Sensory Systems | Auditory (Hearing) System
Objective 5
On a diagram, label the structures of the hearing (auditory) apparatus. Describe the role each structure plays in hearing. Follow the sound conduction pathway from the auricle to the fluids of the inner ear. Explain the coding of pitch and loudness in the auditory system. Describe the path taken by neural information from the auditory receptors to the brain.
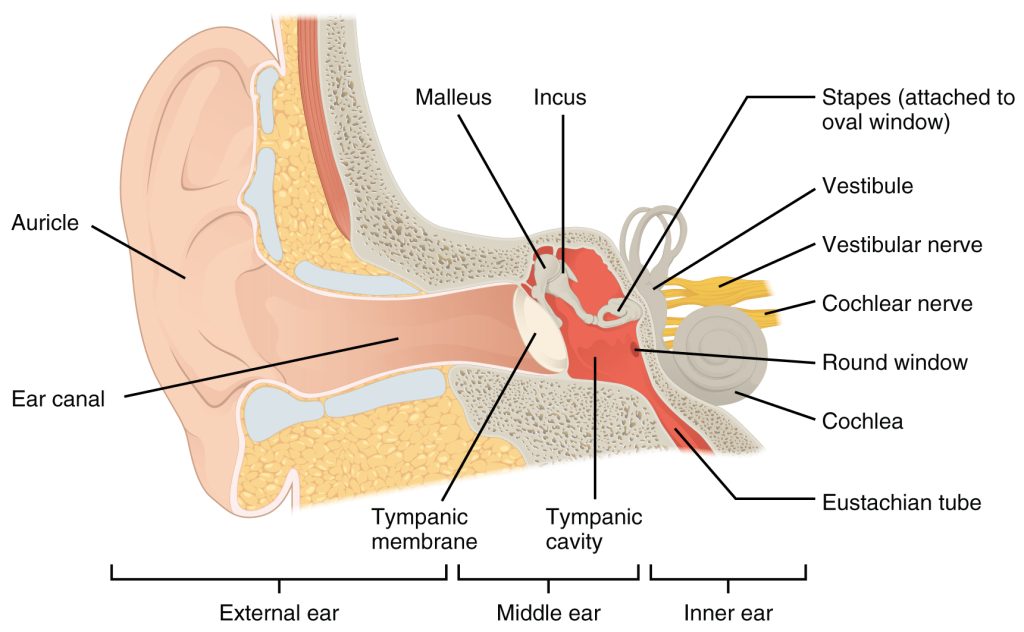
External Ear
The sense of hearing (auditory sense) depends on the ear receiving pressure waves of air. A moving object, such as the vocal cords or the paper cone of a speaker makes regions of increased air pressure alternating with regions of decreased air pressure. These pressure waves of air are the relevant stimulus for the auditory system.
Pressure waves of air arrive at the auricle (or pinna), the external part of the ear, and are carried through the external auditory canal (external auditory meatus) to press against the tympanic membrane (“eardrum”).
The tympanic membrane vibrates as pressure waves of air push against it.
Middle Ear
The special problem of the middle ear is how to get a compressible medium (air) to create pressure waves in an incompressible medium (liquid). To do this, a small amount of energy over a large surface area (the tympanic membrane) is leveraged and focused into a large amount of energy over a small surface area (the oval window). It’s like holding a moving car door open with your finger: a great deal of pressure would be applied to your (now broken) finger in this way. If the ossicles (malleus, incus, stapes) are damaged or surrounded by fluid, the system doesn’t work.
The Eustachian tube (also called the auditory tube) is a tunnel that connects the middle ear to the nasopharynx. This equalizes the pressure on both sides of the tympanic membrane unless the tube becomes swollen or clogged with mucus. If the tube is not patent (open), then pressure builds and causes pain in the ear. This happens, for example, as the pressure changes on an airplane. Moving the jaw, chewing gum or pinching the nose and blowing air against closed lips are all maneuvers to open the auditory tube and restore the pressure balance.
