Small Intestine
Objective 5
Indicate the location of the following regions: duodenum, jejunum, ileum. Describe the histology and function of the unique features of the small intestine: plicae circularis, villi, and microvilli. Identify the organs and specific cellular and molecular structures involved in the absorption of each of the major nutrient types: monosaccharides; peptides and amino acids; fatty acids and monoglycerides. Explain the classification of fat-soluble and water-soluble vitamins. Discuss the absorption of vitamin B12 and its role in pernicious anemia.
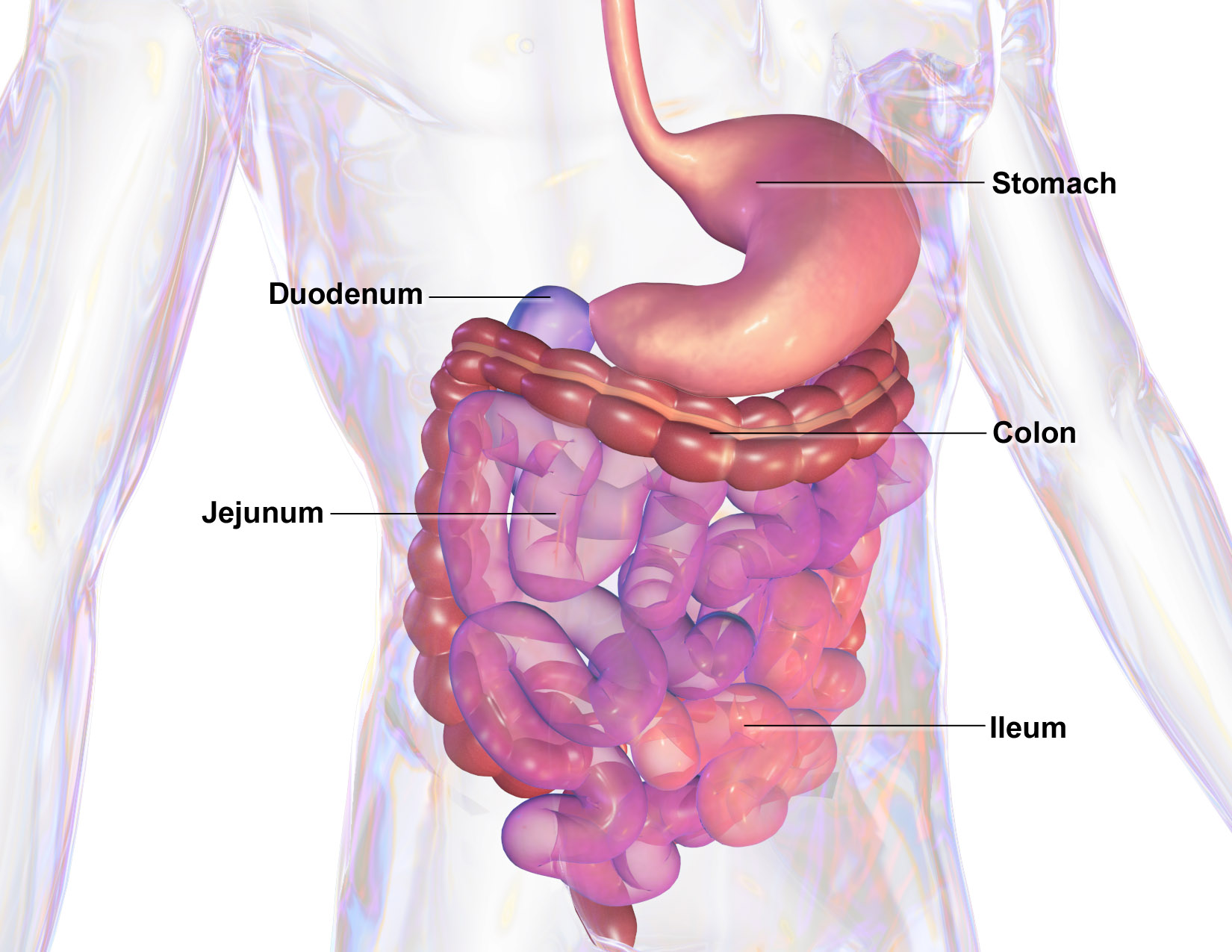
The small intestine has three regions. From stomach to large intestine, they are:
- duodenum (Latin: “12 finger breadths”) — about 0.25 m in length
- jejunum (Latin: “empty”) — about 1 m long
- ileum (Latin: “flank”) — about 2 m long
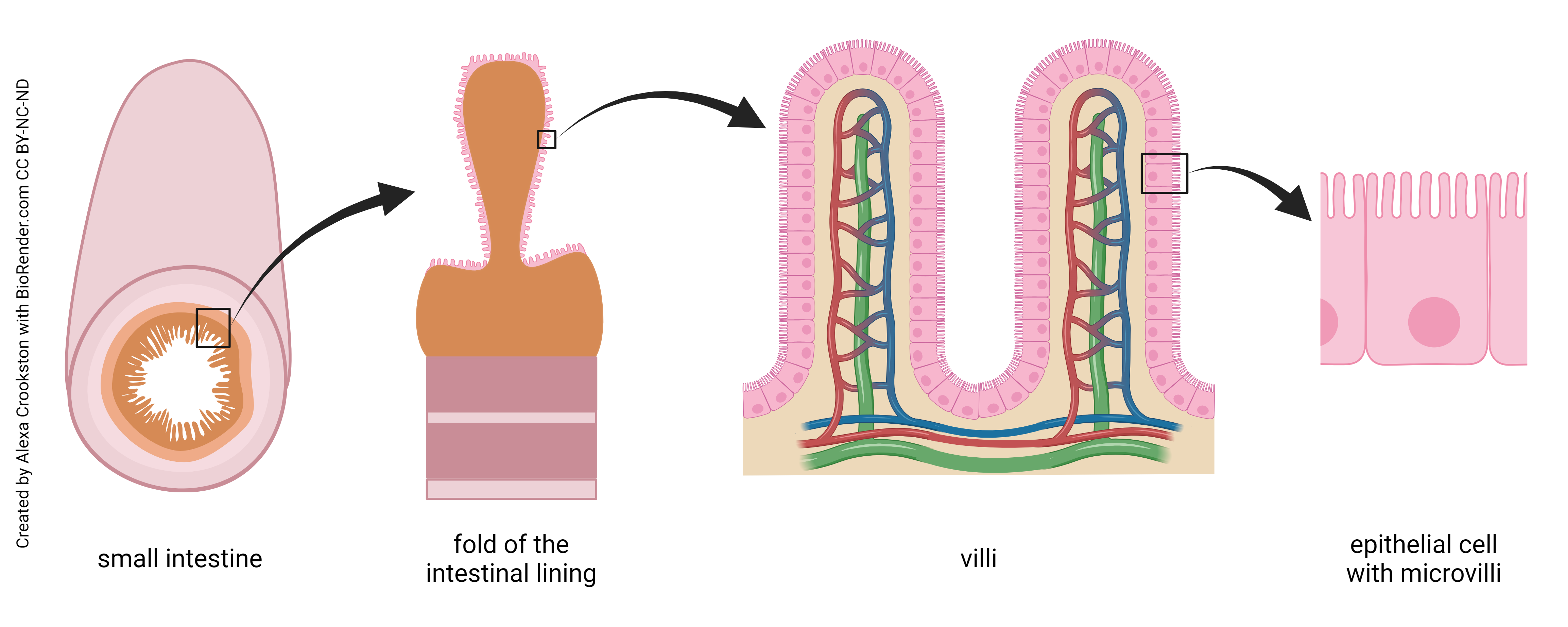
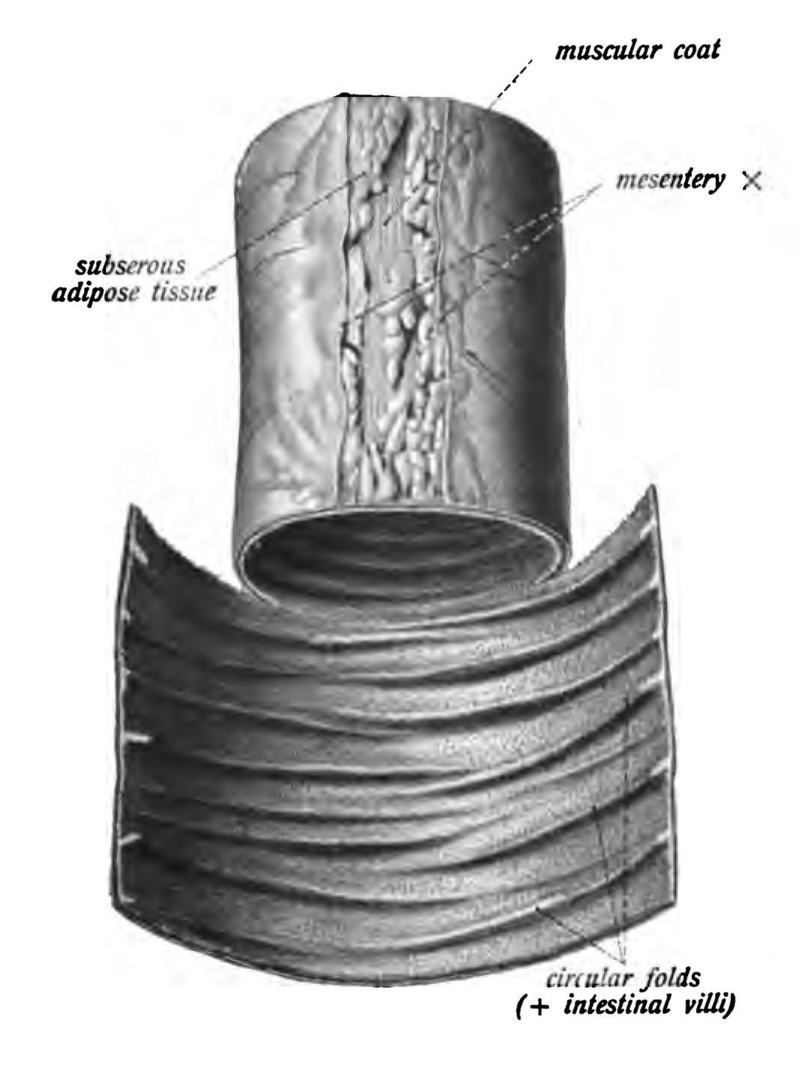 The lumen is wrinkly, with plicae circularis, the Latin name for “circular folds.”
