Stomach
Objective 4
Indicate the location of the following stomach regions: cardiac, fundus, pylorus. Identify the sphincters of the stomach and their function: cardiac, pyloric. Describe the histology and function of the unique features of the stomach: oblique muscle layer, chief cells, parietal cells, enteroendocrine cells, and mucous cells. Explain the function, production, and regulation of hydrochloric acid (HCl).
Food and liquid leaving the esophagus pass through the lower esophageal sphincter (also called the cardiac sphincter) as they enter the stomach. The lower esophageal sphincter sometimes fails to tightly close, causing a condition called gastroesophageal reflux disease (GERD). GERD can be caused by increased abdominal pressure, as in obesity.
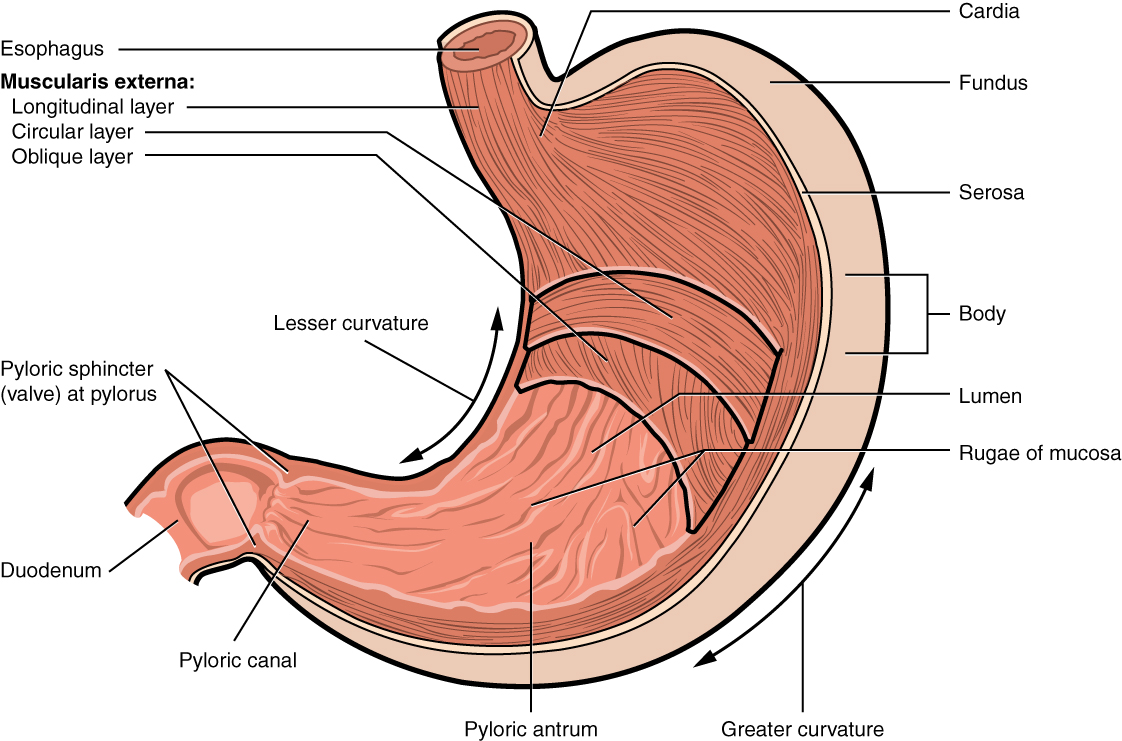
The stomach has five regions and two curves. The cardia is the point at which the esophagus crosses the diaphragm to become the stomach. The fundus (as in the fundus of the eye, or fundus of the uterus) comes from the same word as “foundation” of the bottle. The bulk of the stomach is the body, and the narrower part nearest the small intestine is the pylorus (Greek πσραλος, “gate-keeper”). The pyloric antrum (Latin, “cave”) transitions to the pyloric canal.
