The local signs of inflammation are easy to recognize: redness, pain, heat, swelling, and possibly loss of function.
 These signs relate to the stages of inflammation. The redness and heat are due to the increased blood flow. The swelling is because of the increased vascular permeability. The cytokines and pro-inflammatory chemicals, released as part of inflammation, target free nerve endings that result in the perception of pain. The loss of tissue function depends on the degree of initial damage and the extent of the inflammation. Too much of a good thing may be bad.
These signs relate to the stages of inflammation. The redness and heat are due to the increased blood flow. The swelling is because of the increased vascular permeability. The cytokines and pro-inflammatory chemicals, released as part of inflammation, target free nerve endings that result in the perception of pain. The loss of tissue function depends on the degree of initial damage and the extent of the inflammation. Too much of a good thing may be bad.
The Complement System
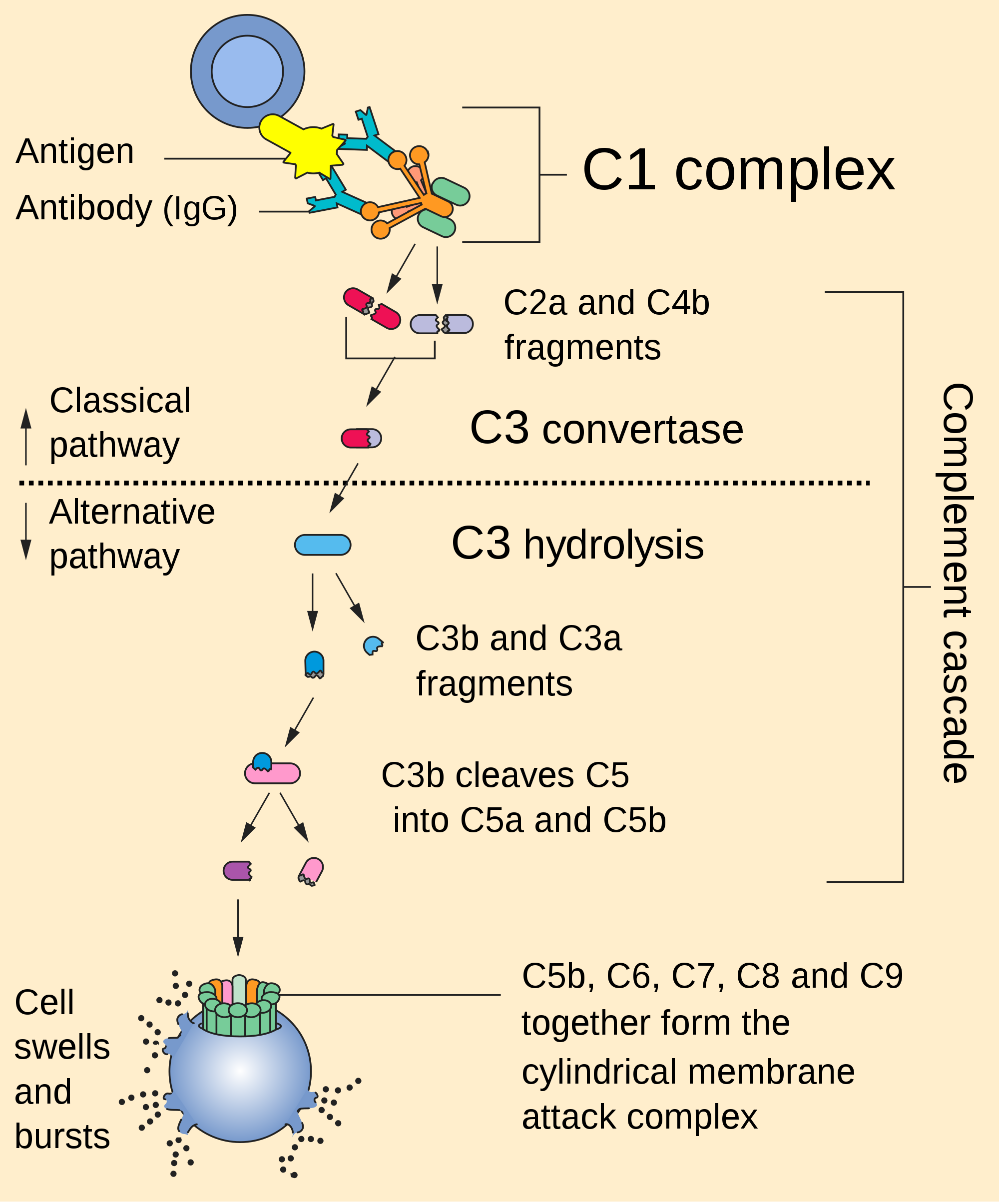
The complement system is a very powerful group of proteins that “complement” the action of the immune system. This system can be compared with the coagulation system in that there are multiple pathways to activate the system and, like clotting, it functions in a stepwise or cascading fashion. Each step results in the fragmentation of one protein that then becomes the activator of the next step.