The lumen is wrinkly, with plicae circularis, the Latin name for “circular folds.”
The histology of the small intestine is exactly what we learned earlier, because the small intestine is used as the “model” for the histology of the GI tract.
In the mucosa, the epithelial layer consists of a simple columnar epithelium called enterocytes or absorptive cells. The shape of these cells allows them to absorb water and nutrients on their apical (luminal) surfaces, process the nutrients as necessary, and then drop absorbed substances into the capillary bed on the basal (abluminal) surface.
For this reason, the lamina propria of the mucosa has a rich capillary bed, with numerous arterioles and venules. Also, a small lymph vessel called a lacteal carries lipid from the absorptive epithelium. These lymphatics eventually gather into the thoracic duct which, in turn, releases into the bloodstream at the left jugular/subclavian junction.
The muscularis layer reverts to the “normal” two sublayers of smooth (autonomic) muscle fibers: a circular and a longitudinal layer. Between them lie the clusters of neurons that control autonomic movements of the intestines: the myenteric plexi. As we’ll see later, these neurons generate the peristaltic waves that keep things moving in the GI tract.
The luminal surface of the small intestine appears velvety. This is because of the presence of villi (sing.: Latin villus, “shaggy”). These finger-like projections are about 1 mm long by 0.1 mm diameter. Their diameter is just at the limit of human vision, so that’s why it looks like velvet. With a little magnification, the intestinal surface looks like pink shag carpeting.
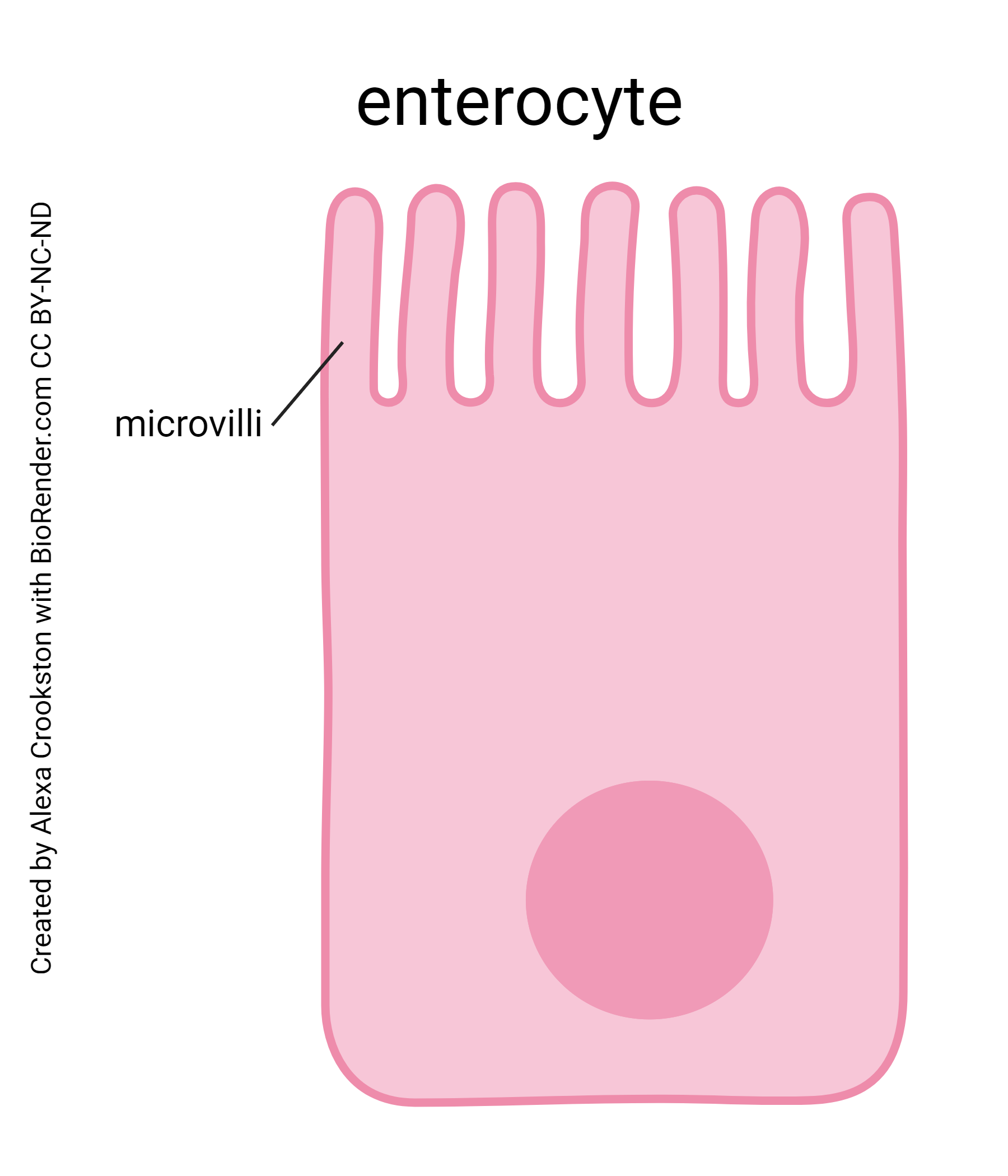
Most of the villi’s epithelial cells are specialized for absorption — the enterocyte. These cells are coated with microvilli, a smaller version of the villi. Microvilli are about 1/1000 the size of villi (micro–, 1/1000, get it?) and are thus about 1 μm long.
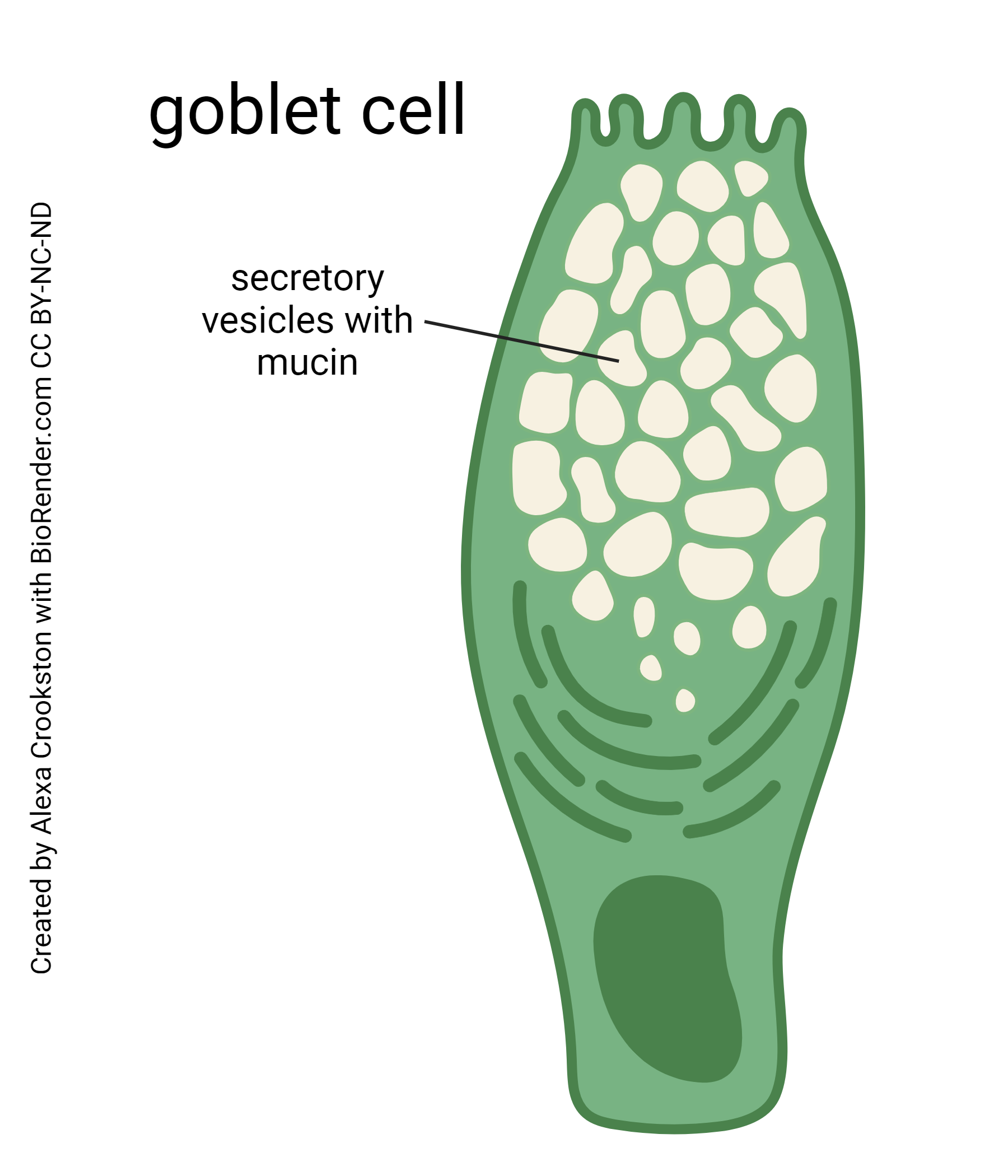
The epithelium has its share of mucus-secreting goblet cells.