Inner Ear
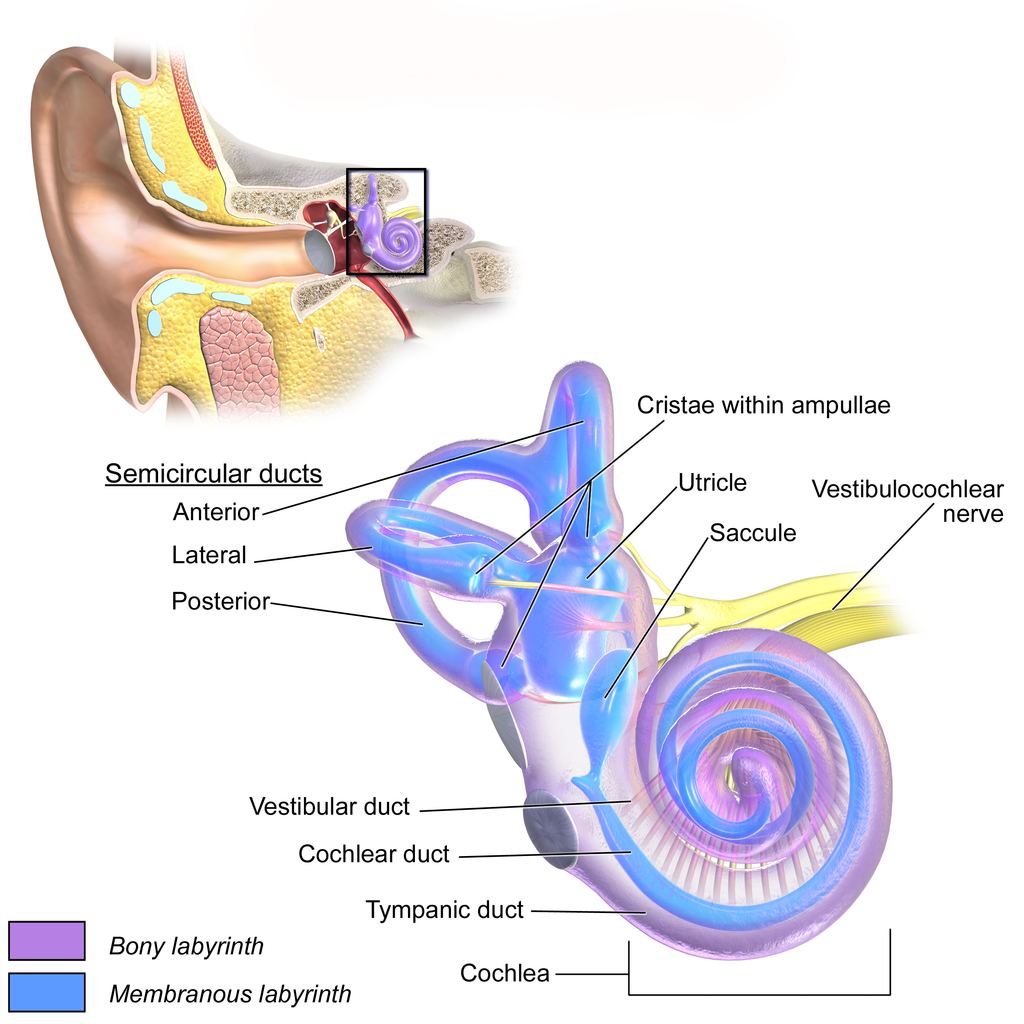
Within the inner ear, there are two different structures with two different functions. The semicircular canals and vestibular apparatus are used for balance, and will be discussed later. We’ll focus for now on the cochlea (Latin: “snail”), a spiral-shaped structure which contains the spiral organ (organ of Corti), the transduction apparatus for hearing.
The cochlea is named for its spiral appearance, like a snail’s shell. It completes 2½ turns. High frequency sounds are represented near the oval window, where the pressure wave of fluid is created. Low frequency sounds are represented near the center of the spiral. We’ll talk about how frequency (pitch) is related to location in the cochlea as we look at the details of this system.