Complement proteins are made by the liver and are some of the most abundant blood proteins.
The complement system has three divisions:
The classical pathway was the first discovered by scientists. Because it was discovered first, it got the lowest numbers (C1-C3). Complement 1 (C1) is good at bringing together the constant regions (FC regions) of antibody proteins. Because the IgM has five of these, IgM is a really effective activator of the complement system. This pathway is a positive feedback loop, so its effect is powerful.
The alternative pathway involves three more sets of destructive tools.
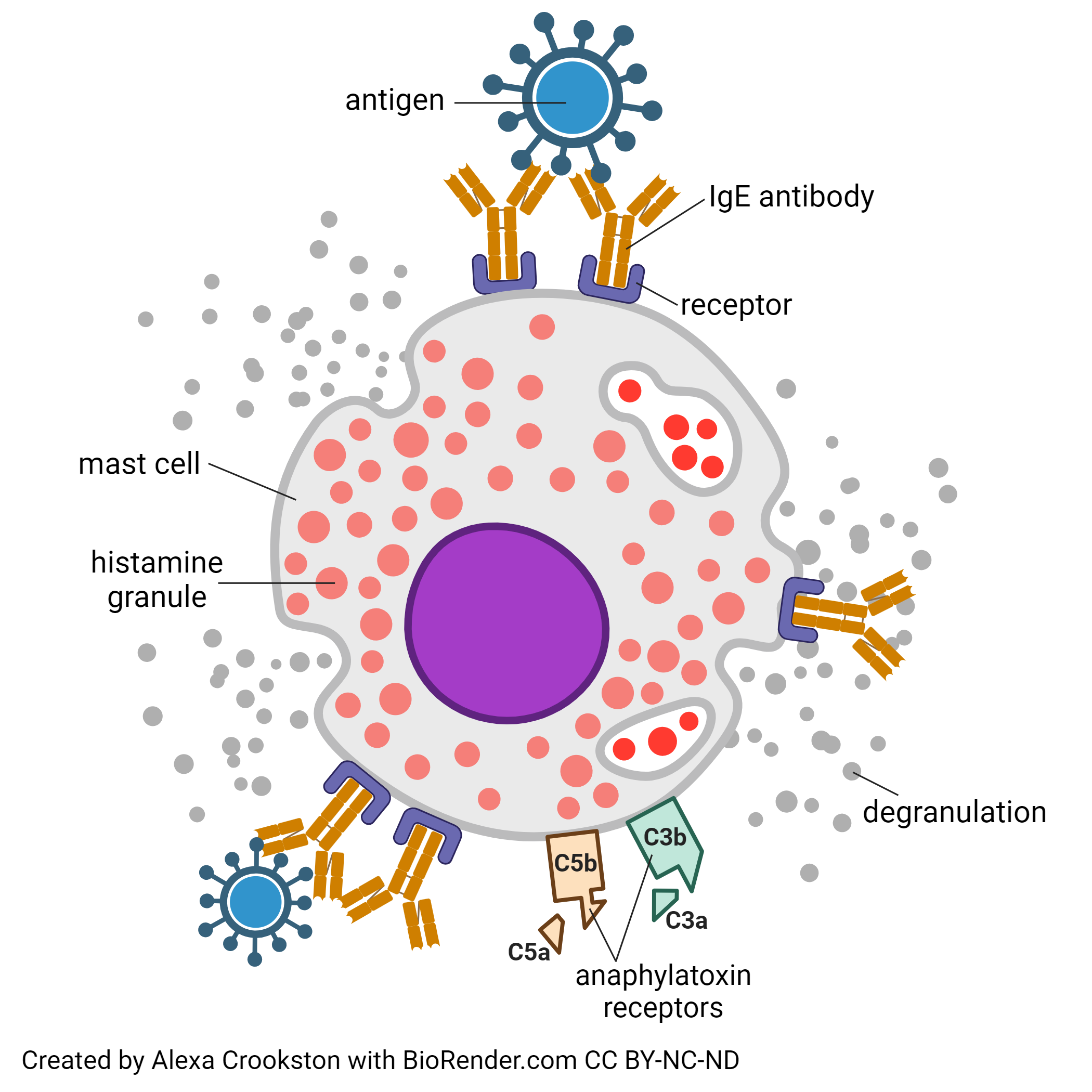
One of the tool sets, if misused, ends up in the destructive reaction known as anaphylaxis (“backward protection”). The allergic and anaphylactic reactions are triggered by a combination of IgE from B lymphocytes with the so-called anaphylatoxins C3a and C5a. When all these things bind to a mast cell, this cell dumps its cargo of inflammatory chemicals stored in membrane-bound granules. The most notable of these inflammatory chemicals is histamine. We take antihistamines to stop these powerful chemicals from reaching their receptors.
