Structures of the Respiratory System
Objective 2
Describe functions for each of the structures of the respiratory system: nose and paranasal sinuses, pharynx, larynx, trachea, bronchi, lungs, pleural membranes, diaphragm and intercostal muscles, phrenic nerves and pulmonary plexus. Be able to identify each of these on a diagram or photograph.
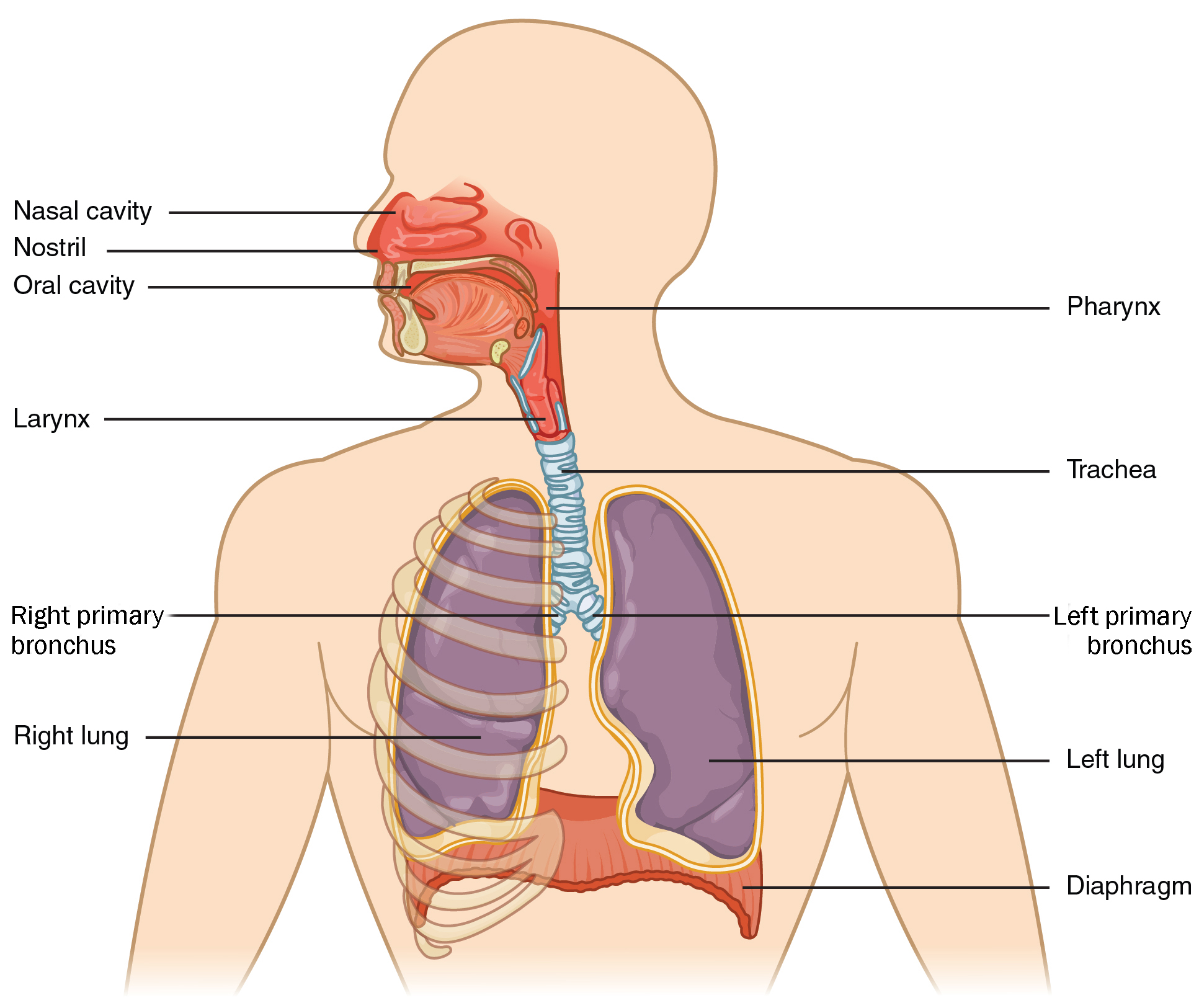
Let’s turn our attention to the structures of the respiratory system. Anatomically, these structures can be divided into the upper and lower respiratory tracts. The nose, paranasal sinuses, and pharynx make up the upper respiratory system. The larynx, or voice box separates the upper from lower respiratory system. The trachea, bronchi, and lungs make up the lower respiratory system.
We’ll begin with the structures of the upper respiratory tract.
Nose
The nose is made up of hyaline cartilage which gives it flexibility. Air enters through the external nares (nostrils). Nose hairs act as a filter for dirt and other particles in the inhaled air.
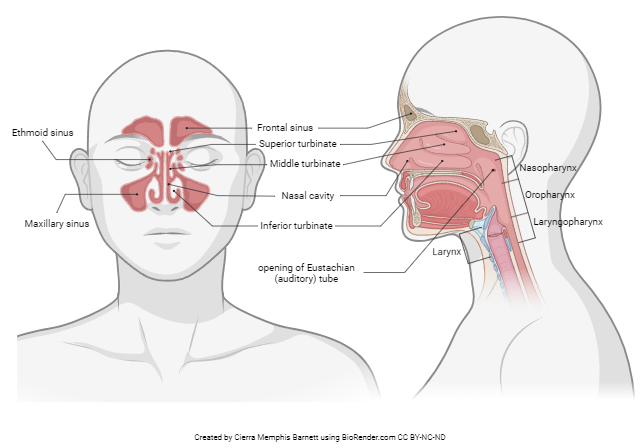
In the internal nose are scroll-like bones that make up the nasal conchae also called turbinates. The conchae provide a turbulent area that air passes through before reaching the rest of the respiratory passages. The conchae are lined with a mucous membrane which helps trap foreign particles and warms and humidifies the air. The olfactory epithelium, which is near the superior nasal concha, increases the surface area and mixes the air to help with olfaction.
