Pregnancy, Birth, and Lactation
Objective 11
List the changes in female physiology that result from pregnancy, including effects on the cardiovascular, respiratory, and urinary systems. Describe the events that initiate labor, the hormonal signals involved, and the three stages of labor. Describe the structure and function of mammary glands.
Physiologic Changes in Pregnancy
To understand the physiologic changes caused by pregnancy, we need to consider the levels of six different hormones. Four of these – human chorionic gonadotropin (hCG), relaxin, human chorionic somatomammotropin (hCS), and corticotropin releasing hormone (CRH) – are produced exclusively by the placenta (and, therefore, only during pregnancy). The other two – estrogen and progesterone – are also produced by the placenta during pregnancy and, additionally, are produced by the ovaries outside of pregnancy.
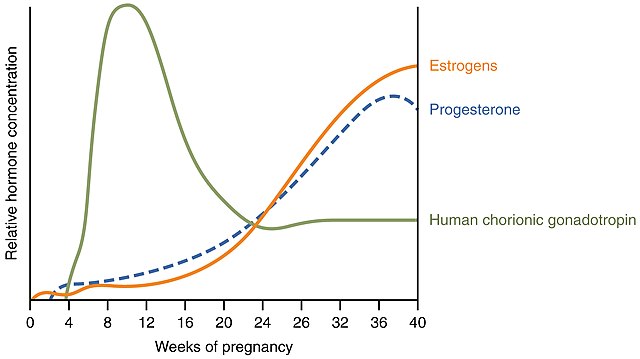
The name human chorionic gonadotropin tells us this hormone is released by the chorionic membrane and acts on the gonads. In fact, hCG supports the function of the corpus luteum. Recall that the corpus luteum (CL) is the remnant of the ruptured follicle after the secondary oocyte is released at ovulation. If pregnancy does not occur, the CL continues secreting estrogen and progesterone for only about two weeks before becoming the corpus albicans (scar tissue). If pregnancy does occur, hCG keeps the CL “alive,” producing estrogen and progesterone, for about three months longer (Note: not the entire pregnancy). The peak hCG level occurs quite early in pregnancy. Since it can be detected in urine, it is used as the basis for home pregnancy tests. Detection starts at about 10-12 days post-ovulation, or about the time of the first missed period.
Relaxin, released by the placenta, helps at childbirth by relaxing the pubic symphysis to make it more flexible (thus, slightly enlarging the pelvic canal) and relaxing the cervix to aid in dilation.
Human chorionic somatomammotropin (hCS) alters maternal metabolism to compensate for the nutritional requirements of the fetus. To ensure enough glucose availability for fetal growth and development, hCS decreases maternal glucose use and increases maternal fatty acid metabolism (gluconeogenesis). It also increases maternal protein synthesis.
Corticotropin releasing hormone (CRH) establishes the time of birth and increases cortisol secretion from the adrenal cortex. (Note: recall, in unit 14, we said something like “Any time you see the term ‘something something releasing hormone,’ you know it is being released by the hypothalamus and going to the anterior pituitary.” This is the exception to that statement – CRH is released by the placenta and goes to the adrenal cortex.)
Estrogen and progestrone levels remain high throughout pregnancy, with progesterone levels dropping just before childbirth.