The stomach is a curved bag, and the smaller of the two curves is called, naturally enough, the lesser curvature while the larger arc is the greater curvature.
As mentioned previously, the “valve” between esophagus and stomach is the lower esophageal sphincter (cardiac sphincter). At the end of the pyloric canal is the pyloric sphincter, which represents the end of the stomach and outlet for stomach contents. The pyloric sphincter opens into the duodenum (Latin: “12 finger breadths”), which is the initial segment of the small intestine.
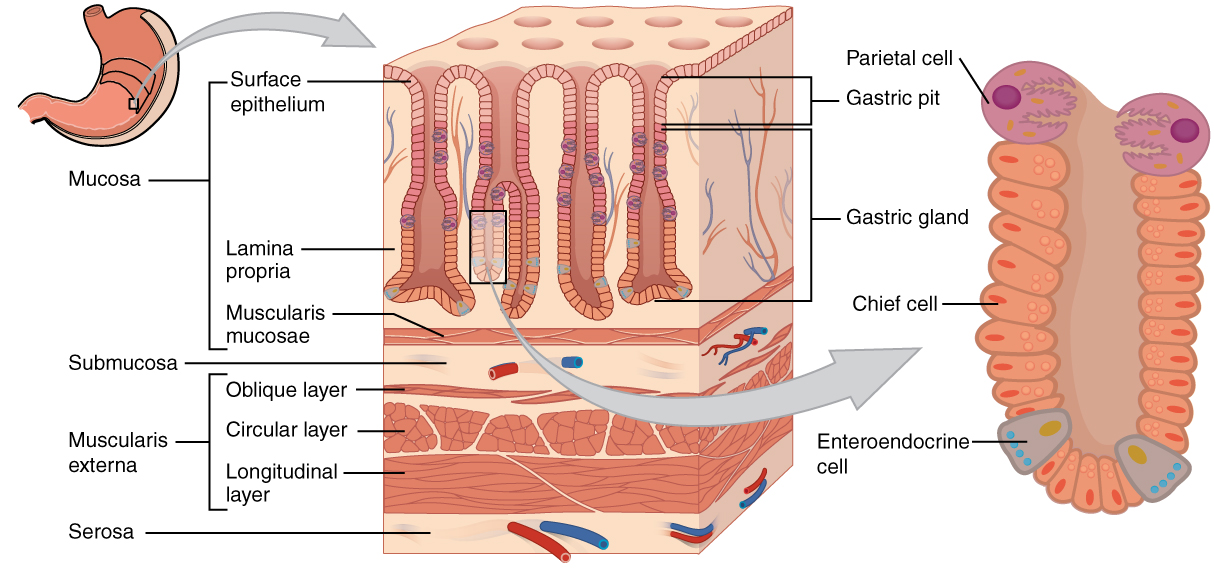
Like the other regions of the GI tract, the stomach follows the basic histological plan laid out in earlier. In the stomach, the mucosa layer is specialized for the digestion of food. The specialization takes the form of gastric pits. Each of these depressions is lined with a simple columnar epithelium. The bottom half of each gastric pit has a higher concentration of glandular cells that collectively are called the gastric glands.
Along the stomach lumen, epithelial cells and surface mucous cells predominate. Mucus is an essential part of the stomach lining, and protects the cells on the surface from being damaged by the acid and enzymes secreted by the stomach. Further from the luminal surface (albuminal), the gastric pit has a number of secretory (glandular) cells.
Let’s now explore the cells of the mucosa layer with more depth.