Sinuses are cavities within cranial and facial bones that are lined with a mucous membrane. In the image, we can see the ethmoid, maxillary, and frontal sinuses. These hollow spaces lighten the weight of the head so we have an easier time carrying our head around. They also serve as chambers that resonate sound as we speak or sing. This is why you may sound funny when your sinuses are stuffed up with a cold. Due to our upright posture, our sinuses don’t drain as easily. They may trap microorganisms and fluid and we can find ourselves with a nasty sinus infection!
Pharynx
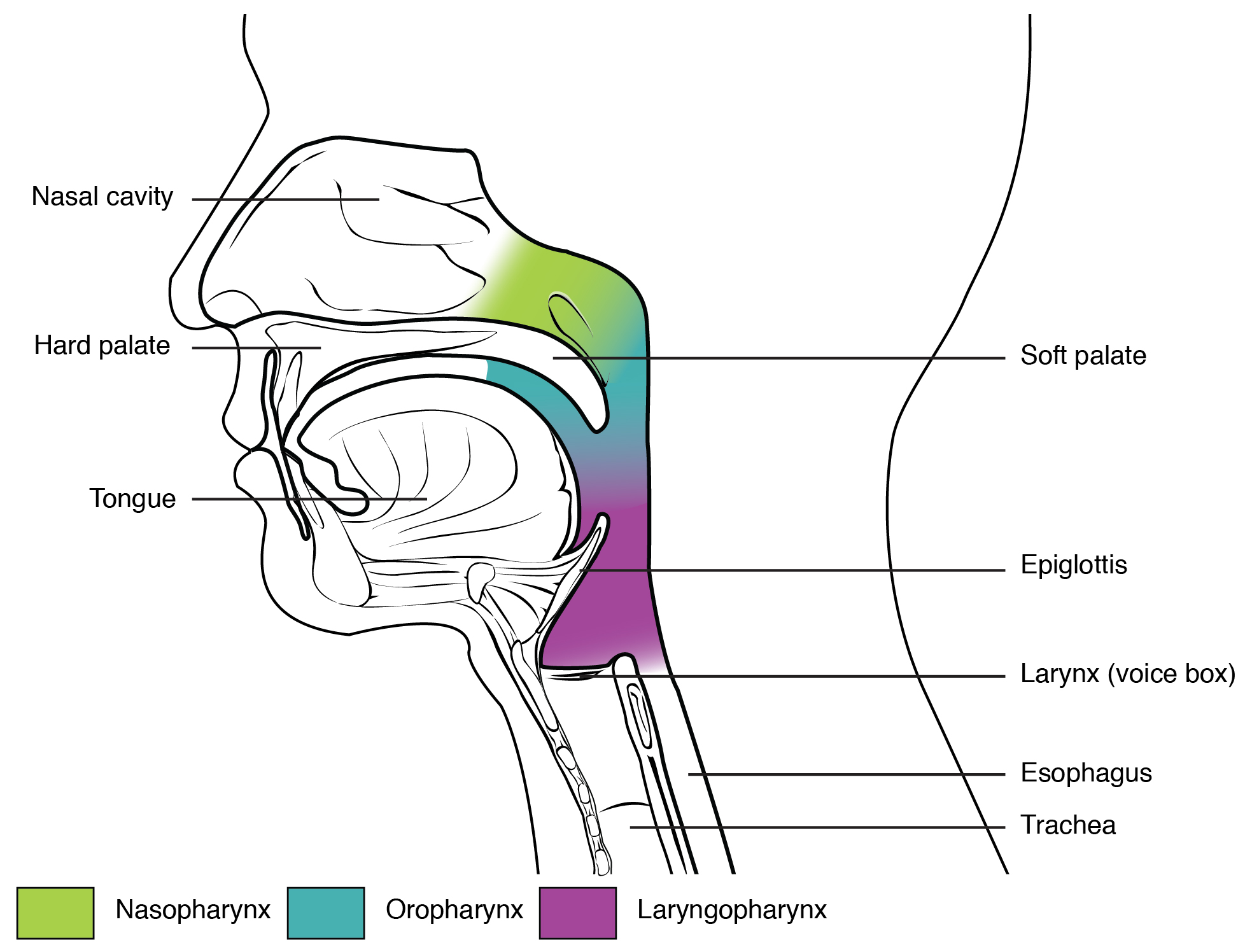
The pharynx or throat is a hollow tube that starts at the posterior part of the internal nares and descends to the opening of the larynx. The pharynx serves as a passageway for air and food, is a resonating chamber for sound, and houses the tonsils.
The pharynx can be divided into three anatomical regions.
- Nasopharynx: Lies behind the internal nares and has a purely respiratory function.
- Eustachian tubes (auditory tubes)
- Houses the pharyngeal tonsils (adenoids)
- Oropharynx: Lies behind the mouth with both reparatory and digestive functions.
- Houses the palatine tonsils (removed in a tonsillectomy) and the lingual tonsils
- Laryngopharynx: Lies inferior to the oropharynx and opens into the larynx and esophagus and has respiratory and digestive functions.
Larynx
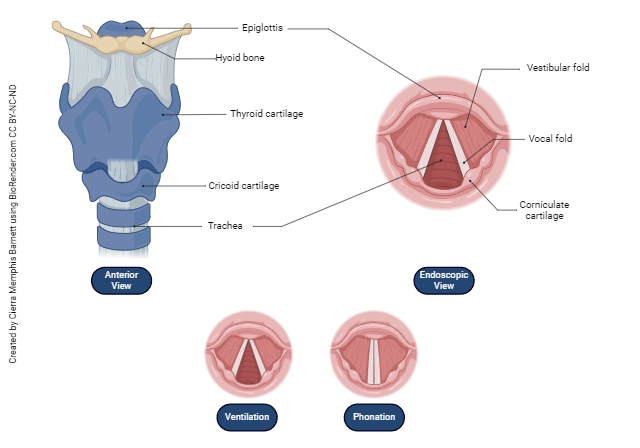
The larynx, or voice box, connects the laryngopharynx with the trachea. It sits in the midline of the neck anterior to the esophagus and superior to the trachea. The hyoid bone, an unattached, free-floating U-shaped bone, sits superior to the larynx. The opening of the larynx is the glottis.
