Production and Transport of Male Gametes
Objective 5
Characterize the process of spermatogenesis, the organs involved, the route sperm take through the duct system during ejaculation, the additional organs involved in semen production, and the composition of semen and its role in sperm function.
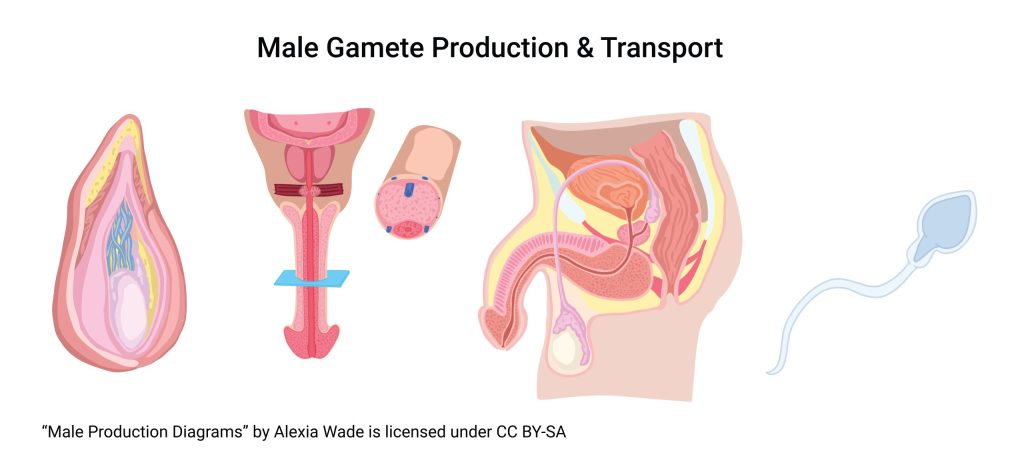
Let’s consider the whole process, briefly; then we’ll look at the specific steps and functions in more detail. Male gametes are spermatozoa. Spermatozoa are produced in the testes and then stored and undergo final maturation in the epididymis. In preparation for ejaculation, they travel from the epididymis through the ductus deferens to just outside the prostate, near the neck of the urinary bladder. There, seminal vesicles, the prostate, and bulbourethral glands add secretions and the mixture is released into the urethra for ejaculation, which occurs through the external urethral orifice at the tip of the glans penis.
Spermatogenesis
Let’s break this process down into several steps.
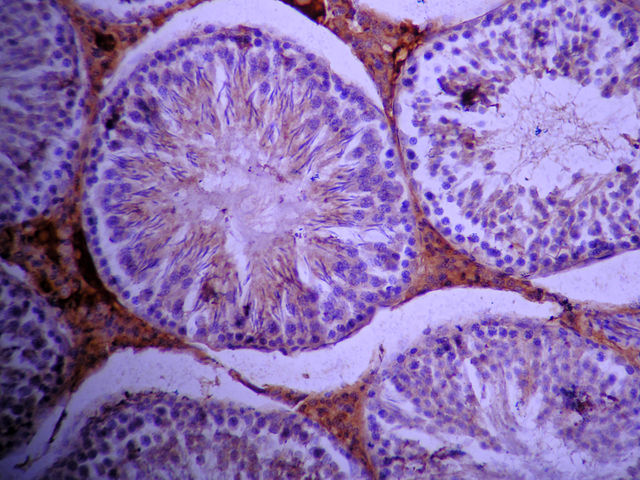
Step 1. The tissue lining the seminiferous tubules generates gametes from a population of stem cells. Each seminiferous tubule is about 60 cm in length and there are about 500 tubules tightly coiled in each testis for an estimated total length of about 600 m of seminiferous tubules in one male (60 cm/tubule x 500 tubules/testis x 2 testes/male = 60,000 cm/male = 600 m/male = ⅓ mile/male). About 500 spermatozoa are released per mm of tubule per day, or about 300 million sperm per day (500 sperm/mm/day x 10 mm/cm x 60,000 cm/male = 300,000,000 sperm/male/day).
