Puberty and Sexual Response
Objective 12
Describe the role of the endocrine system and other factors in male and female puberty. Compare and contrast the male and female sexual response.
Puberty
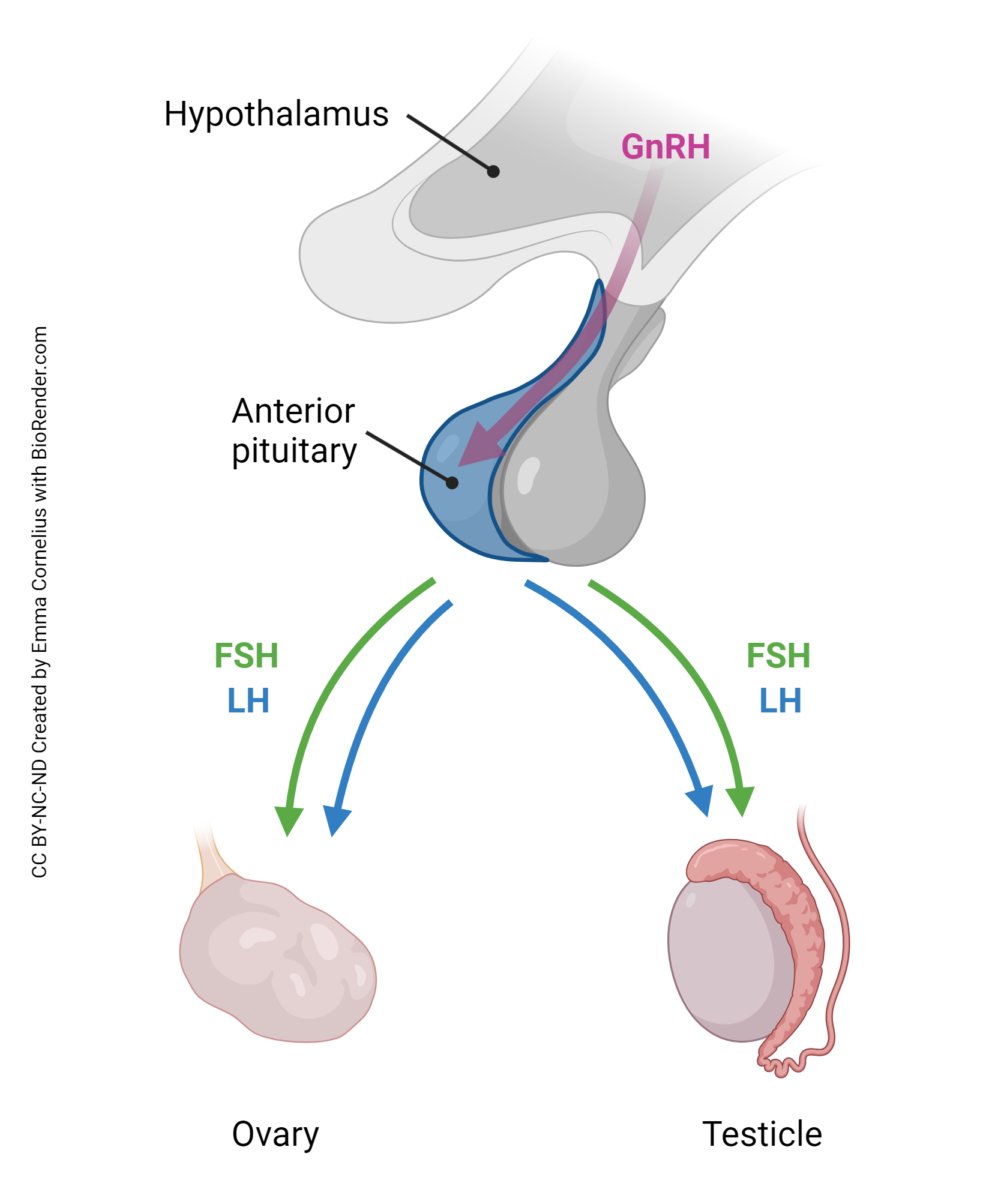
The endocrine system plays a key role, but by no means the only role, in triggering puberty. At the onset of puberty, a number of factors combine to cause a burst of gonadotropin releasing hormone (GnRH) from the hypothalamus. GnRH causes release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary. FSH and LH, in turn, “switch on” gamete production. In males, spermatogenesis begins; in females, menstrual periods begin, the first of which is called menarche.