There are three chambers in the cochlea. The oval window is the wall of the vestibular duct (scala vestibuli) which is filled with a fluid called perilymph. The vestibular duct is a spiral tunnel that extends from the round window to the center of the spiral, a point called the helicotrema. At the helicotrema, the vestibular duct is continuous with the tympanic duct (scala tympani). Because these chambers connect, they have the same fluid, the perilymph mentioned earlier.
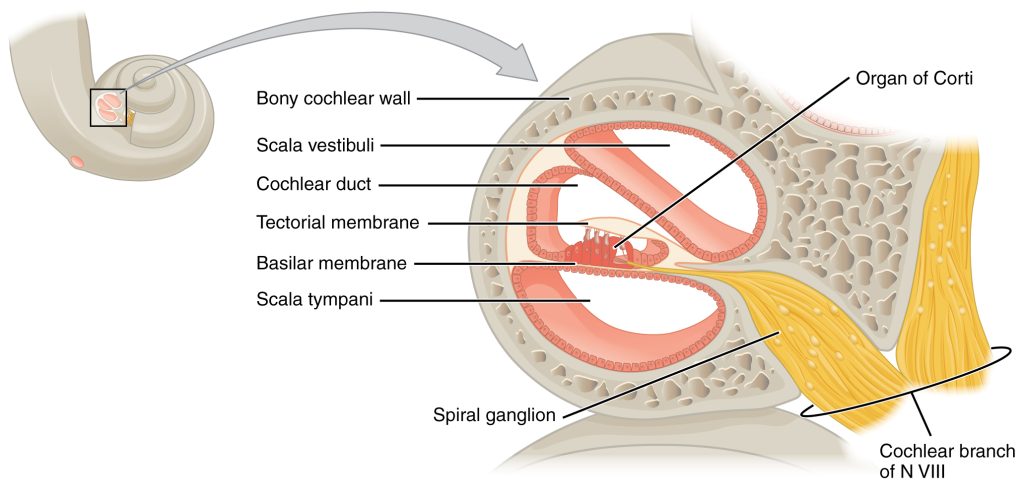
Sandwiched between these two spiral tubes of perilymph is a third tube, shaped like a piece of pie in cross-section, called the cochlear duct.
The cochlear duct contains a special fluid called endolymph. The composition of endolymph is important for the functioning of the cochlea, but we won’t look at it detail other than to mention that disease processes can disrupt hearing and balance by altering the composition of this fluid (as in Ménière disease).
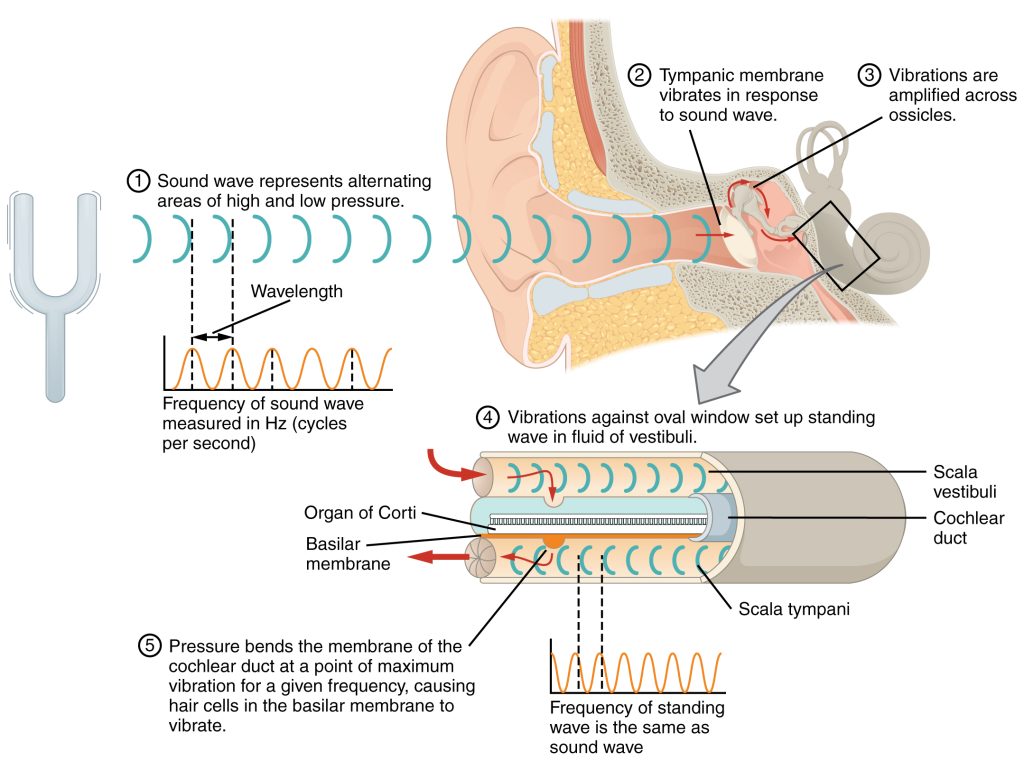
The spiral organ is sandwiched between two fluid-filled chambers. The fluid in these spaces is moved when energy is transferred from the tympanic membrane to the ossicles to the oval window to the vestibular duct to the tympanic duct to the basilar membrane.