Folds of tissue, the vocal cords, and the opening between them make up the glottis. Vibrations caused by air passing the vocal cords produces sound. The greater the pressure, the louder the sound. Tension on the vocal cords produces pitch. Men’s vocal folds become thicker and longer during puberty under the influence of male sex hormones (androgens) which results in a lower pitched voice. The production of speech sounds is termed phonation.
Trachea
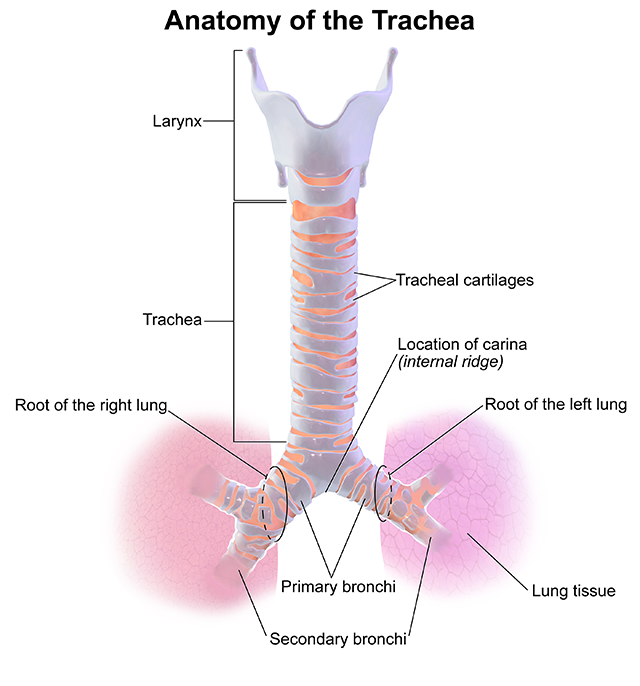
The trachea or windpipe is a semi-rigid passageway for air that’s about 12 cm (5 inches) long. Incomplete cartilage rings resembling the letter C surround the trachea, giving it support and preventing collapse especially during inhalation. The trachea is anterior to the esophagus. The posterior surface of the trachea is shared with the esophagus.
The carina is an internal ridge where the trachea divides into the right and left bronchi. The carina (Latin for boat prow) is used as a landmark when performing a bronchoscopy or visual examination of the bronchi. The carina is very sensitive area for triggering the cough reflex.