In both genders, puberty is also marked by the development of secondary sexual characteristics. Primary sexual characteristics are what differentiate little boys (penis, testes, scrotum, associated glands) from little girls (vulva, ovaries, uterine tubes, uterus, vagina, associated glands). In short, primary sexual characteristics can be visualized at birth and define biological gender.
Secondary sexual characteristics are those that differentiate little boys from men and little girls from women. They are gender-related but not necessarily gender-specific. For example, males are generally more muscular and have deeper voices than do females, but these things do not make a person “male.” In other words, there are some women who are more muscular and have a deeper voice than some men.
Male secondary sexual characteristics include body hair (face, chest, pubic, axillary, arms, legs), deeper voice, more prominent thyroid cartilage (Adam’s apple), more muscular, and larger stature.
Female secondary sexual characteristics include body hair (pubic, axillary, arms, legs), higher voice, larger breasts, and wider hips.
Androgens and estrogens also alter the structure of the brain. It’s no secret that men and women tend to think differently, although this wasn’t supported scientifically until the late 1990s, when a landmark study showed clearly that male and female brains are different both structurally and physiologically.
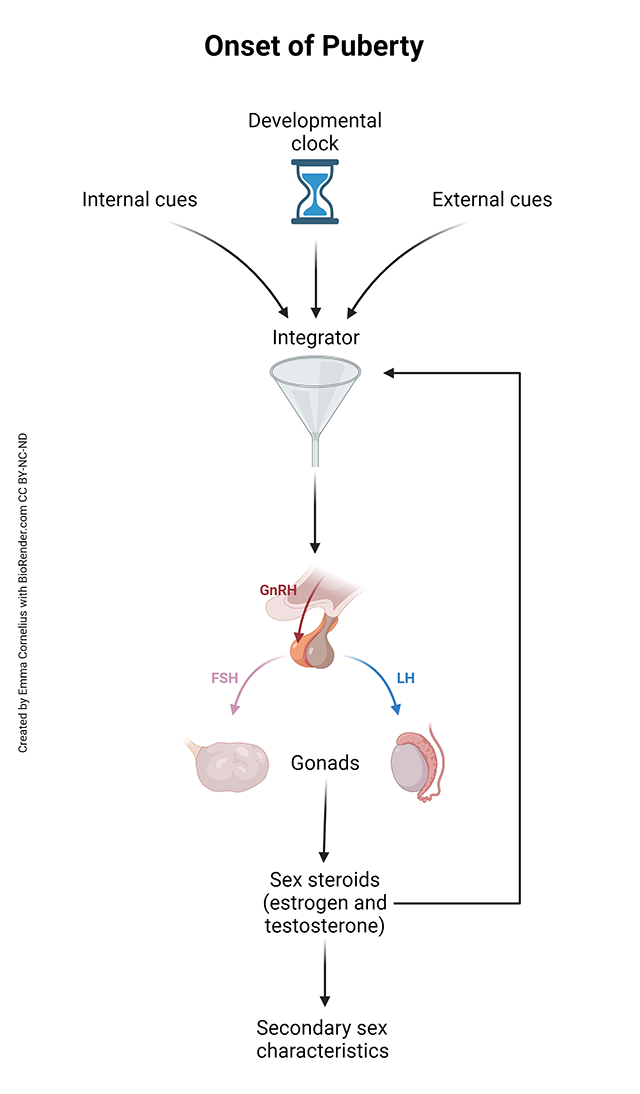
Puberty is a cataclysmic event. The brain is changing, the body is changing, and interpersonal relationships are changing. It’s true that an internal developmental clock participates in the process, but scientists have also shown that internal cues and external cues have an effect as well. Sex steroids act on the brain to alter behavior, and other neurotransmitter systems change as well.