The capillaries of the testes and the interstitial cells that make testosterone are separated from the lining of the seminiferous tubule by a basement membrane. This arrangement forms a blood-testis barrier. The barrier protects developing sperm from the immune system. Oxygen and other nutrients diffuse easily across the blood-testis barrier but immune cells and antibodies cannot.
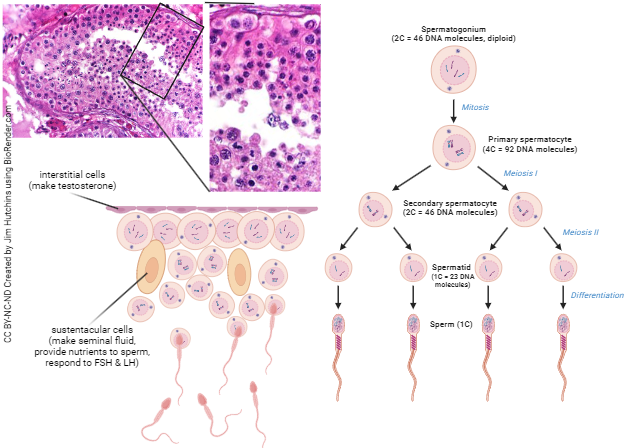
Spermatogenic stem cells, called spermatogonia, are found lining the basement membrane of the seminiferous tubules (opposite side of the basement membrane from the interstitial cells and blood capillaries). These cells constantly divide, with one daughter cell remaining “attached” to the basement membrane and the other differentiating to become a primary spermatocyte. Primary spermatocytes become secondary spermatocytes, secondary spermatocytes become early spermatids, and early spermatids become late spermatids.
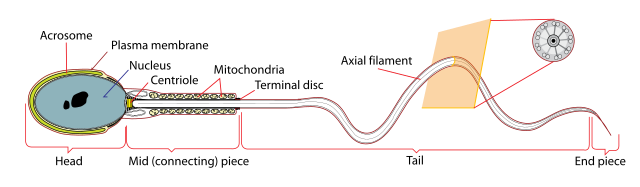
Finally, once the developing cell has become nothing but a “payload” (acrosome to penetrate the egg plus paternal DNA to contribute to fertilization) on top of a “rocket” (flagellum plus mitochondria for energy metabolism), it is called a spermatozoon (“living sperm“).
 The seminiferous tubules empty into the rete testis (Latin: “network of the testicle”). From there, sperm travel through efferent ducts into the head of the epididymis, then through the body of the epididymis, and into the tail of the epididymis.
The seminiferous tubules empty into the rete testis (Latin: “network of the testicle”). From there, sperm travel through efferent ducts into the head of the epididymis, then through the body of the epididymis, and into the tail of the epididymis.
Travel through the three sections of the epididymis (head, body, tail) takes about 14 days. During the journey, sperm mature by gaining motility (movement) and also the ability to fertilize an oocyte.
If sexual arousal occurs, a thin layer of smooth muscle surrounding the epididymis (under sympathetic control) contracts, forcing the sperm into the ductus deferens. If sexual activity does not occur, sperm that hang around in the epididymis longer than about 14 days are reabsorbed.
During sexual arousal, at the same time sperm are being forced out of the epididymis and through the ductus deferens, the bulbourethral glands are activated. These lie just inferior to the prostate, on either side of the urethra. Their alkaline secretions lubricate the urethra and buffer its pH in preparation for ejaculation. Small amounts of this secretion, appearing from the external urethral meatus at the tip of an erect penis, are called pre-ejaculate (often contain small numbers of fully mature sperm).