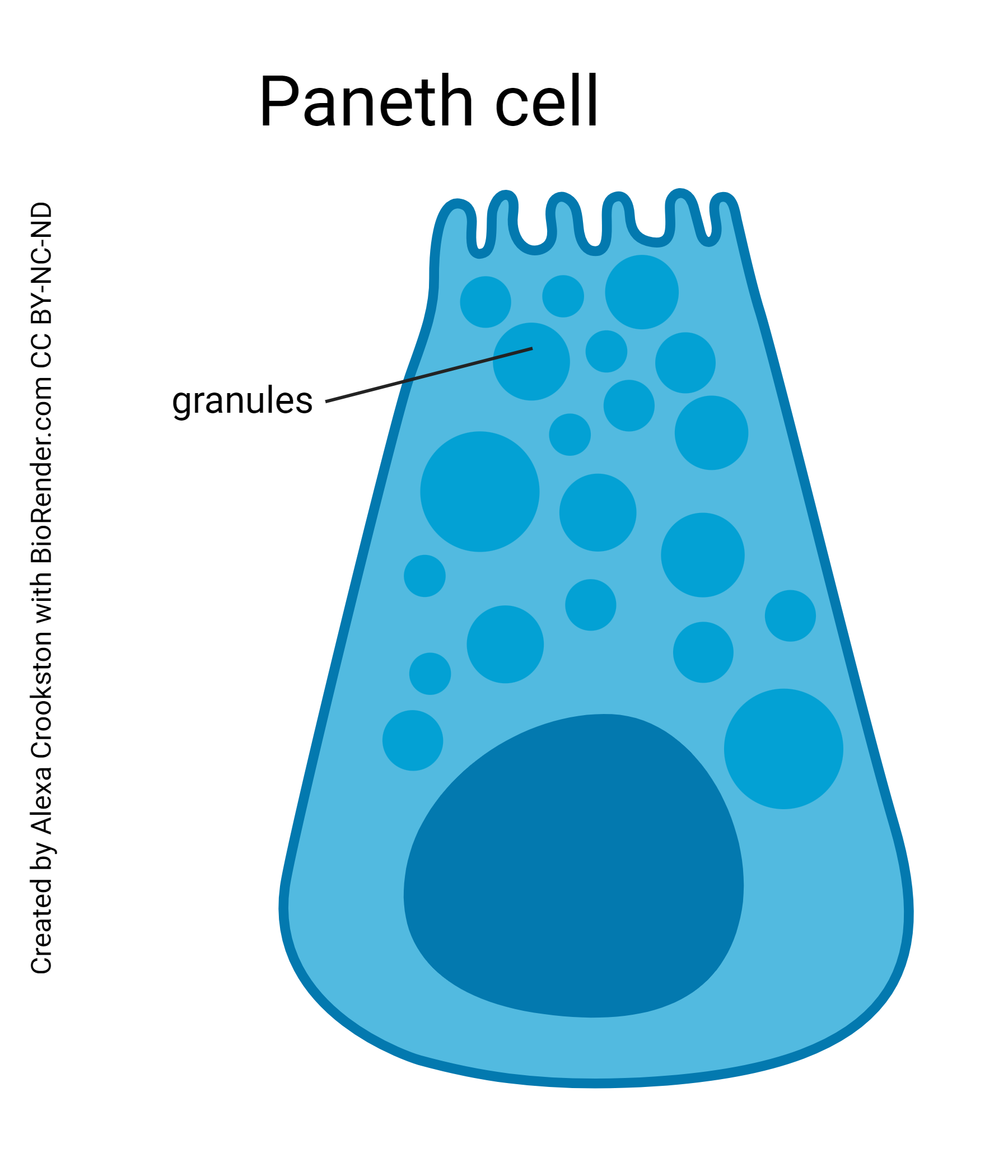
Enzyme-secreting cells of the intestine are called Paneth cells. They secrete many enzymes. They are also capable of phagocytosis.