Internal cues, external cues, and input from the internal developmental clock are all fed into an “integrator,” a sort of funnel that collects the disparate sources of information. If/when the integrator reaches a predetermined set-point, it directs the hypothalamus to ramp up GnRH synthesis. Unfortunately, we don’t know what functions as the integrator, we don’t understand the internal developmental clock, the internal cues, the external cues, or how much weight each of them carries, and we don’t know the predetermined set-point.
Remember that menarche is the term for the beginning of menstrual flow in a female. The cessation of ovulation (and, therefore, cessation of monthly menstrual cycles) is called menopause. Menarche is a relatively sudden event; it is usually apparent within a single menstrual cycle. On the other hand, menopause is a gradual process that takes many years to develop. Typically, at the beginning of menopause, ovulation becomes more and more erratic until it finally ceases. As the ovarian cycle becomes more unreliable, the characteristic hormonal changes of the ovarian cycle also begin varying more, and hormonal fluctuations occur that cause the characteristic symptoms of menopause.
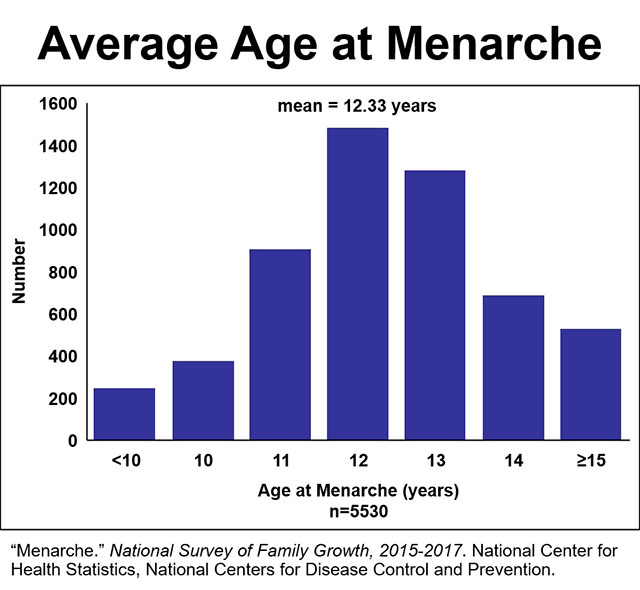
The data represented in the Average Age at Menarche image refers to 5530 US women who participated in the 2015-2017 National Survey of Family Growth, conducted biennially by the National Center for Health Statistics. It represents the average age of menarche across all female participants. In actuality, age of menarche and age of menopause both vary significantly based on family genetics, race, ethnicity, geographical region, nutrition, and other factors.
Clinical Connection: Decreasing Average Age at Menarche
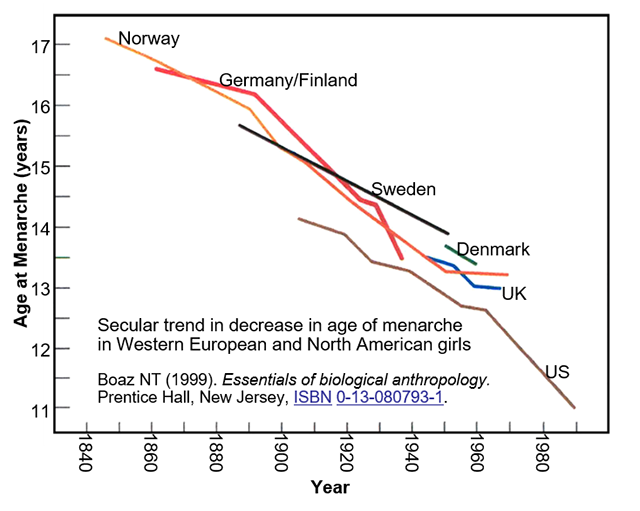
One troubling fact is that data indicates the average age at menarche is dropping. One study of Western European and North American girls shows a six-year decrease, from 17 years old to 11 years old, in average age at menarche over a 150-year period, from 1840 to 1990. The same study shows a three-year two-month decrease in US girls over a 90-year period from 1900 through 1990. These large decreases are almost certainly due to improved nutrition and general health status over those time periods.