As the fluid sloshes about, the basilar membrane of the spiral organ is pushed up and down in waves. These waves match the frequency of the pressure waves of air that reached the ear. As the basilar membrane bobs up and down, the modified cilia (hairs) of mechanoreceptor cells (hair cells) are bent back and forth in the tectorial membrane.
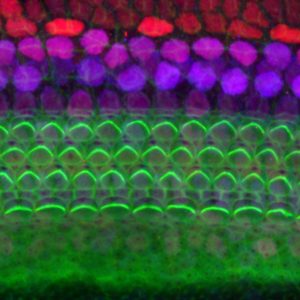
The mechanoreceptors in the organ of Corti are called hair cells. In a single section of the spiral organ, there are usually three outer hair cells and one inner hair cell.
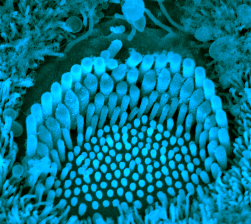 A single hair cell is seen from above in the aqua-tinted image (the original scanning electron micrograph was black and white). In this image, we can see what give the hair cells their name: the presence of a few dozen hairs, modified cilia on the apical surface of the hair cell. The base of each hair cell sits on the basilar membrane of the organ of Corti, hence the name “basilar”.
A single hair cell is seen from above in the aqua-tinted image (the original scanning electron micrograph was black and white). In this image, we can see what give the hair cells their name: the presence of a few dozen hairs, modified cilia on the apical surface of the hair cell. The base of each hair cell sits on the basilar membrane of the organ of Corti, hence the name “basilar”.