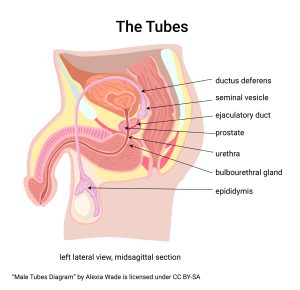
Each ductus deferens joins the duct of the ipsilateral (same side) seminal vesicle to form an ejaculatory duct. The two ejaculatory ducts join the urethra in the prostate gland. Once the prostate and seminal vesicles have added their secretions, the combination (sperm + seminal vesicle secretions + prostate gland secretions) is called semen. This semen may now be ejaculated.
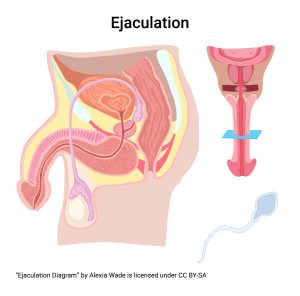
While sexual arousal is under parasympathetic control, ejaculation is a sympathetic reflex. Sensory neurons from the penis and surrounding areas carry information back to the lumbar spinal cord, where sympathetic motor neurons activate the muscles that trigger ejaculation. The internal urethral sphincter closes to prevent urine leakage and backflow of semen. Peristaltic waves in the epididymes, ducti deferens, seminal vesicles, ejaculatory ducts, and prostate coincide with strong contractions of the muscles surrounding the root of the penis (bulbospongiosus, ischiocavernosus, and superficial transverse perineus) to propel semen into, through, and out of the urethra. The result is ejaculation. Most of the muscles involved are smooth muscle, but a few striated muscles participate as well.
Semen

Semen is a mixture of sperm from the testes and epididymis plus secretions from the seminal vesicles and prostate gland. In other words, semen is sperm plus accessory gland secretions. The bulbourethral glands make a small contribution, but most of the bulbourethral secretion lubricates and buffers the urethra before ejaculation.
Average ejaculate volume is 2.5 – 5.0 ml (≈ 3 ml or ≈ ⅔ teaspoon). Semen contains about 100 million sperm per ml. Anything less than 20 million per ml would be defined as infertility. Combining the average ejaculate volume and the average sperm count per ml, the average ejaculate contains about 300 million sperm, which is equivalent to 24 hours of continuous sperm production by the testes. This suggests that, for couples trying to get pregnant, frequency of intercourse greater than once every 24 hours does not increase chances of conception.
Recall this statement from Objective 2: “…they need a safe liquid medium in which to swim and a sack lunch for nutrition along the way.” These requirements are filled by the accessory glands. The seminal vesicles add secretions with alkaline buffering capacity, fructose, and prostaglandins. The fructose is the fuel used by flagellar mitochondria to propel spermatozoa forward. The prostate contributes Zn2+, citrate ions, and the enzyme acid phosphatase. Since acid phosphatase is very low in blood, its presence in forensic testing is used to indicate the presence of semen.
Semen contains clotting proteins (different than those in blood) and clots about 5 minutes after ejaculation, but no one knows why. About 15-20 minutes later, semen re-liquefies. One of the major anti-clotting agents is prostate-specific antigen (PSA), a prostatic secretion that is also used to detect prostate cancer in men. Blood PSA level is commonly used to screen for prostate cancer, even though evidence of the relationship between increased blood PSA and prostate cancer remains a bit tenuous.
Media Attributions
- U20-017 Male Gamete Production and Transport © Wade, Alexia is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-018 Rat Seminiferous Tubules © TrJaagup is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-004 Spermatogenesis © CoRus13 and BioRender adapted by Jim Hutchins is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U20-019 Simplified Spermatozoon Diagram © Ruiz, Mariana is licensed under a Public Domain license
- U20-005 Testisanimacion © KDS444 is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-021 Male Tubes © Wade, Alexia is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-022 Ejaculation © Wade, Alexia is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-023 Human Semen in Petri Dish © Jchoi30 is licensed under a Public Domain license