Another study shows an eight-month decrease over the 20-year period from the 1960s through the 1980s. The causes for this more recent decrease are much less clear. It is likely that several of the factors already mentioned are responsible for this more recent change: internal cues, external cues, even increased obesity. Adipose tissue acts as an endocrine organ and, therefore, childhood obesity may alter the developmental clock. In fact, solid research has shown a strong correlation between increased BMI and decreasing age at menarche.
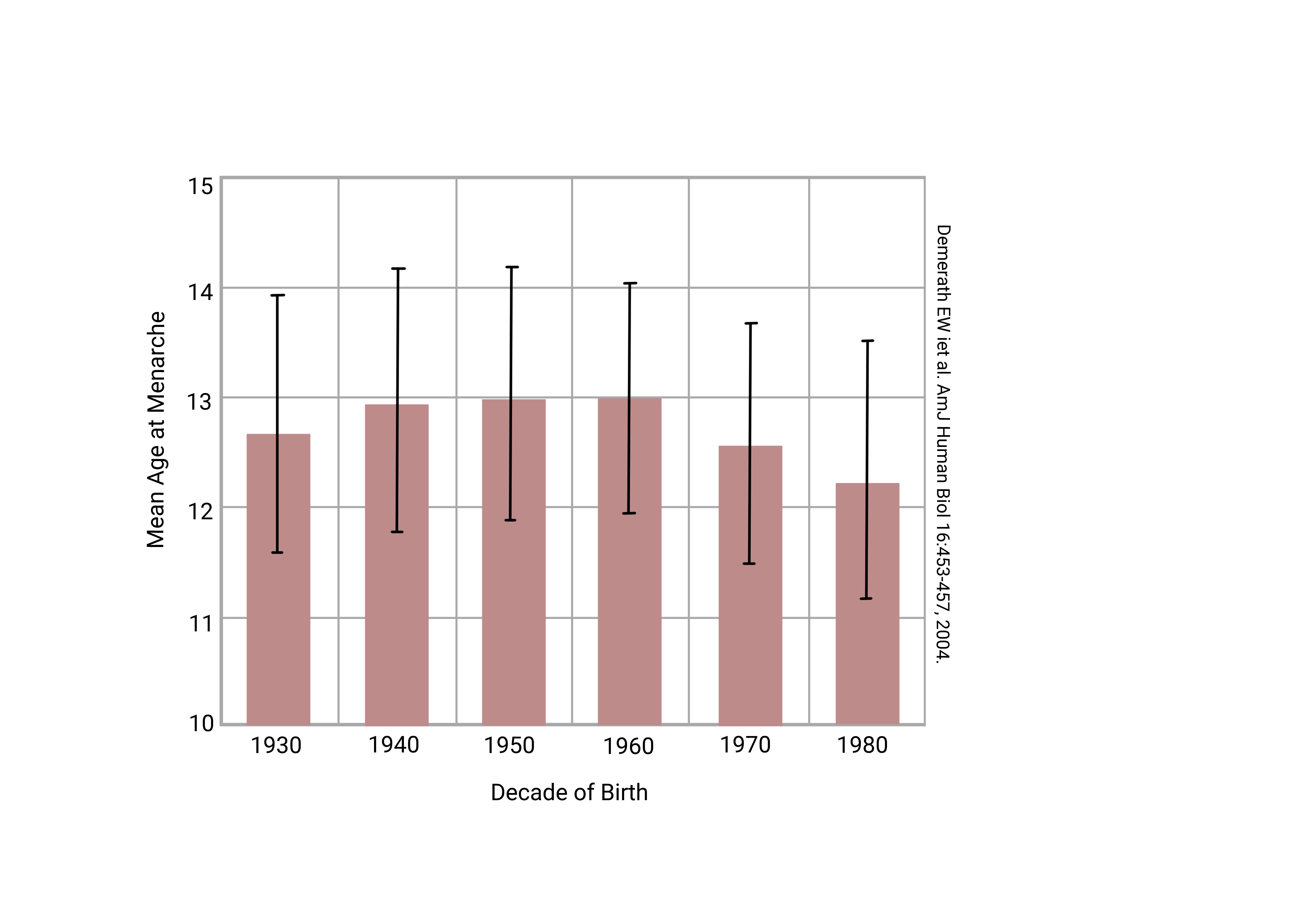
At this time, the average age of menarche about 12 years of age. Just a generation ago, the average age of menarche was almost a year later. That doesn’t sound like a very big change until you consider that not every young woman goes through menarche at the “average” age. The standard deviation is about 1½ years. That means in your parents’ generation, about 30% of girls underwent menarche before 10½ years of age. Now, that 30% of girls who lie more than one standard deviation below the mean are perhaps age 9½ or younger. It was rare for your parents to see a sanitary napkin dispenser in an elementary school girls’ restroom. It is not rare today.