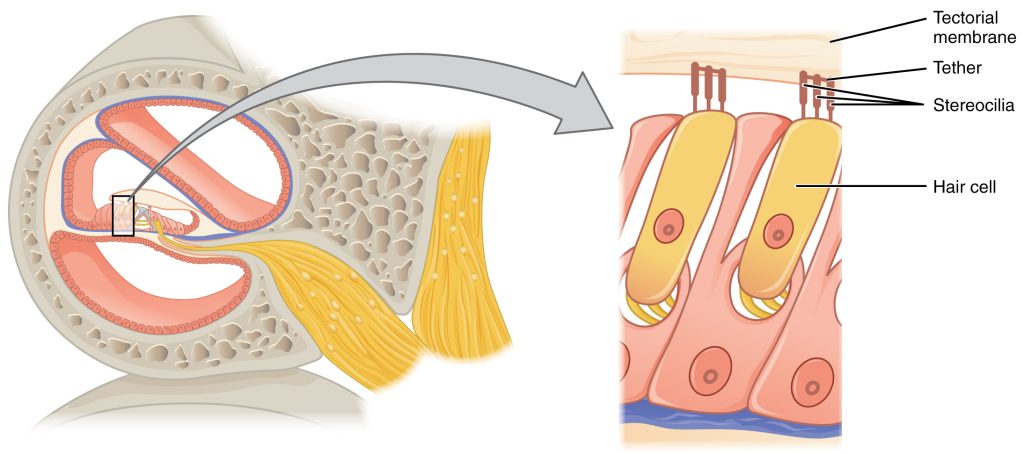
The base of each hair cell sits on the relatively floppy basilar membrane. The hairs (stereocilia, literally, “non-motile hairs”) at the apical end touch the relatively stiff tectorial membrane. In this way, the hairs are moved when the basilar membrane moves and the hairs get bent or “squeezed” between these two membranes. Tethers connect the stereocilia together, and make sure the stereocilia move as a bundle. The mechanoreceptor proteins at the stereocilia tips allow ions to leak in when the stereocilia tethers pull on the membrane surrounding each stereocilium.
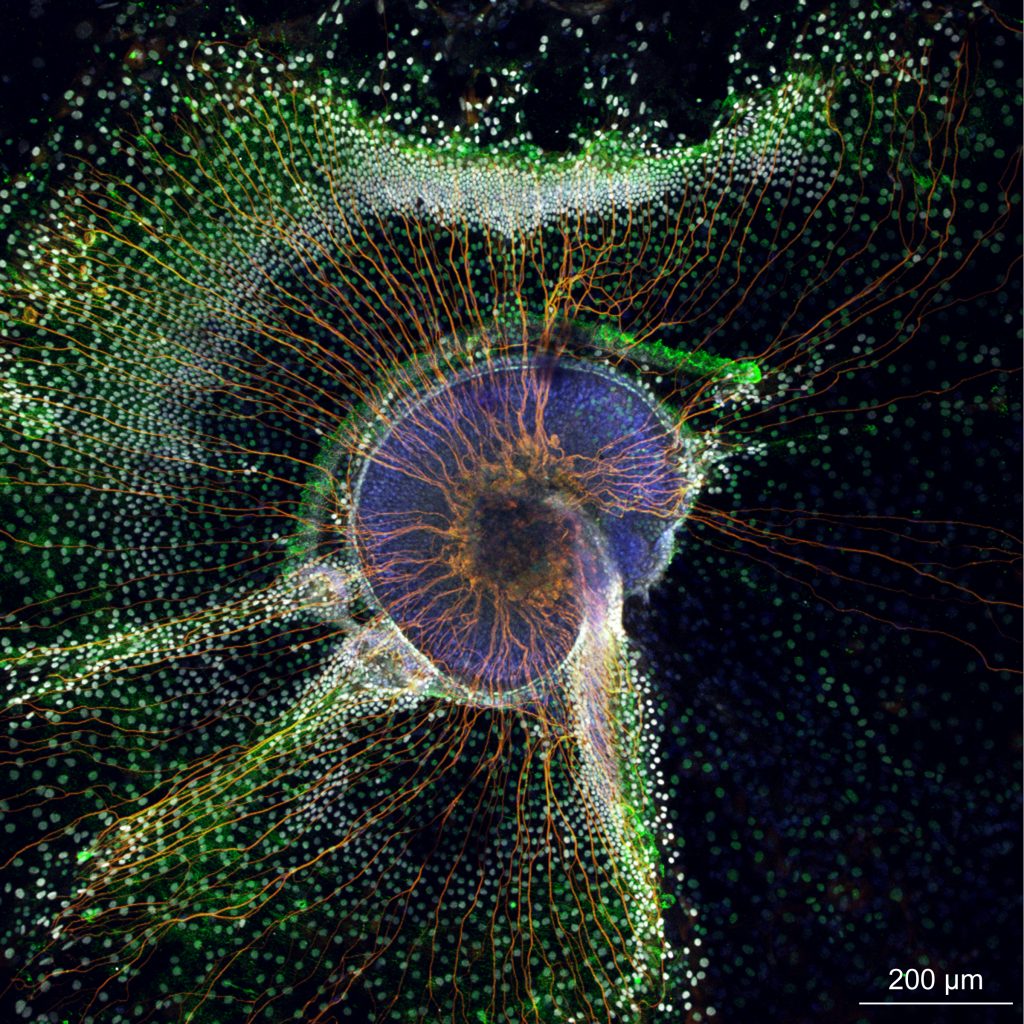 The hair cells are small and don’t send their information far. They make contact on the dendrites of an afferent fiber. The primary afferent is a bipolar cell with dendrites in the organ of Corti, a cell body in the spiral ganglion and an axon that travels in the cochlear branch of the vestibulocochlear nerve (CN VIII).
