Red Blood Cells
Objective 3
Describe the structure and function of the red blood cells (RBCs). Identify the components of the hemoglobin molecule and describe its function. Identify the ABO and Rh antigens that may be present on red blood cells and describe their inheritance and corresponding antibody development.
 The primary function of red blood cells is to transport oxygen. Their unique characteristics enable them to do this with remarkable efficiency. Among these characteristics is their biconcave shape, their reversible deformity, their lack of a nucleus, and the fact that they do not consume the oxygen they carry.
The primary function of red blood cells is to transport oxygen. Their unique characteristics enable them to do this with remarkable efficiency. Among these characteristics is their biconcave shape, their reversible deformity, their lack of a nucleus, and the fact that they do not consume the oxygen they carry.
Their biconcave shape gives them a high surface-to-volume ratio, thus allowing them to carry a great deal of oxygen in relation to their size. Think of this shape as a donut, but the hole in the middle doesn’t go all the way through.
RBCs are required to squeeze through really small spaces, specifically blood capillaries. As they pass through these small spaces, they become almost torpedo-like, but when they come out the other side, they revert back to their biconcave shape. The ability to change shape like this is called reversible deformity.
Red blood cells lack mitochondria, so they don’t produce ATP by oxidative metabolism. Instead, they utilize glycolysis to stay alive. By so doing, they use glucose for energy, but they transport all of the oxygen they pick up.
Because a RBC lacks a nucleus, it allows all of the cytoplasmic space to carry oxygen. Before the nucleus is lost, it provides the instructions to produce hemoglobin, the oxygen-carrying molecule of the red cell. A mature red blood cell is like a membrane bound bag of hemoglobin.
Red blood cells live for approximately 120 days. This isn’t too bad due to the fact that they are constantly damaged from squeezing through small spaces, and they don’t have a nucleus or any organelles to repair the damage that takes place. Once the damage has rendered the cells dysfunctional, they are removed from the circulation by phagocytic white blood cells, the spleen, and the liver.