The most worrying aspect of this phenomenon is that we have no idea what’s causing it. We already mentioned the correlation with childhood obesity. Various authors have also suggested hormone residuals in meat and milk as the cause. Others blame increasing harmful environmental exposures. Still others point a finger at representations of sexual behavior in the mass media. As you review the drivers of puberty, you can see evidence for each of these points of view. It is quite possible that all are at least partially involved, as well as other things of which we are not yet aware.
Sexual Response
The study of the anatomy and physiology of human sexual response has a short history. It was only with the landmark research of Kinsey, Pomeroy, and Martin (1948) that it even began as a field of research. In the 1960s, William Masters and Virginia Johnson, first collaborators and later husband and wife, advanced the field greatly.
Some of the difficulties inherent in this field of study are obvious; others, not so much. For example, studying male sexual response is relatively easy, in both the stimulus and response. The factors which produce a male sexual response are well-understood, and the penile plesmythograph (an instrument for measuring penile erection) has been in use for decades.
Studying female sexual response is not at all simple. Masters and Johnson approached the female sexual response as if it operated, anatomically and physiologically, the same as the male sexual response. For example, instead of the plesmythograph, they used a glass capsule in the shape of a penis with a camera inside to visualize the female vagina during simulated intercourse. Turns out there is a lot more going on.
For both male and female, there are at least two components to the sexual response. The first, the reflexive component, is easiest to study and is well-understood. The second, the psychological component, is much less understood.
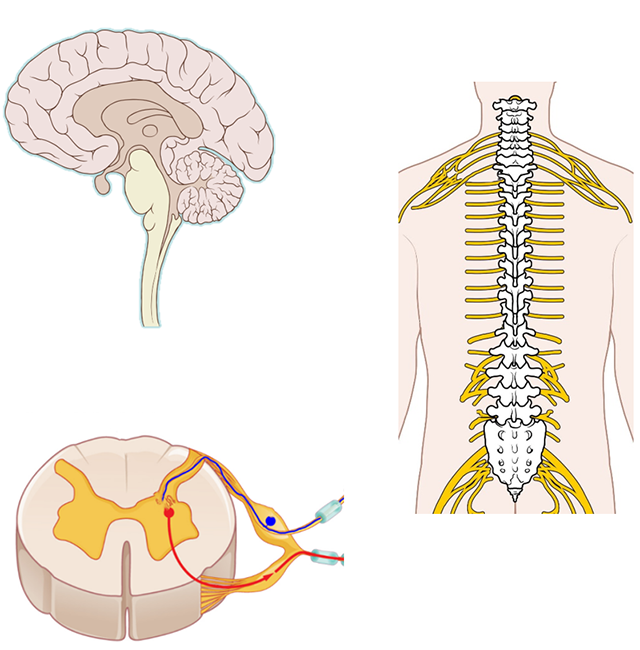
The reflexive component is primarily controlled by the autonomic nervous system and is wired through spinal nerves S2-S4 (sensory); S2-S4 (parasympathetic motor); and T10-L2 (sympathetic motor). Descending influences from the cortex are obviously important in this system, probably much more so in the female than in the male.