The hair cells are small and don’t send their information far. They make contact on the dendrites of an afferent fiber. The primary afferent is a bipolar cell with dendrites in the organ of Corti, a cell body in the spiral ganglion and an axon that travels in the cochlear branch of the vestibulocochlear nerve (CN VIII).
Auditory pathways from the cochlear division of the vestibulocochlear nerve to the brain are incredibly complicated and will be discussed only briefly here.
Calculation of Sound Location
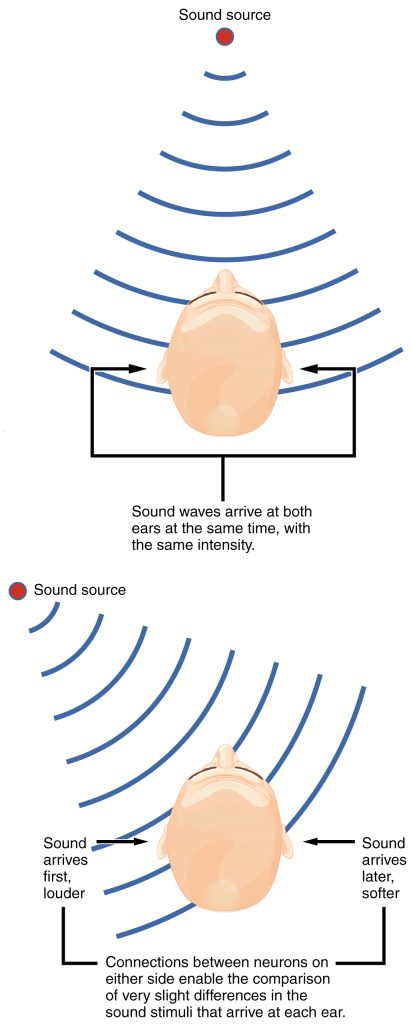
Surprisingly, the only place in the brain that calculates the location of sounds is the superior olivary nucleus (superior olive), in the medulla where microsecond (millionth of a second!) differences in the arrival of sound between the two ears are used to determine the source of sounds.