Pregnancy alters maternal metabolism in fairly significant ways. As described above related to hCS, mom’s physiology must shift to meet the various demands of the fetus. These changes include:
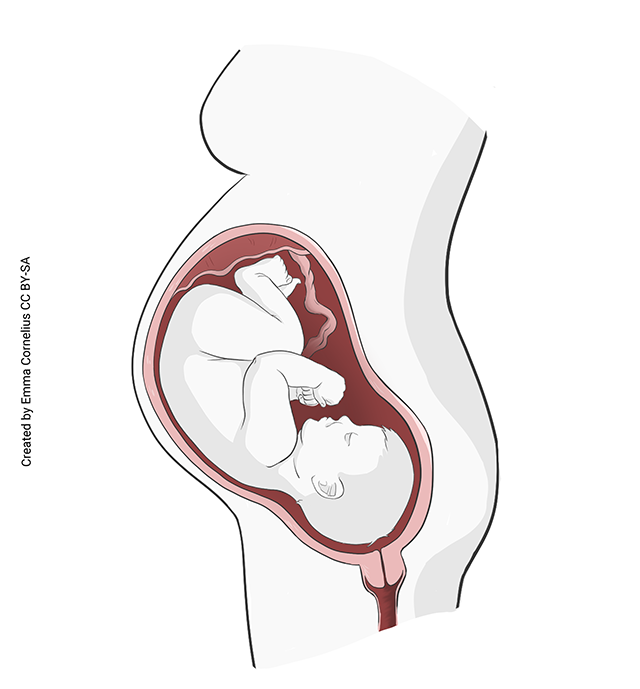 Cardiovascular
Cardiovascular
- increased stroke volume
- increased cardiac output
- increased heart rate
- increased blood volume
- compression of inferior vena cava, leading to lower extremity edema and varicose veins
- compression of renal artery may lead to renal hypertension
Respiratory
- increased tidal volume
- decreased expiratory reserve volume (ERV)
- increased ventilation
- increased total oxygen consumption
- dyspnea possible
- Gastrointestinal
- increased appetite
- decreased bowel motility (may cause GI symptoms)
Gastrointestinal
- increased appetite
- decreased bowel motility (may cause GI symptoms)
- direct pressure of fetus and placenta reduces bladder volume
- increased glomerular filtration rate
Clinical Connection: Eclampsia & Preeclampsia
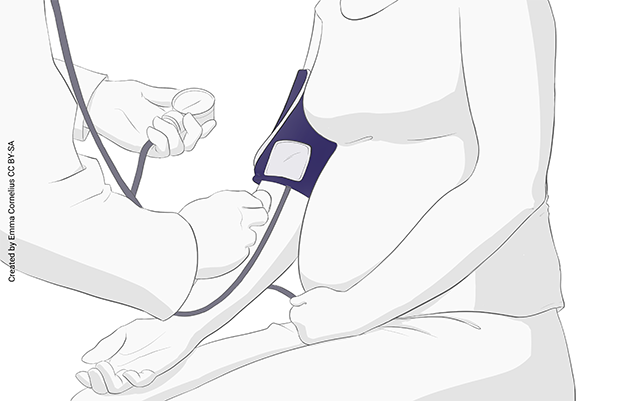 Preeclampsia (or toxemia of pregnancy) occurs in about 4% of pregnancies. The cardinal signs of pre-eclampsia are a rapid rise in blood pressure (to hypertensive levels) and proteinuria.
Preeclampsia (or toxemia of pregnancy) occurs in about 4% of pregnancies. The cardinal signs of pre-eclampsia are a rapid rise in blood pressure (to hypertensive levels) and proteinuria.
Preeclampsia rarely progresses to eclampsia, but when it does, it is life-threatening and hard to control. Vasospasm and clonic seizures may occur.
A closely related complication of pregnancy is HELLP syndrome, which occurs in about 10% of women with preeclampsia. This life-threatening condition gets its name from its clinical signs: hemolytic anemia, elevated liver enzymes, and low platelet count.
The causes of these conditions remain obscure. Hormonal fluctuations have been ruled out. It appears to be some sort of autoimmune disorder triggered by the fetus.
Labor
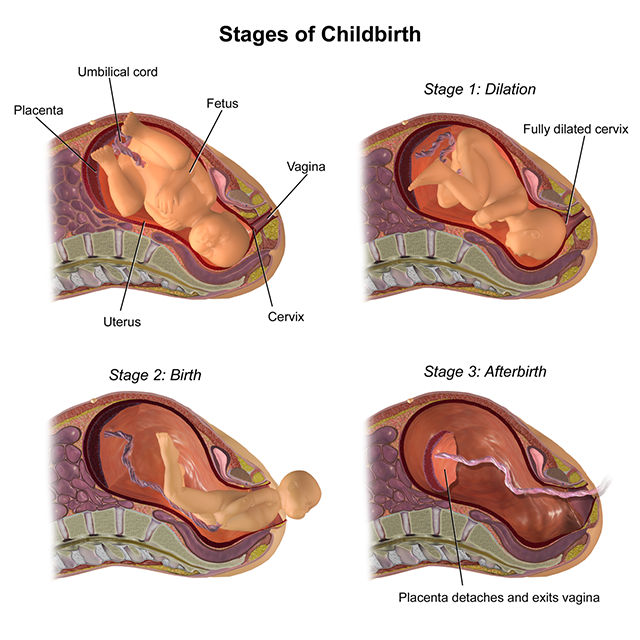
Labor has three stages:
- Dilation stage
- Expulsion stage
- Placental stage
The dilation stage begins with uterine contractions. The estrogen/progesterone ratio, increased maternal oxytocin release, and increased fetal oxytocin release probably all play a role in initiating parturition (childbirth). This phase can last 6 to 12 hours, and ends when the cervix is fully dilated (10 cm).