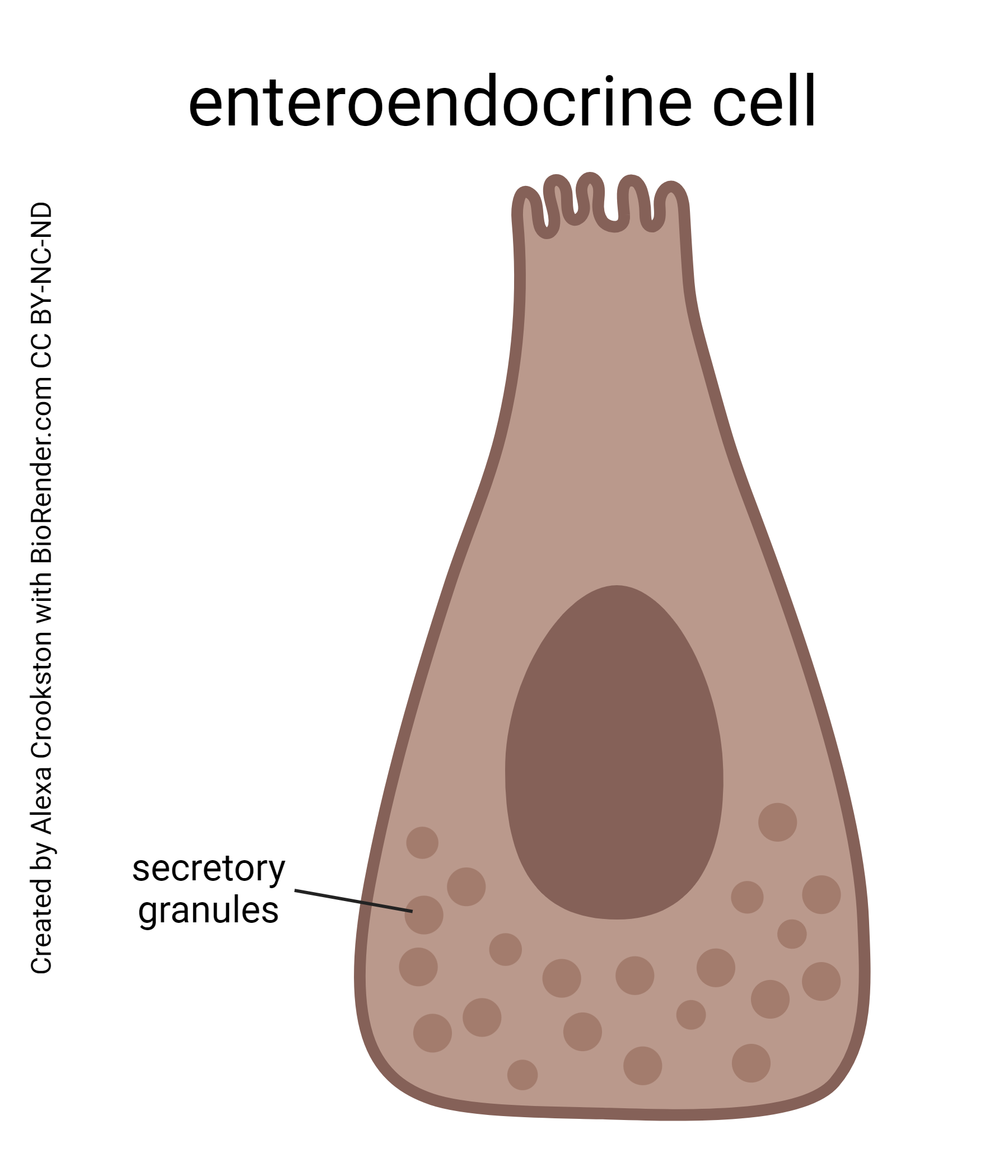 Enteroendocrine cells of the intestine secrete secretin from S cells, cholecystokinin (CCK) from CCK cells, and glucose-dependent insulinotropic peptide (GIP) from K cells. We will discuss more enteroendocrine system secretions as we go through this unit and will have a summary in a later objective.
Enteroendocrine cells of the intestine secrete secretin from S cells, cholecystokinin (CCK) from CCK cells, and glucose-dependent insulinotropic peptide (GIP) from K cells. We will discuss more enteroendocrine system secretions as we go through this unit and will have a summary in a later objective.
All these folds and shag carpets and microscopic fingers are aimed at increasing the surface area of the small intestine. Since the surface is covered with an epithelium of (mostly) absorptive cells, this increased surface area increases the area available for absorption of water and nutrients. The absorptive cells, on the other hand, are covered with protein channels that bring substances from the lumen into the cell by symport systems. These systems carry Na+ and glucose, or Na+ and amino acids, into the intestinal cell at the same time.
If you examine the government-mandated “Nutrition Facts” label on your favorite food, you’ll notice that food contains three major classes of ingredients:
- carbohydrates, including monosaccharides (simple sugars), disaccharides (e.g. sucrose), and polysaccharides (starches)
- fats or lipids
- proteins, polymers of amino acids
Each of these substances has a different route from the gut lumen into the bloodstream.
Starches (amyls) are broken down by amylase into disaccharides. Enzymes break disaccharides into two monosaccharides. For example, sucrose is broken into glucose and fructose by sucrase.