Auditory Cortex
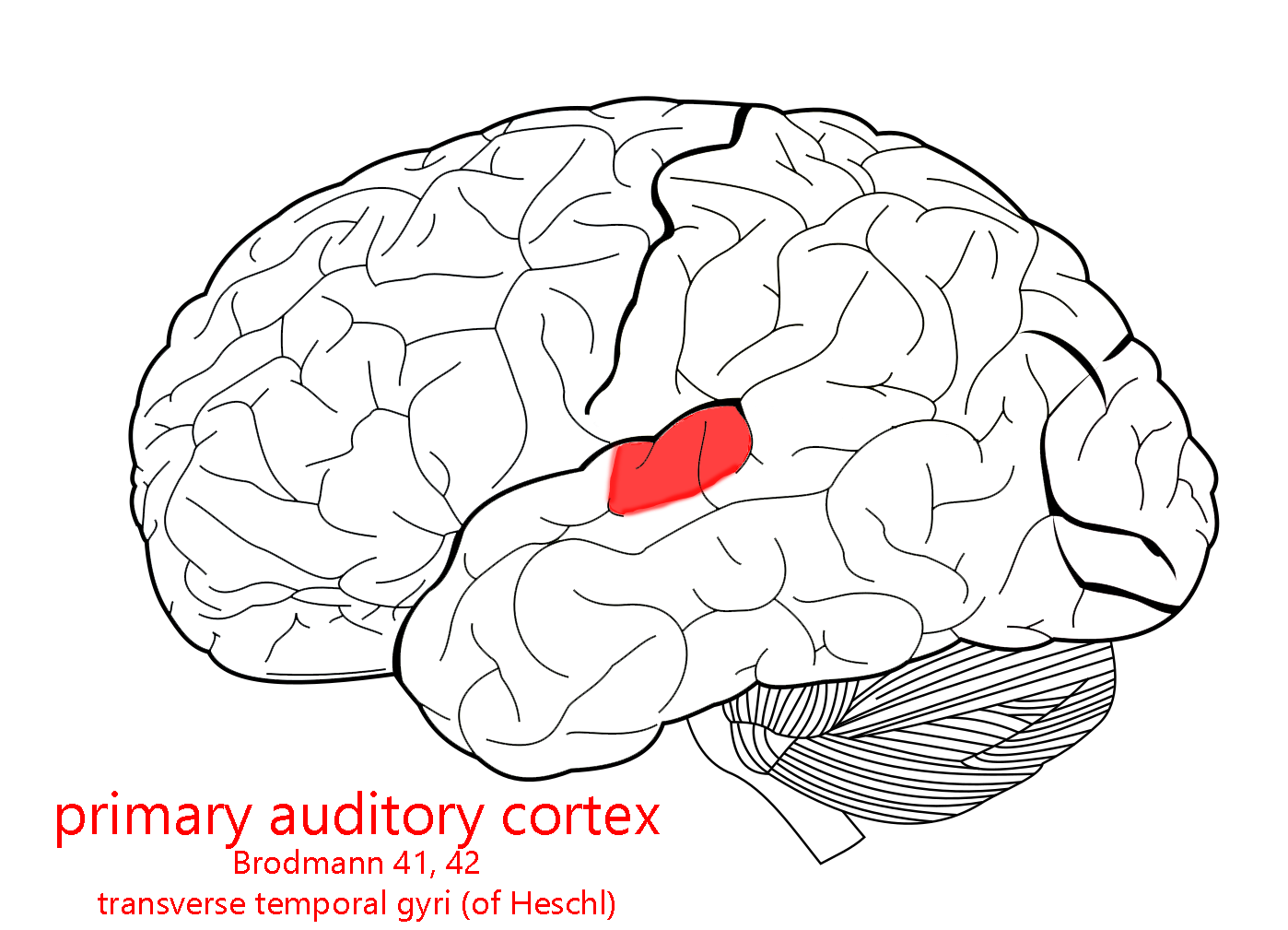
The auditory cortex is in the temporal lobe. Primary auditory cortex (A1) is identical to Brodmann’s areas 41 and 42, in the superior part of the temporal lobe. (Though it’s too detailed for us at this level, there are gyri tucked inside the lateral fissure which run perpendicular to the superior temporal gyrus; these are called the transverse temporal gyri of Heschl and that’s the exact anatomical location of A1.)