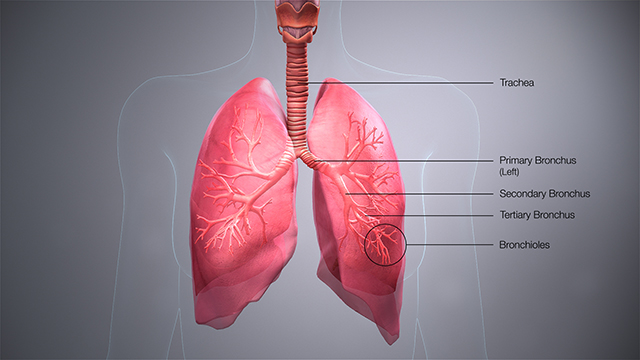
The trachea divides into the right and left primary bronchi. The bronchi resemble an inverted tree, branching into divisions of secondary bronchi, tertiary bronchi, and eventually into the tiny bronchioles and terminal bronchioles. The right primary bronchus extends more vertically, is wider, and shorter than the left. Because of this, an aspirated object is more likely to lodge in the right bronchus than the left.
Lungs
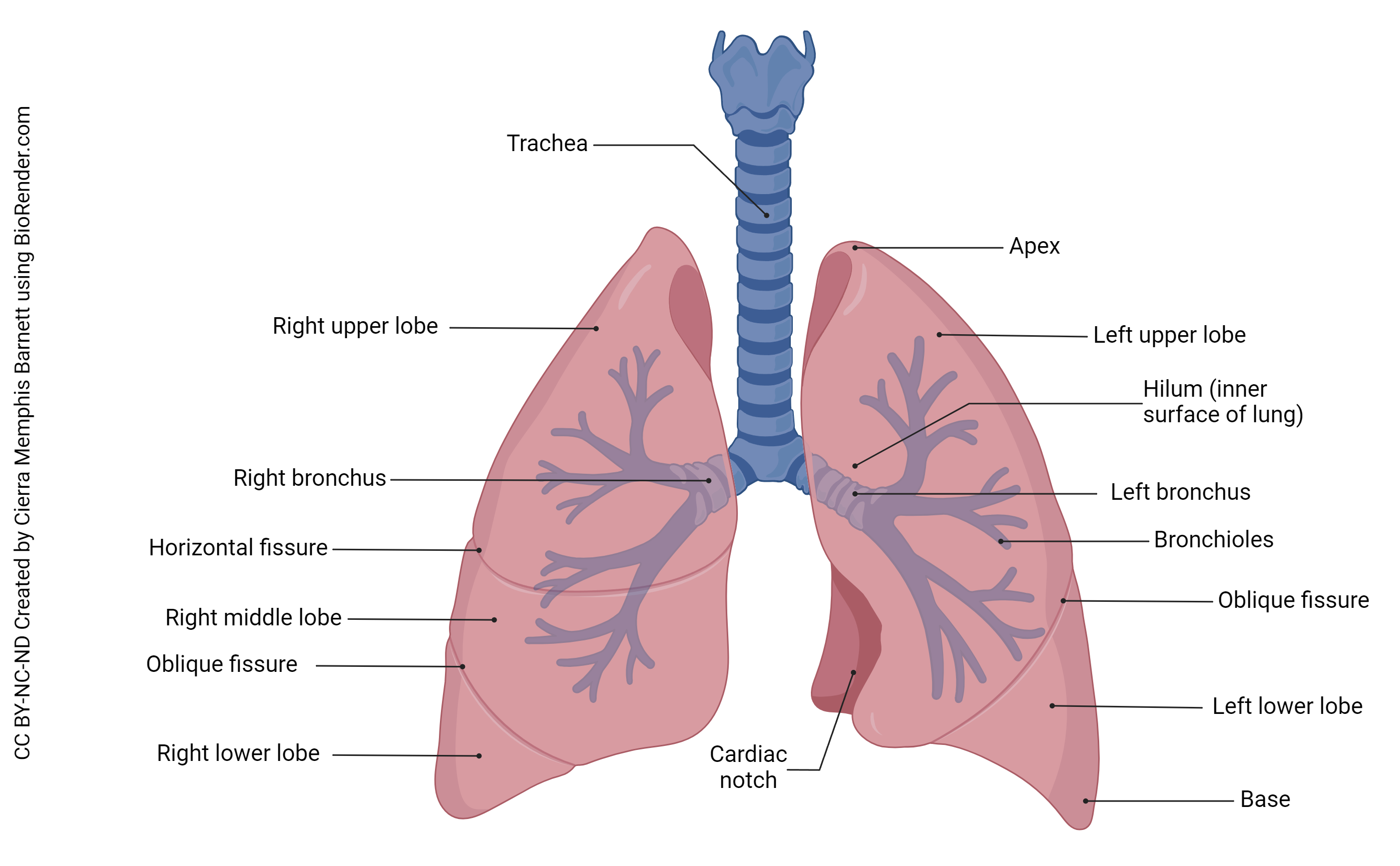
The right and left lungs are slightly different. The right lung contains 3 lobes while the left contains 2. This is because the apex of the heart rests at the medial portion of the left lung, the cardiac notch. The three lobes of the right lung are named the inferior, middle, and superior lobe. The lobes of the lungs are separated by fissures with the horizontal fissure separating the superior (upper) lobe and the middle lobe and the oblique fissure separating the middle lobe and the inferior (lower) lobe. As for the left lung, there is only an oblique fissure separating the superior (upper) and inferior (lower) lobes.