Cells of the Mucosa Layer
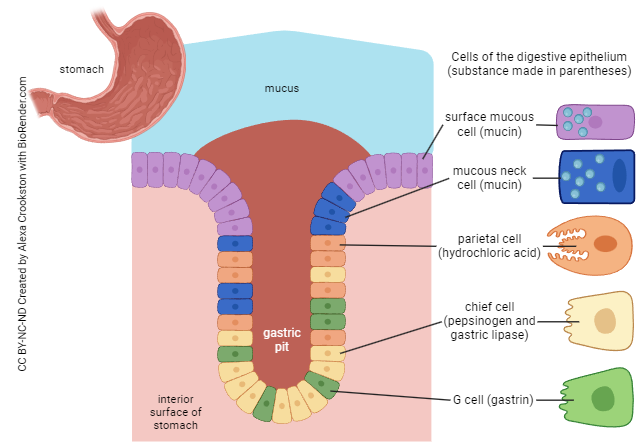
Mucous neck cells secrete protective mucus.
Parietal cells have two essential roles. First, they have specialized protein pumps that dump H+ and Cl– ions into the lumen, making HCl (stomach acid). More about this later. Second, they secrete intrinsic factor. Intrinsic factor is critical for absorption of vitamin B12. B12 is needed for red blood cell production. Decreased production of intrinsic factor leads to pernicious anemia.

Now let’s discuss stomach acid. In HTHS 1110, we discussed several types of ion transport. We use two of these to “run” the secretion of stomach acid by parietal cells:
- an active transport process (“pump”) that uses ATP as an energy source, and expels one H+ ion from the cell for every K+ it brings in (the H+/K+ ATPase); and
- an antiporter that allows bicarbonate ion (HCO3–) to run down its concentration gradient, which catapults Cl– from the interstitial fluid into the parietal cell.
Carbon dioxide (CO2) and water in the stomach are turned into carbonic acid (H2CO3) by the enzyme carbonic anhydrase, found in parietal cells. Because H2CO3 is an acid, it dissociates into H+ ions (protons) and bicarbonate ion (HCO3–). The HCO3– is used to buffer the blood.
The H+ is pumped out of the parietal cell, against its concentration gradient (H+ is lower inside than outside the parietal cell), by the H+/K+ ATPase.
Disease can increase the secretion of stomach acid, or more commonly, decrease the secretion of protective materials (such as mucus from surface mucous cells and mucous neck cells). When this happens, the stomach has an increased tendency to ulcerate. For example, the bacterium Helicobacter pylori disrupts the secretion of protective mucus and predisposes patients to gastric ulcers. Failure of the pancreas to make bicarbonate can result in duodenal ulcers.
Several neurotransmitter/hormones promote the secretion of stomach acid by parietal cells. Examples include acetylcholine released from the vagus nerve, gastrin from G cells of the stomach, and histamine from mast cells in the lamina propria. Mast cells are activated by any inflammatory process, so chronic inflammation may lead to gastric ulcers. Most drugs given for ulcer relief act on one of these neurochemical systems, as shown above. For example, cimetidine (Tagamet™) acts to block the H2 subtype of histamine receptors, and thereby decreases acid secretion. Another class of drugs that one sees heavily advertised on television act by inhibiting the proton pump (H+/K+ ATPase) shown on the previous page. Examples of these proton-pump inhibitors (PPIs) include: omeprazole (Prilosec™), lansoprazole (Prevacid™), and esomeprazole (Nexium™). These drugs reduce the secretion of HCl by parietal cells and can reduce the symptoms of gastroesophageal reflux disease.
Chief cells secrete the enzymes pepsinogen and lipase. Note that stomach enzymes, such as pepsin, have been known for so long that they carry names that were created before the modern naming convention of adding “-ase” to the substrate.
G cells are an example of enteroendocrine cells, a kind of hormonal system in the GI tract. They secrete the hormone gastrin. Later objectives focus on the enteroendocrine system.
Muscularis Layer
Another special feature of the stomach is the presence of an “extra” layer in the thick muscularis: the oblique muscle layer with fibers running diagonally. This layer aids in the stomach’s ability to “churn” substances and speed digestion.
Media Attributions
- U18-018 Stomach © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U18-019 Stomach Histology © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U18-020 Gastric Gland © Crookston, Alexa is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U18-021 Parietal Cell Producing Stomach Acid © Hutchins, Jim is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license