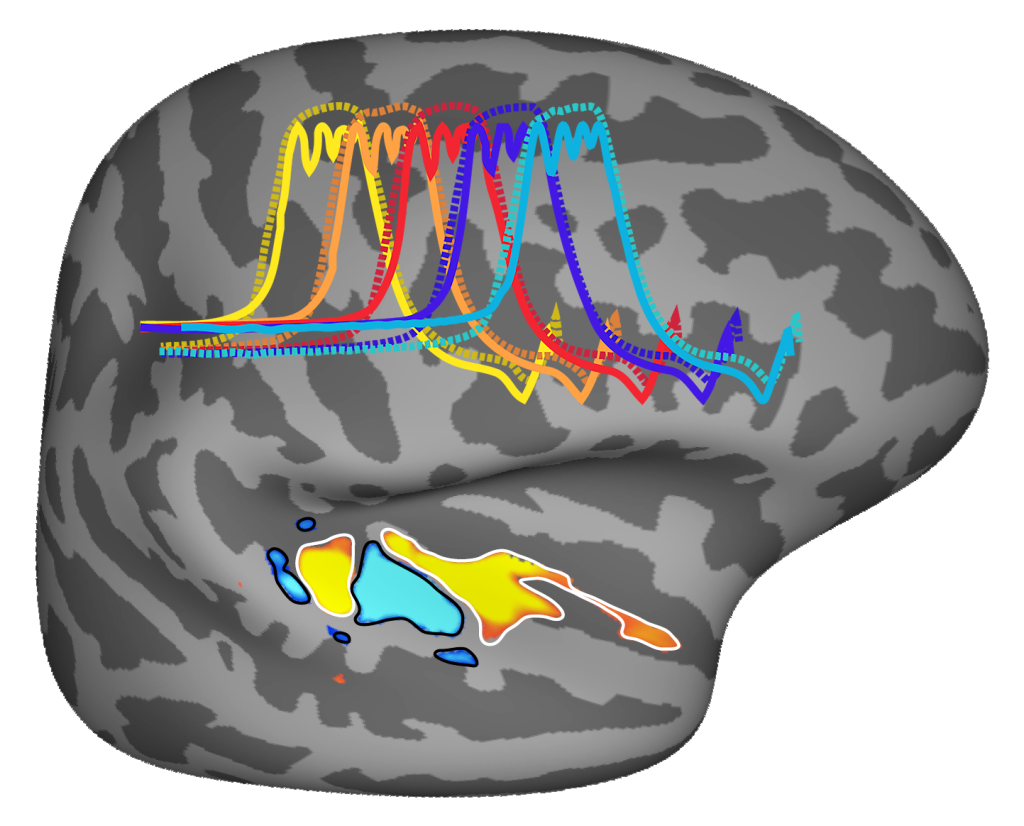 Throughout the auditory system, the “map” is based on tones and not on the location of the sound source. For this reason, the orderly map of auditory space in auditory cortex is called a tonotopic (“sound place”) map.
Throughout the auditory system, the “map” is based on tones and not on the location of the sound source. For this reason, the orderly map of auditory space in auditory cortex is called a tonotopic (“sound place”) map.
Media Attributions
- U12-047 Auditory © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U12-048 EarAnatomy_InternalEar © BruceBlaus is licensed under a CC BY (Attribution) license
- U12-049 Auditory Cochlea © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U12-050 Auditory Transduction © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U12-051 Cochlea Mouse © Driver, Elizabeth Carroll Ph.D., National Institute on Deafness and Other Communication Disorders, , NIH is licensed under a Public Domain license
- U12-052 Hair Cells Mouse © Kawashima, Yoshiyuki NIDCD is licensed under a CC BY-NC (Attribution NonCommercial) license
- U12-053 Auditory Hair Cell Cochlea © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U12-054 Mouse Cochlea Tissue Culture © Jan, Taha A. M.D., and Scheibinge, Mirkor, Ph.D., Marine Biological Laboratory at Wood’s Hole, Biology of the Inner Ear Course is licensed under a CC BY-NC (Attribution NonCommercial) license
- U12-055 Auditory Sound Localization © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U11-084 Auditory Cortex © Carter, Henry Vandyke adapted by Jim Hutchins is licensed under a CC BY-SA (Attribution ShareAlike) license
- U12-058 Human Brain Pitch Regions © NIH is licensed under a Public Domain license