The other tool set in the alternative pathway is opsonization. We were introduced to the process of opsonization when we saw the action of antibodies in Objective 9. Another way to imagine this is the laser scope used by warfighters to guide a smart missle to its target by “lighting it up”. Complement C3b “paints the target” and attracts a missle fired hundreds of miles away to an exact location.
The third set of tools in the alternative pathway is formation of a membrane attack complex (MAC) which is a complex of proteins that come together to attack the membrane. When we create a huge hole in the membrane of an invader, his death occurs in short order.
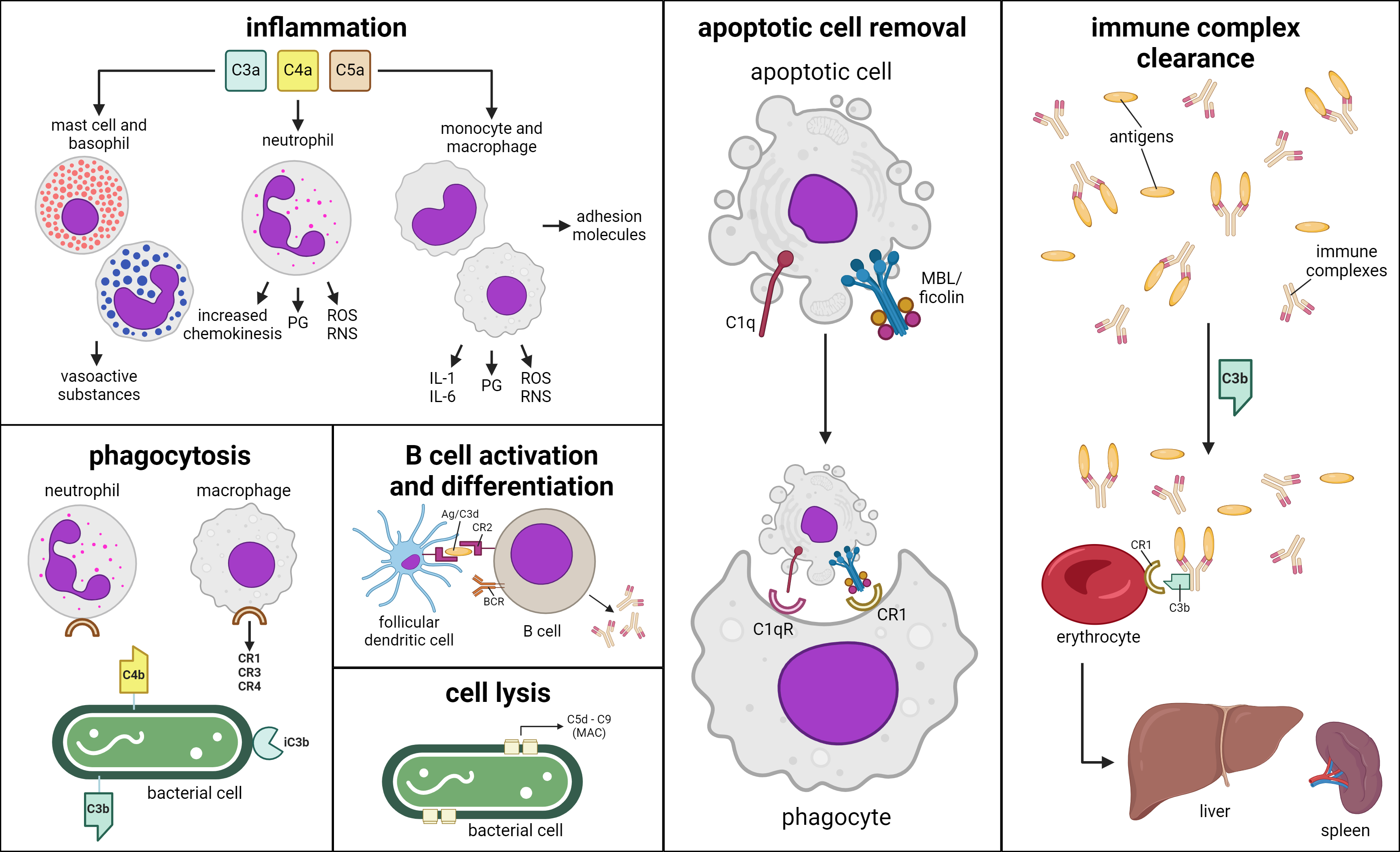
The lectin pathway is the oldest division of the complement system, found in sea urchins that developed about 700 million years ago. Its main actor is a protein called mannose binding lectin (MBL). Lectins are proteins that bind to sugar trees (glycan moieties) on glycoproteins. Mannose binding lectin is a lectin that binds to mannose, one of the sugars commonly found in glycoproteins.
Our cells have helpful proteins, like the weirdly-named delay accelerating factor and the appropriately named protectin (CD59) which protect us from the destructive tools of the complement pathway.
Media Attributions
- U15-066 Castle Walls © Turner, John S. is licensed under a CC BY-SA (Attribution ShareAlike) license
- U15-067 Neutrophils © NIAID is licensed under a CC BY (Attribution) license
- U15-068 Macrophage © NIAID is licensed under a CC BY (Attribution) license
- U15-069 Vasodilation © www.scientificanimations.com is licensed under a CC BY-SA (Attribution ShareAlike) license
- U15-070 Allergic to Antibiotic Cefaclor © Gouvas, Harry MD PhD is licensed under a CC BY-SA (Attribution ShareAlike) license
- U15-071 Chemotaxis of WBCs © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U15-072 Complement Pathway © NIH Publication No. 03–5423 is licensed under a Public Domain license
- U15-073 Mast Cell Degranulation © Crookston, Alexa is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U15-074 Functions of Complement System © Crookston, Alexa is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license