The apex or superior part of the lung rests slightly above the clavicle.
The base of each lung rests on the diaphragm. The anterior, lateral, and posterior surfaces of the lungs rest against the ribs.
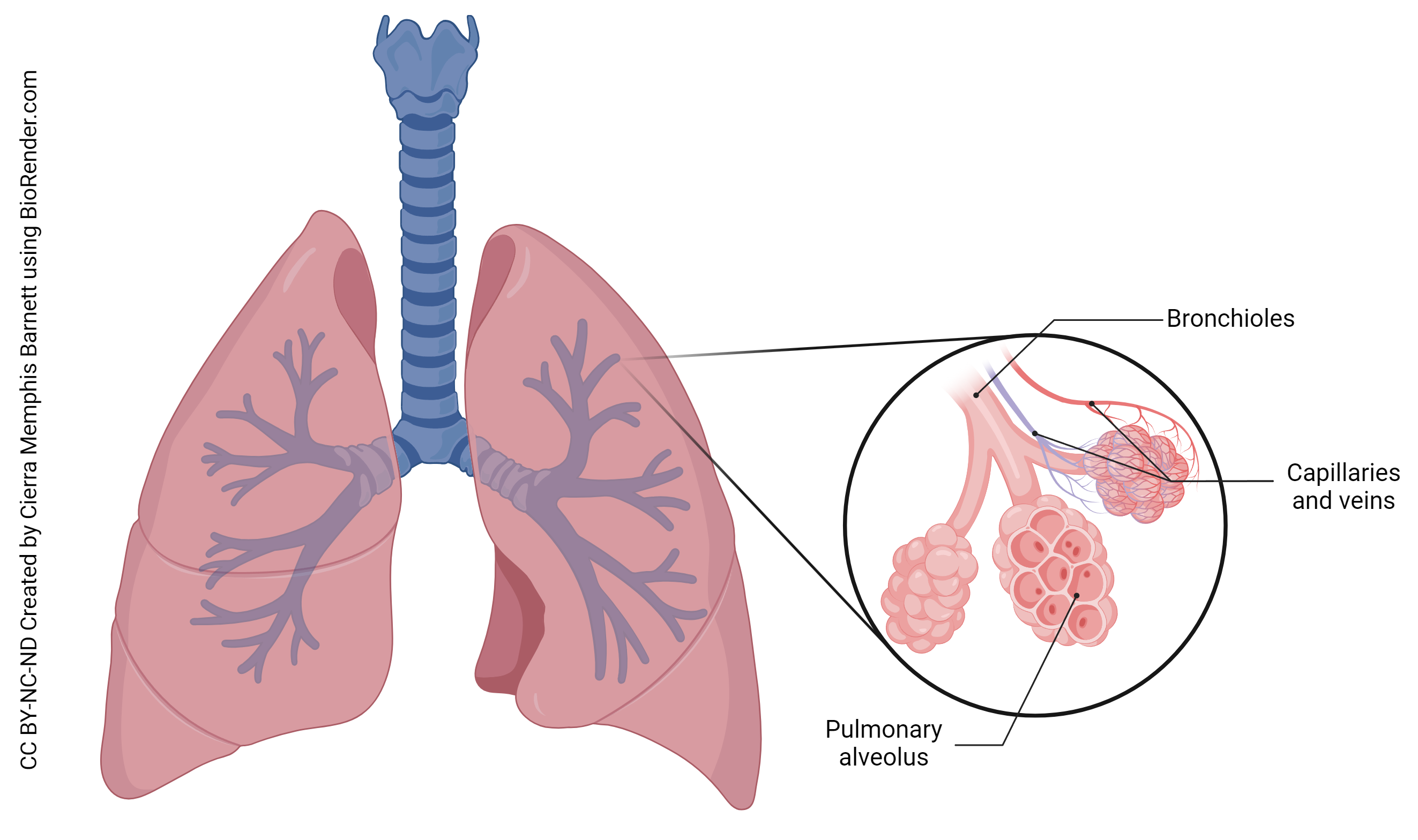
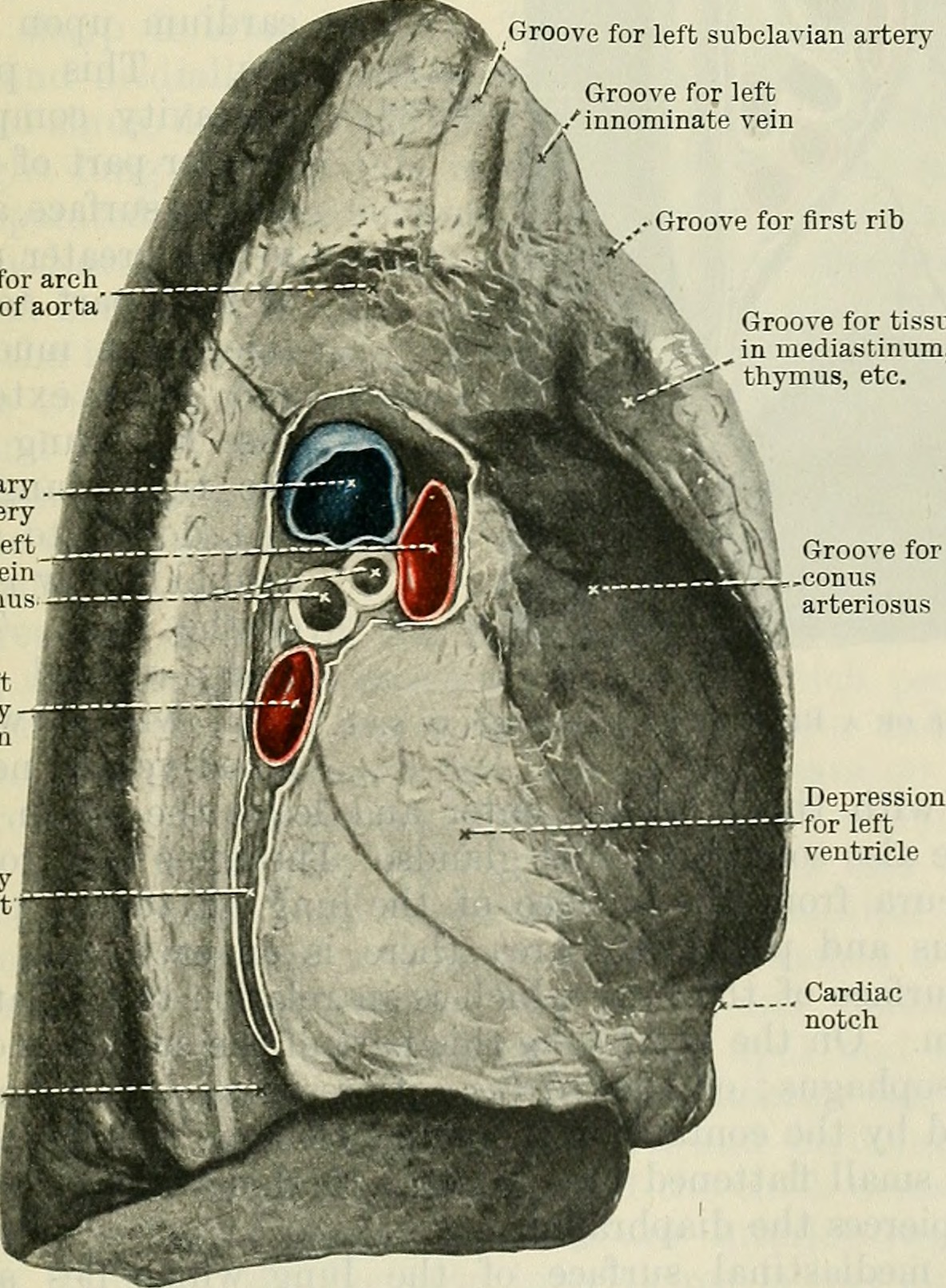
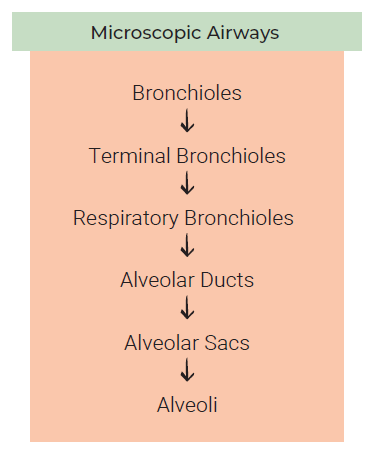
The primary bronchi, blood vessels, lymphatic vessels, and nerves enter the lungs at the hilum, an opening on the medial surface of each lung. The primary bronchi branch to form secondary bronchi, one for each lobe of the lung. The secondary bronchi further branch to form tertiary bronchi and then these branch into bronchioles. Eventually, bronchioles divide into several alveolar ducts. These ducts end in grape-like clusters called alveoli. The alveoli provide a large surface area for the exchange of gases. It’s estimated that the lungs contain 300 million alveoli, giving a surface area about the size of a racquetball court for gas exchange!