The expulsion stage can last 10 minutes to several hours. It begins with the end of the dilation phase (ie, full cervical dilation) and ends with delivery of the baby. Irritation of the cervix and stretch of the uterine musculature both increase uterine contractility, in a positive feedback loop. The baby passes through the cervix and vaginal canal and is born.
The final stage, the placental stage, can last 5 to 30 minutes or more. Strong uterine contractions continue, expelling the placenta and helping to control bleeding.
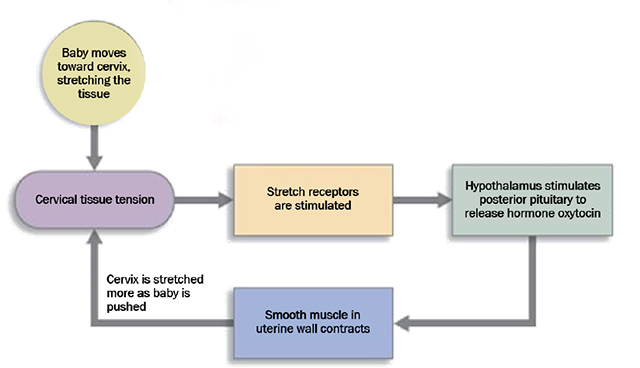
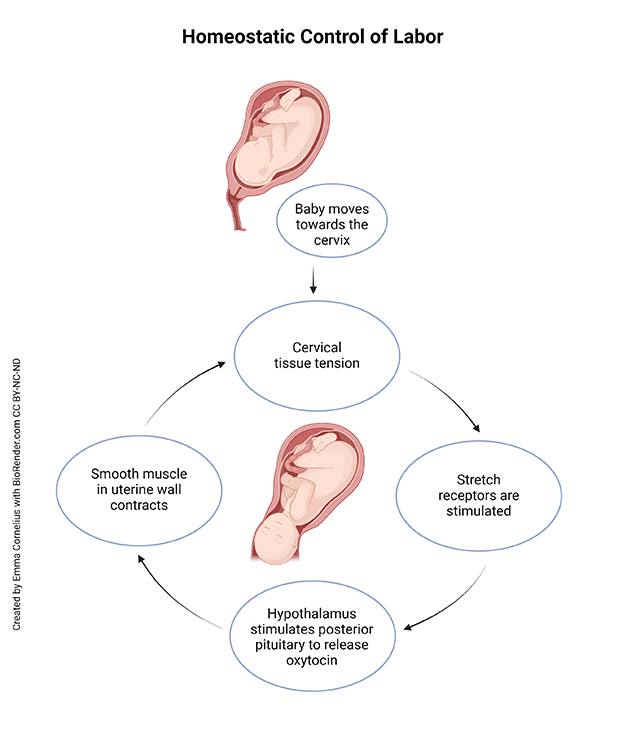
Labor (parturition) is a rare example of a positive feedback loop. Positive feedback loops are generally avoided in the body because they can “spin out of control.” In the case of parturition, what prevents that from happening? Remember that, in a positive feedback loop, the response to the stimulus reinforces the stimulus. In labor, the stimulus is the baby’s head pressing on the cervix. Stretch receptors in the cervical tissue pick up the stimulus and send it to the brain. The brain tells the posterior pituitary to release oxytocin. The oxytocin stimulates strong contractions of the smooth muscle myometrium. The uterine contractions make baby’s head push harder on the cervix, stimulating the stretch receptors. And the loop repeats. The positive reinforcement will continue until the stimulus is removed, in this case delivery of the baby.
Lactation
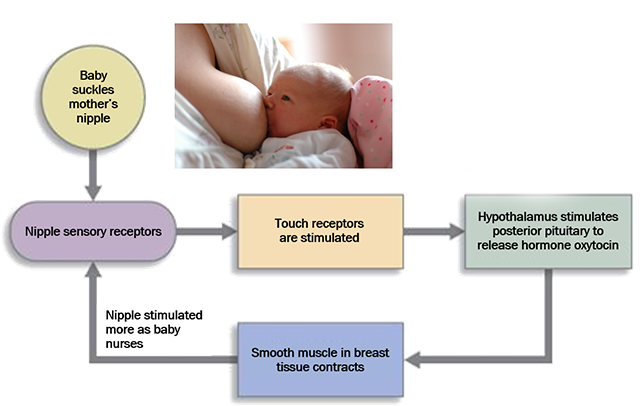
Another positive feedback loop is associated with childbirth – the suckling or milk let-down reflex, which allows the newborn to nurse.