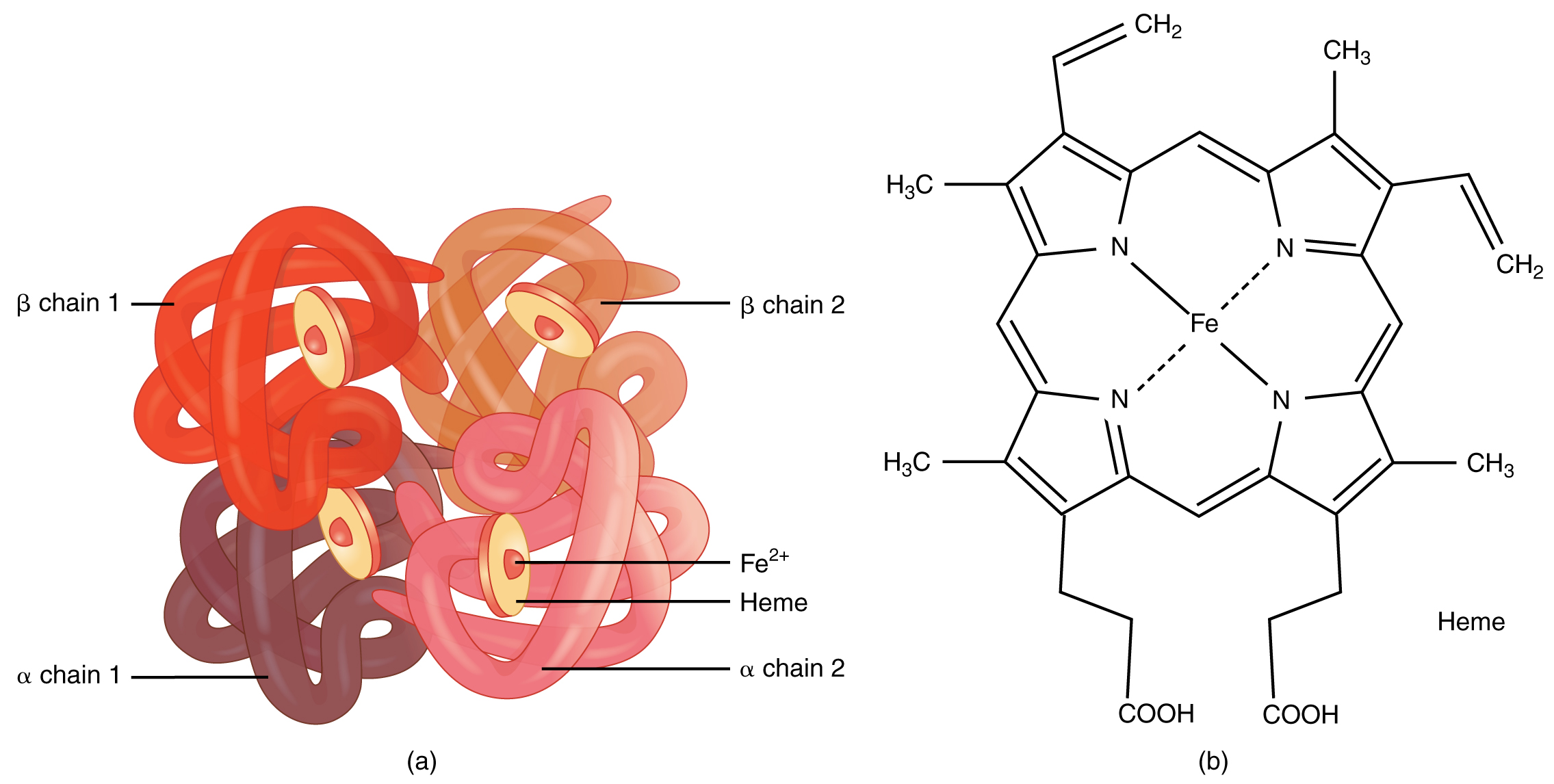
As previously mentioned, hemoglobin is the oxygen-carrying molecule of the red blood cell. There are approximately 280 million hemoglobin molecules in each red cell. One hemoglobin molecule consists of two main components, heme and globin. Globin is a protein that is made up of four-polypeptide chains, two alpha chains and two beta chains. Each polypeptide chain has a heme molecule bound to it. Heme is a ringed molecule with one iron (Fe2+) atom at the center. The iron atom is the binding site for oxygen; each Fe2+ can pick up one oxygen molecule (O2) at the lungs. So, if there are 280 million hemoglobin molecules in a red cell and each hemoglobin molecule has four hemes, and each heme can pick up one oxygen molecule, one red cell can carry 1.1 billion oxygen molecules. The concentration of hemoglobin in the blood ranges from 14-16 g/dl.
At the lungs, hemoglobin has a high affinity, or attraction to oxygen; it wants to pick it up and hold on to it. At the tissue level, hemoglobin has a lower affinity for oxygen. Hemoglobin wants to let go of oxygen, thereby allowing it to diffuse into the cells. It doesn’t do any good to pick up oxygen and just hold on to it in the blood. This affinity for oxygen can increase or decrease based on the body’s needs. Hemoglobin also picks up a little bit of CO2 from the tissues to transport back to the lungs and be exhaled.
Red blood cells, like all other cells, contain genetically-determined cellular markers. These markers constitute a cell’s signature. Through this signature, cells can be identified. A person inherits genes from their parents that dictate which markers will appear on their cells, in this case specifically red blood cells. Many groups of RBC markers exist, and they all seem to have strange names like Kidd, Kell, Duffy, Lewis, M, I, S etc. We will only look at the ABO and Rh blood group systems as they are the most important.
When a person is blood typed, their cells are evaluated for the presence or absence of specific markers. These markers, because they can react with products of the immune system, are called antigens. The immune system can make specific antibodies to these antigens.