In males, activation of the sympathetic response (fight-or-flight) promotes flaccidity. Sympathetic neurotransmitters, like norepinephrine and epinephrine (acting through α-adrenoceptors) cause blood vessels supplying the penis to constrict, which prevents erection. This should make sense, as it’s pretty obvious a penile erection has no place in the fight-or-flight response.
On the other hand, parasympathetic activation promotes penile erection. The hypothalamus and limbic systems of the brain control the psychological aspects of penile erection. Stimulation of nerves leads to release of nitric oxide (NO), vasoactive intestinal polypeptide (VIP), calcitonin gene-related peptide (CGRP), and prostaglandin. Let’s take a closer look at NO.
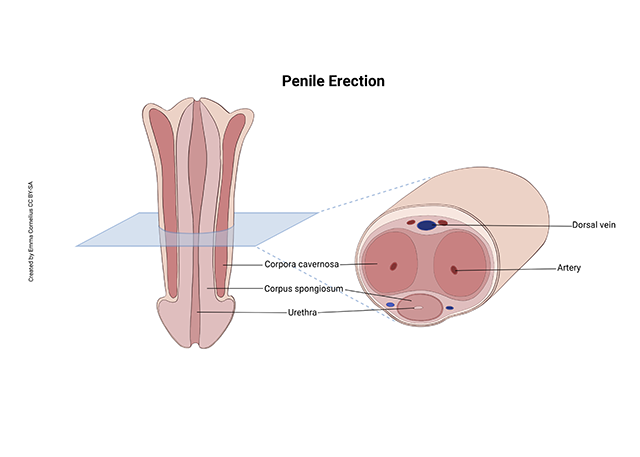
Three things cause a male penis to become erect.
- The smooth muscle of the corpora cavernosa relax, allowing blood to fill the open spaces in this spongy tissue.
- Arterial blood flow to the penis increases.
- Out-flow of blood from the penis is restricted (venous congestion)
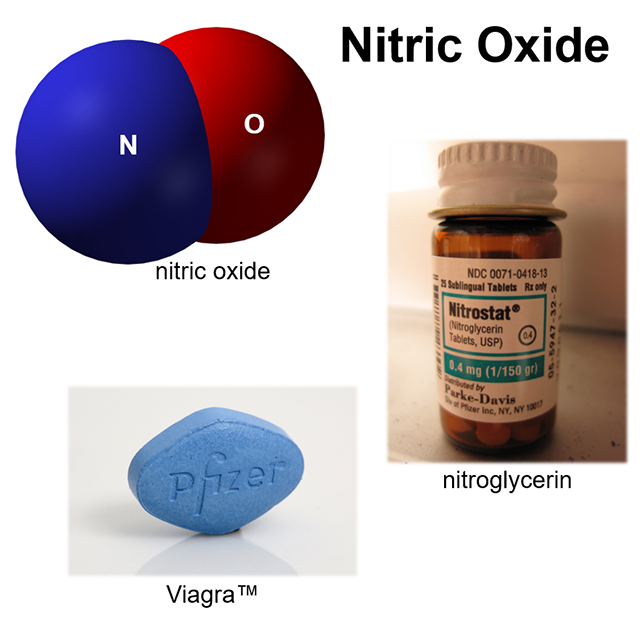
Nitric oxide (NO) promotes dilation of blood vessels throughout the body. For example, nitroglycerine, a precursor of NO, is used to relieve heart-related chest pain (angina) by dilating coronary blood vessels and increasing blood flow to the heart. NO has the same relaxing effect in the blood vessels in and around the penis. Increased NO promotes penile erection by stimulating all three of the above processes.