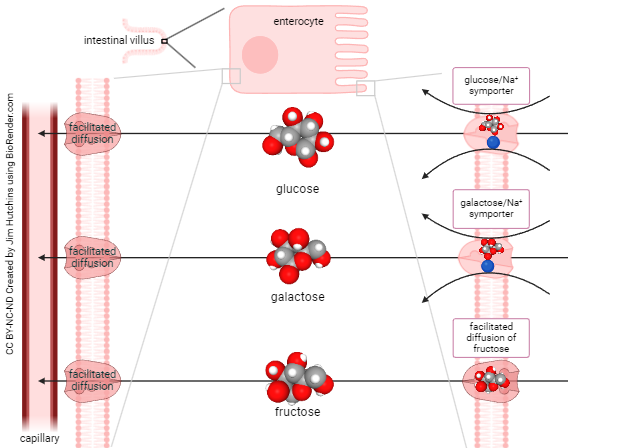
The only monosaccharides absorbed by intestinal cells are glucose, galactose, or fructose. Glucose and galactose are at higher concentrations inside the intestinal cell than in the lumen, so they must be carried into the intestinal cell by secondary active transport (symport). Fructose is always at higher concentration outside the cell (in the lumen) than inside the cell, so it can cross the cell membrane by facilitated diffusion. Once inside the cell, sugars diffuse from areas of higher concentration (inside the absorptive cells of the intestine) to lower concentration (bloodstream) by facilitated diffusion.
Proteins are polymers of amino acids. Examples of enzymes that break down proteins are peptidases or proteases: pepsin, trypsin, chymotrypsin, elastase, aminopeptidases, and dipeptidases.
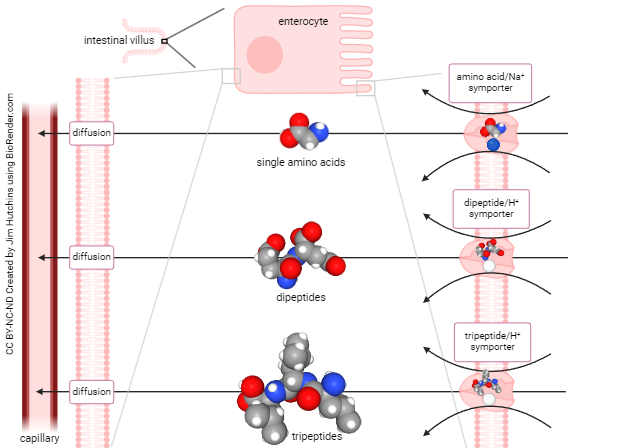
Once the protein is broken into fragments of one, two or three amino acids in length, intestinal cells can absorb the remnants. As shown previously, amino acids are pumped into the absorptive cell by Na+-driven symport. Di– and tripeptides are brought in using a similar H+-driven symport system. Once inside the absorptive cell at high concentration, they diffuse into the villus capillary bed.
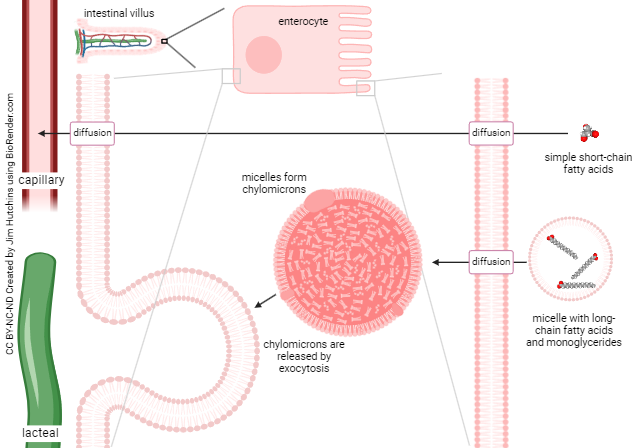
Absorption of lipids is more complex. Short-chain fatty acids are small enough molecules to move across the intestinal absorptive cell membrane, and then into the bloodstream, by simple diffusion.
Other lipids are too large and too water-insoluble to move this way. Rather, they are found in micelles in the gut lumen.
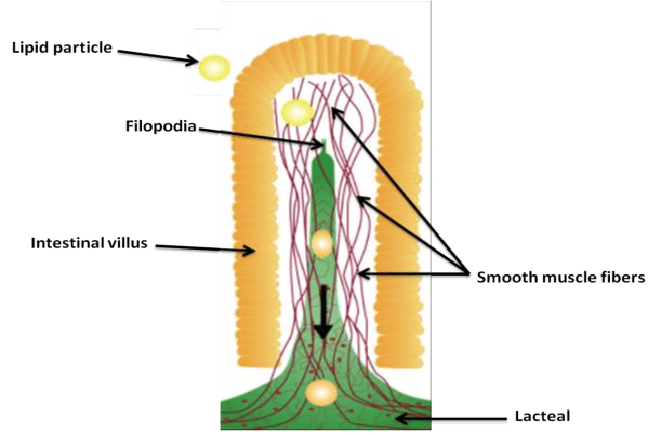 In order for lipids to be fully broken down by enzymes and absorbed by the intestinal absorptive cells, they must be emulsified and formed into triglycerides. This emulsification is the responsibility of bile, which we will discuss later. Triglycerides are further processed into chylomicrons which are pushed out the basolateral surface of the absorptive cell and into a small lymph vessel, the lacteal.