Pleural Membranes
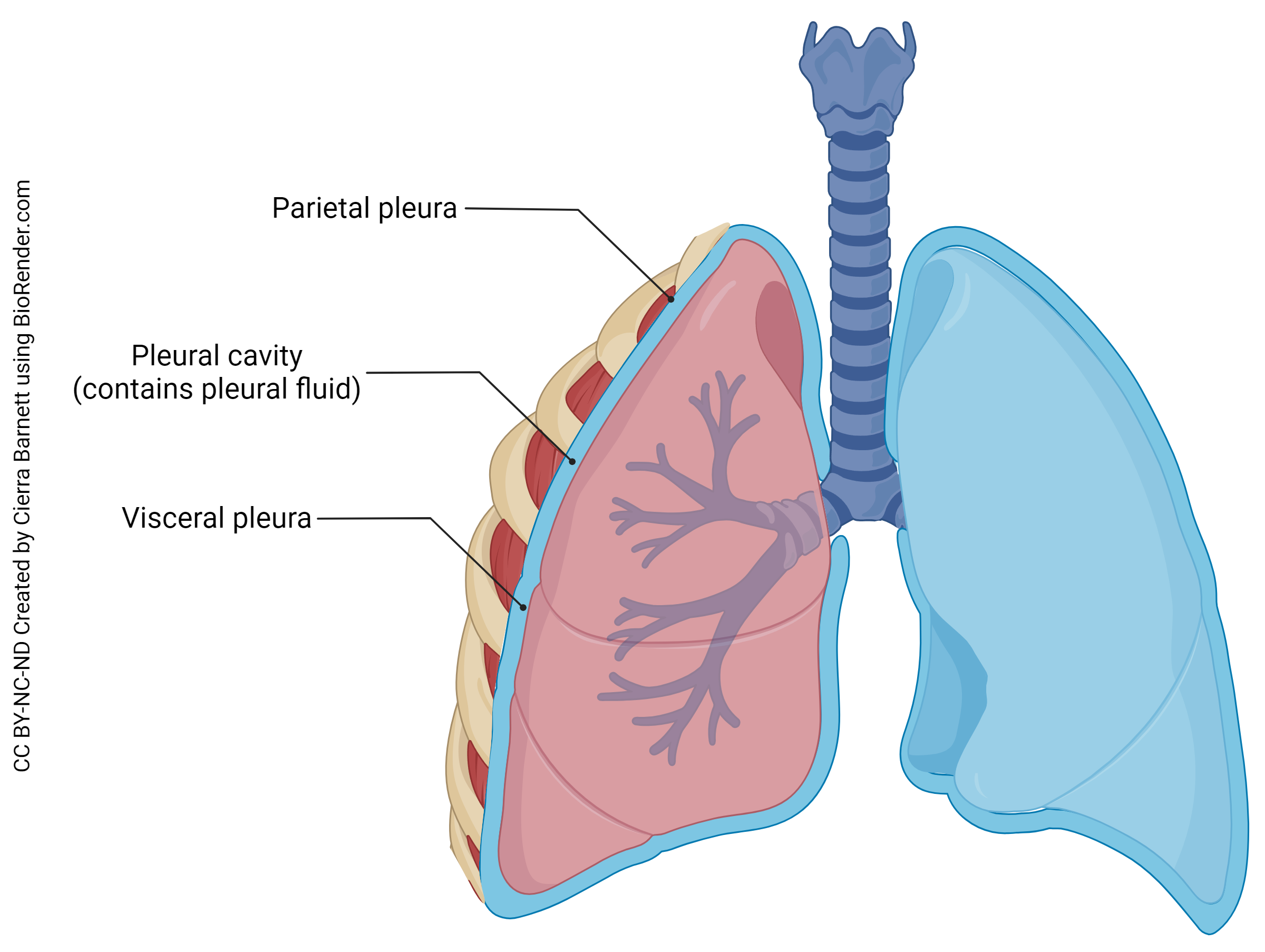
The lungs, like other visceral organs, are covered with a double-walled serous membrane. Remember that serous membranes line organs and body cavities that do not open to the external world. A serous membrane consists of areolar connective tissue covered by simple squamous epithelium (mesothelium). The visceral pleura adheres to the lung. The parietal pleura adheres to the chest wall. Between the two pleura is a small space, the pleural cavity which contains pleural fluid. This fluid reduces friction. The pleural fluid allows easy movement as the lungs expand and contract. The fluid also allows the two layers of the membrane to adhere to each other because of the surface tension it creates.
Clinical Connection: Pleurisy & Pleural Effusion
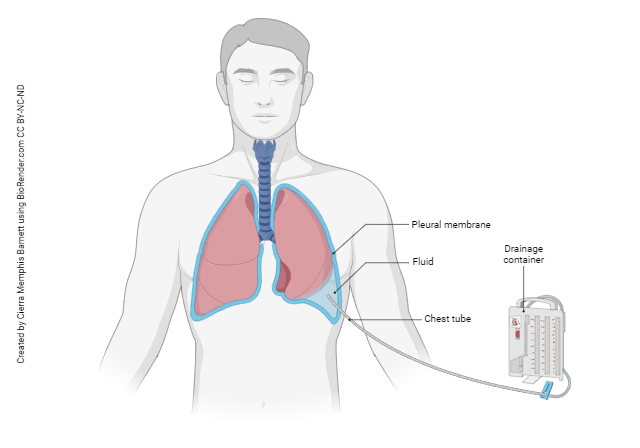
If the pleural membrane becomes inflamed, a condition called pleurisy occurs. Pleurisy can be extremely painful because of friction between the two layers of the pleural membrane.
Excess fluid may accumulate in the pleural cavity due to inflammation. This serious condition, called pleural effusion, makes it difficult to breathe.
Diaphragm
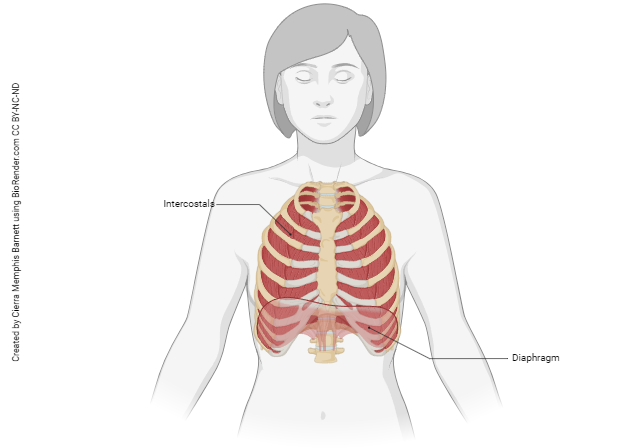
The inferior portion of the lungs rest on a large, dome-shaped muscle, the diaphragm. This muscle, which forms the floor of the thoracic cavity, is the most important muscle that powers breathing. Contraction of this muscle enlarges the thoracic cavity enabling inhalation (more about this to come).The diaphragm is responsible for about 75% of the air that enters the lungs during normal quiet breathing.