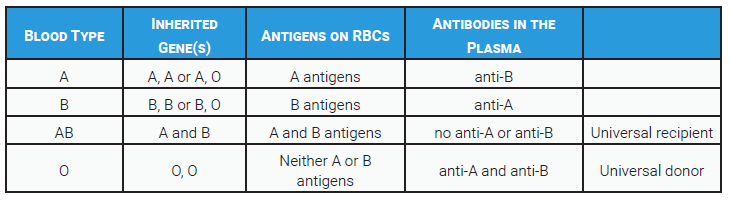
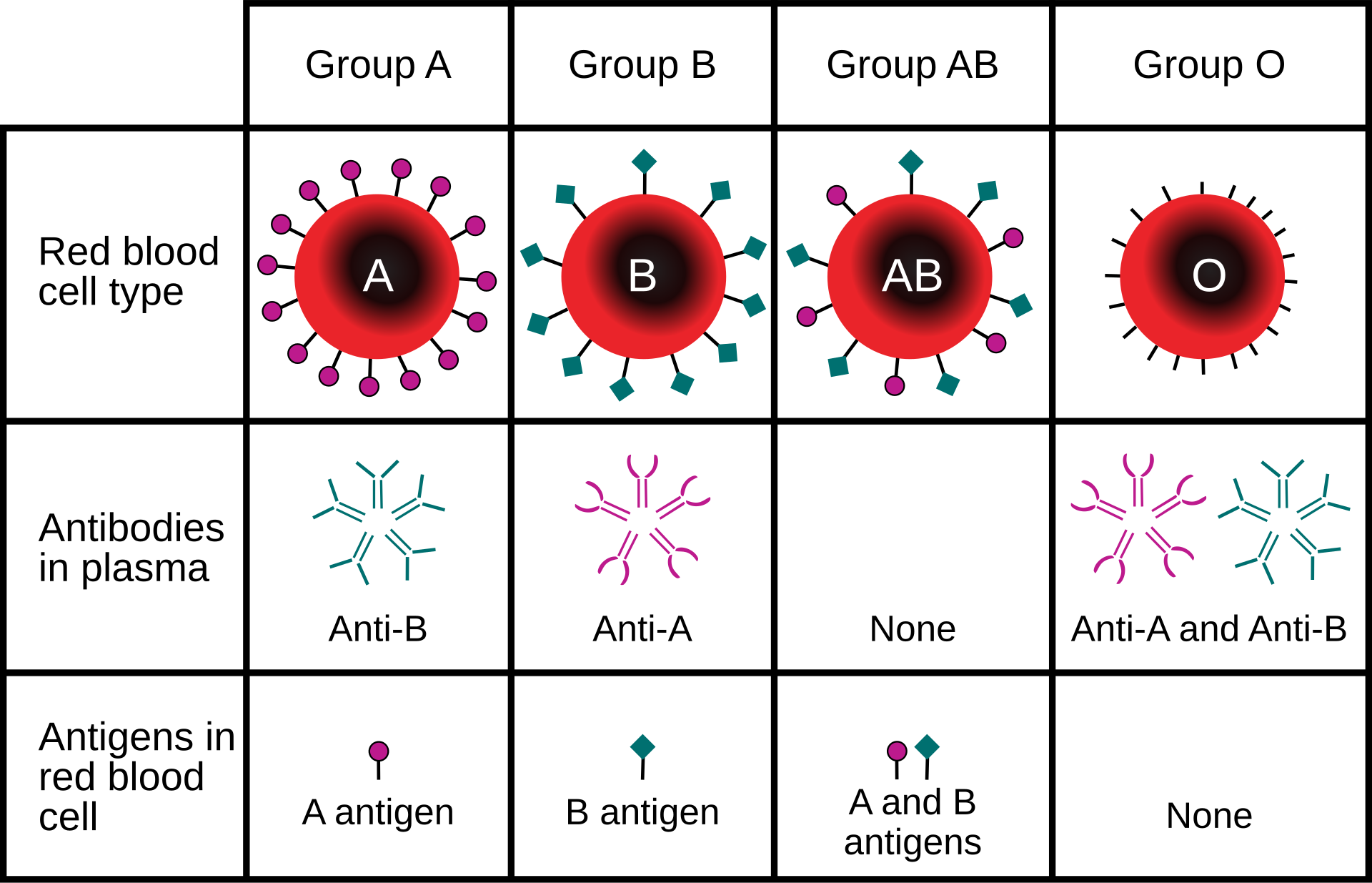
The ABO blood group is the most important blood group system to consider. A person’s ABO blood type is based on the presence or absence of A and B antigens on their red cells, due to the inheritance of certain genes. Both father and mother will pass an ABO blood-type gene to their offspring.
 The choices are A, B, or O. If a person inherits the A gene from at least one parent, they will have A antigens on their cells. If they inherit the B gene from at least one parent, they will have B antigens on their cells. If they inherit both genes, one from each parent, they will have both A and B antigens on their cells. If an individual does not inherit either the A or B gene, they will be identified as having the O blood type and will have no A or B antigens on the red blood cell surface.