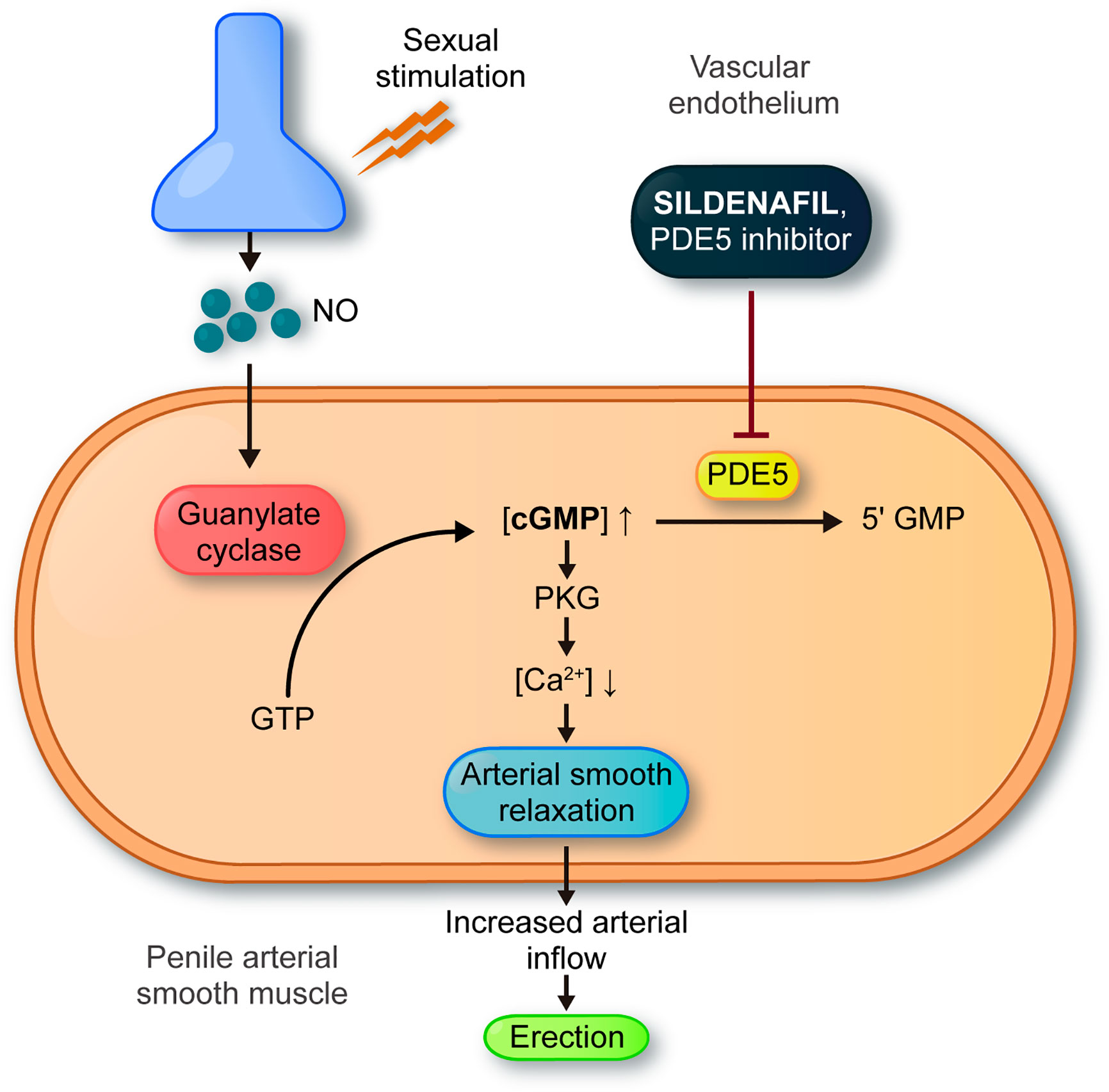
The popular drug sildenafil (Viagra™) works similarly to NO, producing greater smooth muscle relaxation, increased blood flow to the penis, and improved and prolonged penile erection. It should be apparent why men should not take nitrates at the same time they’re taking Viagra.
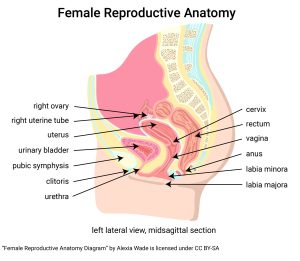 Female arousal is somewhat more complicated. In terms of the mechanics of arousal, the same mechanisms seen in the penis are also observable in the clitoris (blood filling erectile tissue).