Intercostals
You may recall from Unit 10 that we have intercostal muscles that assist with breathing. The internal intercostal muscles make up the intermediate layer of the intercostal space. These muscles help decrease the size of the thoracic cavity during forced exhalation. The external intercostals assist with inhalation.
Accessory Respiratory Muscles
There are several muscle that assist with respiratory movements when needed. For inhalation, these muscles include the sternocleidomastoid, scalenes, pectoralis minor, and serratus anterior. For exhalation, these muscles include the transversus thoracis and abdominal muscles.
Innervation
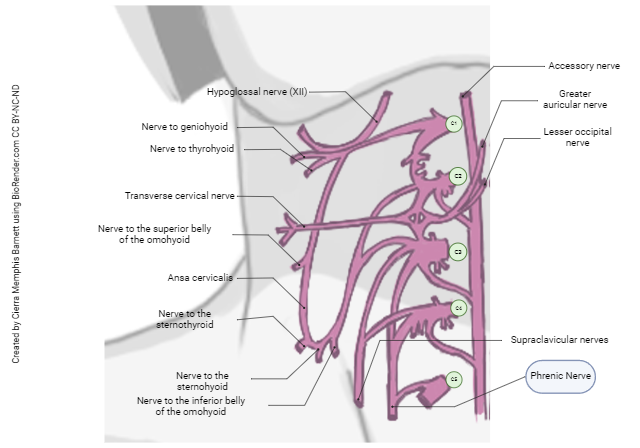
The phrenic nerve arises from the cervical plexus at levels C3, C4, and C5. It stimulates the diaphragm muscle to contract, enabling inspiration. The mnemonic “C3, 4, 5, keep the diaphragm alive” can help you remember the origin of this important spinal nerve.
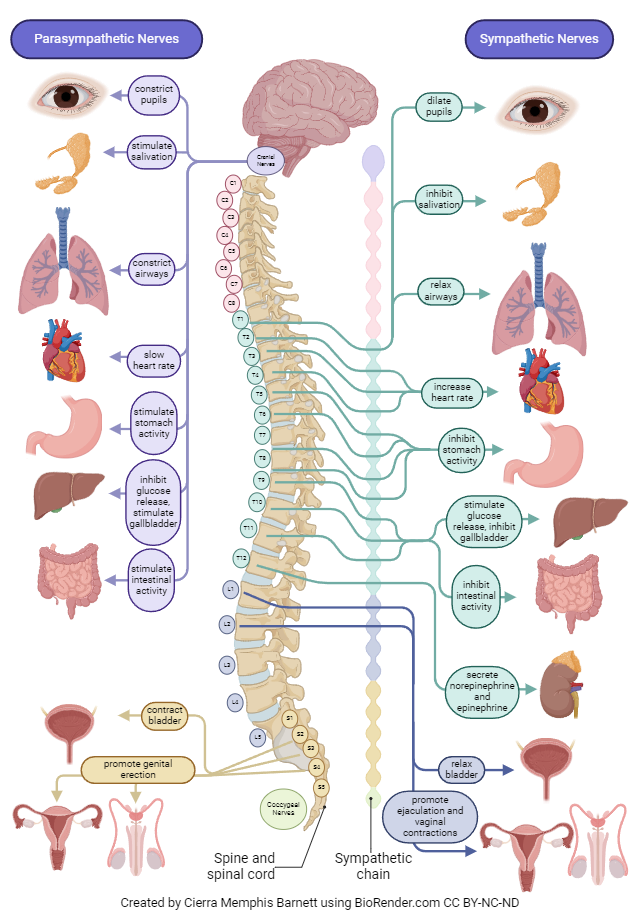
The lungs receive both sympathetic and parasympathetic innervation.
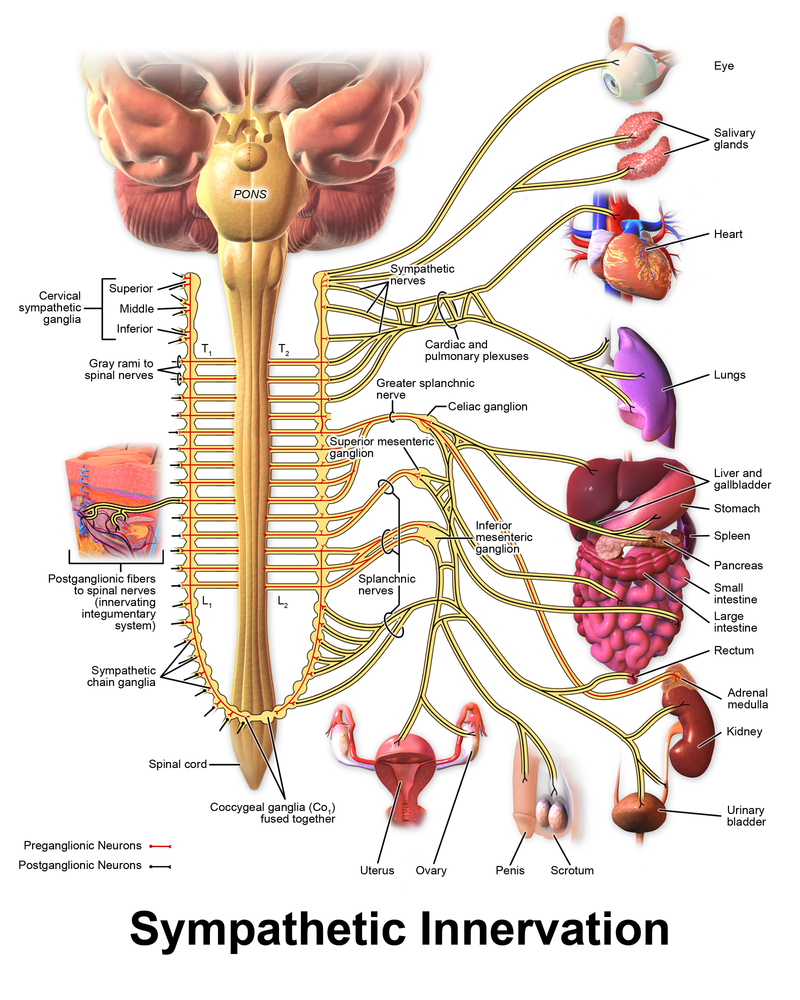 Remember that the sympathetic nervous system enables the “fight or flight” response. If you were running from a saber-tooth tiger (or on a hot date) you would need more air to your lungs. Under sympathetic stimulation, smooth bronchial muscle dilates. Sympathetic nervous stimulation arises from the thoracolumbar region of the spinal cord. Sympathetic nerves that innervate the lungs have cell bodies in the intermediate horn (sides of the gray matter) in the T1-T4 areas of the spinal cord. The nerves synapse at the sympathetic chain ganglia (along the sides of the spinal cord). The nerves enter the lungs at the hilum forming the pulmonary plexus.