The choices are A, B, or O. If a person inherits the A gene from at least one parent, they will have A antigens on their cells. If they inherit the B gene from at least one parent, they will have B antigens on their cells. If they inherit both genes, one from each parent, they will have both A and B antigens on their cells. If an individual does not inherit either the A or B gene, they will be identified as having the O blood type and will have no A or B antigens on the red blood cell surface.
This occurs because the A and B genes are dominant genes. That means a person will demonstrate the antigens on their cells if they inherit the genes. So, the possible blood types within the ABO group are: A, B, AB, and O.
To make things a little more confusing, a person will have antibodies in their plasma that target the antigen they don’t have. So, if a person lacks the A antigen on their cells, they will have anti-A antibodies in their plasma. A lack of B antigens will result in the presence of anti-B antibodies in their plasma. A person with the O blood type lacks both antigens, so they will have both anti-A and anti-B antibodies in their plasma. This is why a person’s blood type must be considered when a patient needs a blood transfusion. If type-A blood is given to a type-B person, the anti-A antibodies the recipient has will flag the transfused red cells for destruction by the immune system. O type blood lacks antigens, so there is nothing for a recipient’s antibodies to attack. That is why it is referred to as the universal donor. Type AB individuals have both antigens on their red blood cells and therefore do not make antibodies to either. For this reason they are considered the universal recipient.
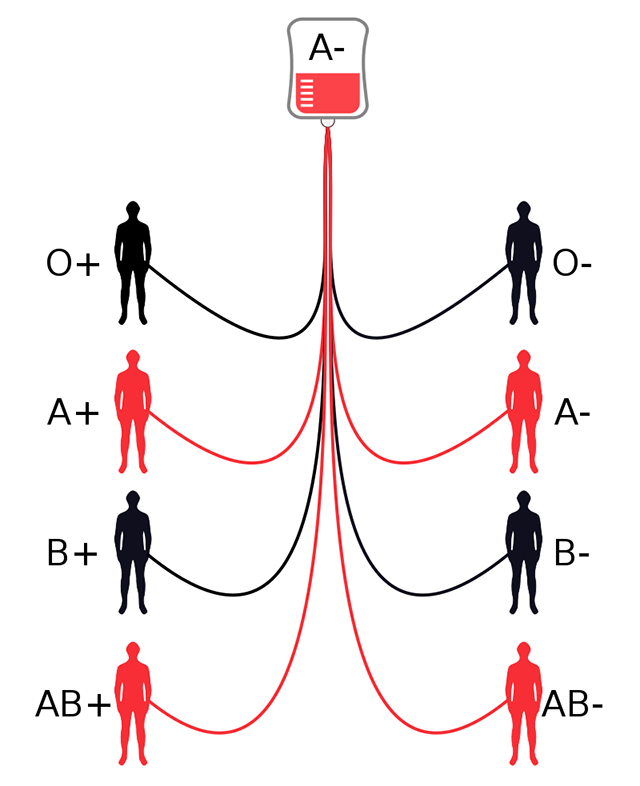
 The Rh blood type is a little easier to understand. It is determined simply by the presence or absence of the Rh antigen on red cells. If a person inherits the dominant Rh gene from either parent, they will have the antigen, so they are Rh positive. If they don’t inherit it, they will be Rh negative.
The Rh blood type is a little easier to understand. It is determined simply by the presence or absence of the Rh antigen on red cells. If a person inherits the dominant Rh gene from either parent, they will have the antigen, so they are Rh positive. If they don’t inherit it, they will be Rh negative.
Another important aspect of this system is that individuals don’t make antibodies to the Rh antigen unless the immune system sees it. So, unless an Rh negative person is exposed to Rh positive blood, they will not have any Rh antibodies.
Media Attributions
- U15-009 Red Blood Cells © SciTechTrend.com is licensed under a Public Domain license
- U15-010 Hemoglobin © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U15-011 Shipping Blood, Saving Lives © Tech. Sgt. James Hodgman is licensed under a Public Domain license
- U15-012 A- Transfusion Compatibility Diagram © KCVelaga is licensed under a CC BY-SA (Attribution ShareAlike) license
- U15-013 Blood Group Antigen Antibody Table © Price, Travis and Newton, Kathy is licensed under a CC BY-SA (Attribution ShareAlike) license
- U15-014 ABO Blood Type © InvictaHOG is licensed under a Public Domain license