In order for lipids to be fully broken down by enzymes and absorbed by the intestinal absorptive cells, they must be emulsified and formed into triglycerides. This emulsification is the responsibility of bile, which we will discuss later. Triglycerides are further processed into chylomicrons which are pushed out the basolateral surface of the absorptive cell and into a small lymph vessel, the lacteal.
Lacteals carry chylomicrons to the bloodstream, where the lipids can associate with lipoproteins (high-density lipoproteins, or HDL; low-density lipoproteins, or LDL; very low-density lipoproteins, or VLDL). Lipoproteins, as the name implies, are lipid-carrying proteins of the bloodstream. They are synthesized by the liver.
All nutrients end up in the hepatic portal vein (except chylomicrons) on their way to the liver.
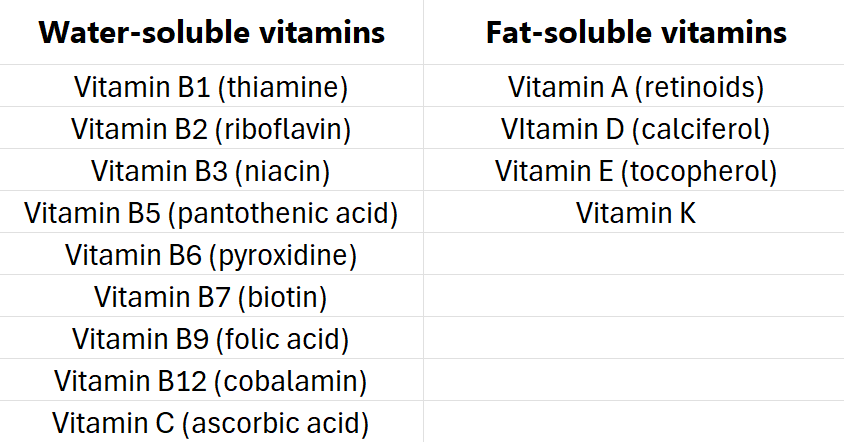
Chemical cofactors called vitamins work to help speed up essential chemical reactions in cells by lowering the activation energy of chemical reactions. Enzymes do the same thing, but are proteins; vitamins are non-protein catalysts.
There are two major categories of vitamins: water-soluble and fat-soluble. Most vitamins are absorbed directly from dietary sources. Some exceptions, relating to GI dysfunction, are discussed here. epatic portal vein (except chylomicrons) on their way to the liver.
In the stomach, parietal cells secrete intrinsic factor, a glycoprotein that helps cells of the intestinal ileum absorb vitamin B12 from the diet. Disruption of normal intrinsic factor production by diseases of the stomach results in pernicious anemia, a macrocytic anemia. In this disease, RBCs are too large and low in number.
Folic acid deficiency also results in pernicious anemia, and a deficiency in pregnant women can increase the chances of neural tube defects (e.g. spina bifida) in their fetuses.
Vitamin K is found naturally in spinach, brussels sprouts, broccoli, cauliflower, and other foods. There are plenty of people who almost retched reading the previous sentence. Those people, whose diets are low in vitamin K, rely on Escherichia coli bacteria in the large intestine to synthesize vitamin K. Vitamin K is essential for blood clotting (acting along with clotting factors II, VII, IX and X).
Media Attributions
- U18-022 GastroIntestinal System © BruceBlaus is licensed under a CC BY (Attribution) license
- U18-023 Circular Folds of the Intestines © Sobotta, Johannes is licensed under a Public Domain license
- U18-024 Small Intestine © Crookston, Alexa is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U18-025 Enterocyte Cell © Crookston, Alexa is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U18-026 Goblet Cell © Crookston, Alexa is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U18-027 Paneth Cell © Crookston, Alexa is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U18-028 Enteroendocrine Cell © Crookston, Alexa is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U18-030 Sugar Absorption by Enterocytes © Hutchins, Jim is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U18-031 Amino Acid Absorption by Enterocytes © Hutchins, Jim is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U18-032 Lipid Absorption by Enterocytes © Hutchins, Jim is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U18-033 Structure of the Intestinal Lymphatic Capillary © Yousef, Malaz is licensed under a CC BY-SA (Attribution ShareAlike) license
- U18-034 Vitamin Table © Hutchins, Jim is licensed under a CC BY-SA (Attribution ShareAlike) license