Remember that the sympathetic nervous system enables the “fight or flight” response. If you were running from a saber-tooth tiger (or on a hot date) you would need more air to your lungs. Under sympathetic stimulation, smooth bronchial muscle dilates. Sympathetic nervous stimulation arises from the thoracolumbar region of the spinal cord. Sympathetic nerves that innervate the lungs have cell bodies in the intermediate horn (sides of the gray matter) in the T1-T4 areas of the spinal cord. The nerves synapse at the sympathetic chain ganglia (along the sides of the spinal cord). The nerves enter the lungs at the hilum forming the pulmonary plexus.
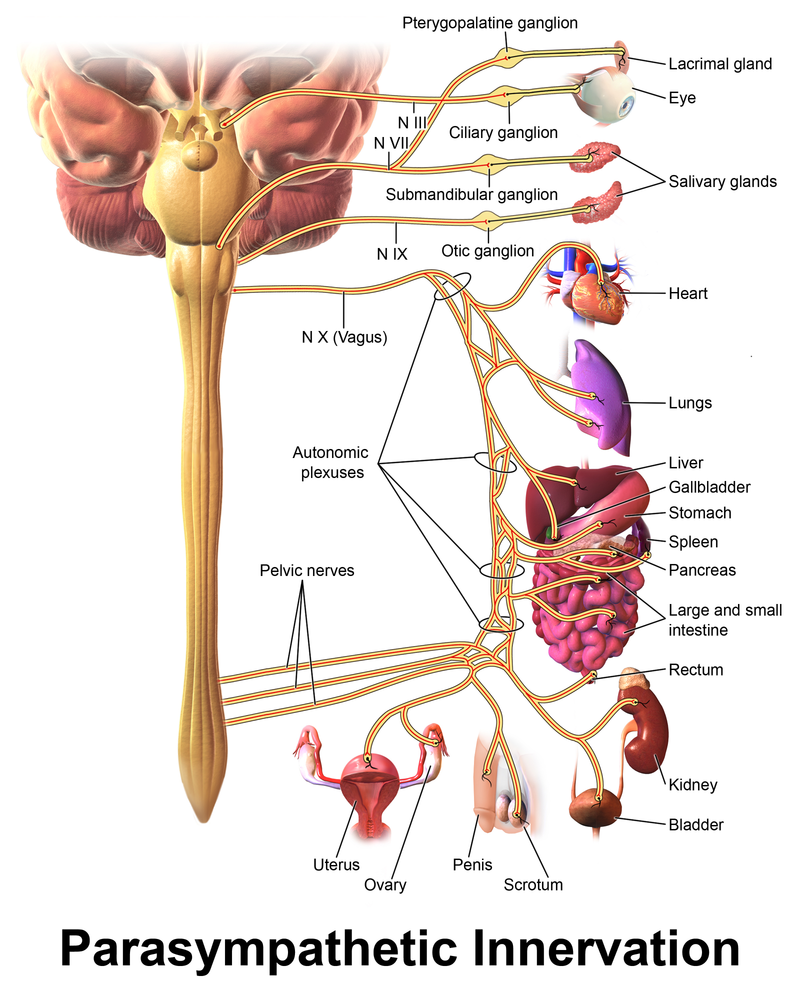
Remember that the parasympathetic nervous system enables the “rest and repose” response. Think post-Thanksgiving dinner; breathing is barely necessary when one is semi-comatose digesting on the couch. Parasympathetic stimulation causes mucus secretion and constriction of bronchial smooth muscle. The parasympathetic nerve innervating the lungs is cranial nerve X, the vagus nerve, using acetylcholine as the neurotransmitter.
Media Attributions
- U17-002 Major Respiratory Organs © Ernstmeyer, K. & Christman, E., eds. is licensed under a CC BY (Attribution) license
- U17-003 Nose Anatomy Memphis © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U17-004 Pharynx Divisions © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U17-005 Larynx Anatomy © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U17-006 Trachea Anatomy © BruceBlaus is licensed under a CC BY (Attribution) license
- U17-007 Bronchus Description © www.scientificanimations.com is licensed under a CC BY-SA (Attribution ShareAlike) license
- U17-008a Lung Anatomy © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U17-009 Airway Itinerary © Burr, Justin is licensed under a CC BY-SA (Attribution ShareAlike) license
- U17-010 Alveolus in Lung © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U17-008b Hilum © Cunningham, Daniel John & Robinson, Arthur is licensed under a Public Domain license
- U17-011 Pleura of Lung © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U17-012 Pleural Effusion © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U17-013 Diaphragm and Intercostals © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U17-014 Phrenic Nerve in Cervical Plexus © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U12-019 Sympathetic Innervation © BruceBlaus is licensed under a CC BY (Attribution) license
- U12-021 Parasympathetic Innervation © BruceBlaus is licensed under a CC BY (Attribution) license
- U17-015 Parasympathetic and Sympathetic Nervous Systems © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license