Female arousal is somewhat more complicated. In terms of the mechanics of arousal, the same mechanisms seen in the penis are also observable in the clitoris (blood filling erectile tissue).
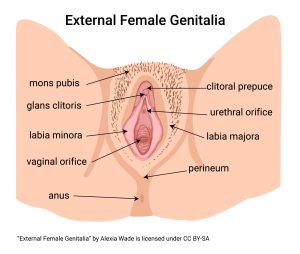
However, trials aimed at improving female sexual response using NO agonists (like Viagra™) have been complete failures. Yes, NO agonists increase and prolong erection of clitoral tissues, but this does not equate with improved female sexual arousal. We conclude that, while there is little more to male sexual response than penile erection, in females, merely causing clitoral erection is not enough to produce sexual arousal.
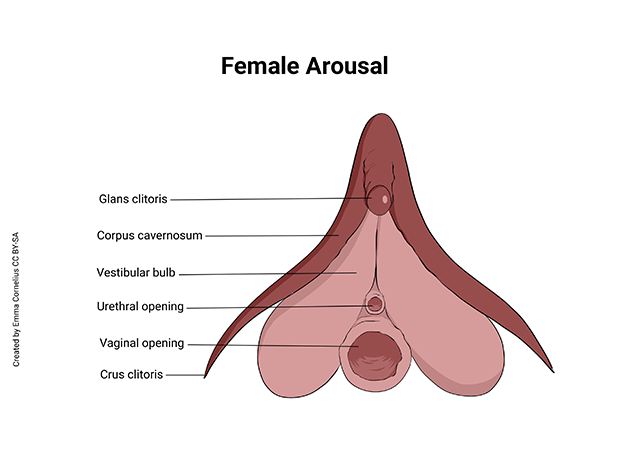
Direct imaging of female genital tissues shows that two areas are consistently engorged in sexual arousal: the glans clitoris and the vestibular bulb. The role of the glans clitoris in sexual arousal has been established for some time and is not controversial. However, there is much more to the clitoris than what is visible in the vulvar area (the glans clitoris). The rest of the clitoris (crus clitoris and vestibular bulb) is internal and lies on either side of the vaginal entrance. Also, the vestibular bulb, the pubocervical fascia, and the paraurethral glands embedded in nearby tissue, are homologous to the corpus spongiosum in males, so embryonic origin is consistent with a similar role in female sexual arousal.
A third region that has been the source of some controversy in the medical literature is the so-called Gräfenberg spot (“G-spot”), a location in the anterior vaginal wall near the position of the pubocervical fascia. Some investigators argue that the tissue in this area may be sexually responsive as well, but consistent data has been difficult to gather. It is possible that there are significant individual differences in the sexual responsiveness of this area.
Clearly, there is much more to be learned about the human sexual response, particularly in the female.
Media Attributions
- U20-069 Puberty © Cornelius, Emma is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U20-070 Puberty Triggers © Cornelius, Emma is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U20-071 Average Age of Menarche © Winterton, Brad is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-072 Declining Age of Menarche © Boaz, Noel Thomas is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-073 Mean Age at Menarche © Cornelius, Emma is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-074 Nerves of Sexual Arousal Composite © Lynch, Patrick J.; Andrewmeyerson | OpenStax adapted by Jim Hutchins is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-075 Penile Erection © Cornelius, Emma is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-076a Sildenafil Composite © Benjah-bmm27; Intropin and Kehkasha adapted by Jim Hutchins is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-076b PDE5 Inhibitors © Marian Cruz-Burgos et al. is licensed under a CC BY (Attribution) license
- U20-008 Female Reproductive Anatomy © Wade, Alexia is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-009 External Female Genitalia © Wade, Alexia is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-077 Clitoral Anatomy © Cornelius, Emma is licensed under a CC BY-SA (Attribution ShareAlike) license