If you place your fingers close to the newborn baby’s lips, the baby will “suckle” your fingers. When the baby’s lips suckle the mother’s nipple, a sensory signal reaches the hypothalamus. Neurosecretory cell bodies in the hypothalamus send action potentials down their axons to the posterior pituitary, where they release oxytocin from their terminal end bulbs. (Wait, didn’t we just talk about oxytocin in relation to labor? Actually, yes, oxytocin is the hormone involved in both uterine contractions and milk let-down, and both are positive feedback loops).
The mother’s mammary glands, under the influence of prolactin from the anterior pituitary, have already made and stored milk. In response to the suckling stimulation, the oxytocin stimulates contraction of special fibers in breast tissue, which expresses the stored milk into the mammary ducts so it is available for baby. Thus, the milk let-down reflex involves only the release of this stored milk.
Interestingly, researchers have found evidence suggesting that oxytocin is also released during coitus. They speculate that the rush of emotion felt during sexual intercourse and the rush of emotion women feel during nursing may be related. Both seem to serve the same purpose: to increase relationship bonds – between husband and wife and between mother and child.
Mammary Glands
Mammary glands are a female secondary sexual characteristic. They are the anatomical structure that gives Class Mammalia its name – live birth and suckling young are characteristics of all mammals.
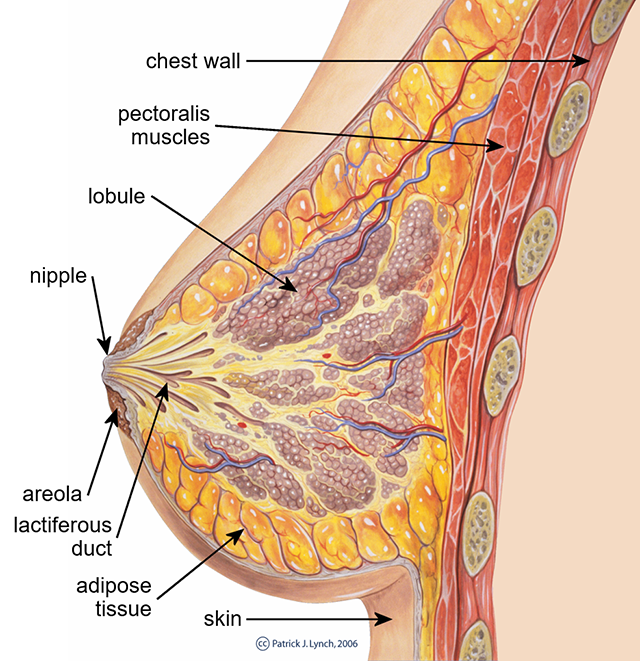
Mammary glands are modified sudoriferous (sweat) glands. Instead of salty water with a small amount of protein (sweat), these glands produce a secretion rich in sugars, proteins, and fats. Most of the breast is made up of adipose tissue. Embedded in the adipose are groups of alveolar (grape cluster-shaped) glands. These glands are grouped into lobules and surrounded by myoepithelial cells. When stimulated by oxytocin, the myoepithelial cells contract, expressing milk from the alveoli into mammary ducts, then into lactiferous sinuses, then into lactiferous ducts, and then to the nipple. In this manner, milk is delivered to the baby.
The nipple is surrounded by a pigmented tissue called the areola. The structure of the breast is maintained by numerous suspensory ligaments (Cooper’s ligaments). These ligaments become stretched throughout life.
Media Attributions
- U20-061 Hormones Initiating Labor © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U20-062 Physiological Changes © Cornelius, Emma is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-063 Eclampsia © Cornelius, Emma is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-064 Stages of Childbirth © BruceBlaus is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-065 Homeostatic Control of Labor © Cornelius, Emma is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U20-066 Homeostatic Control of Labor Positive Feedback Loop © Winterton, Brad is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-067 Suckling Positive Feedback Loop © Nosik, Anton adapted by Brad Winterton is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-068 Breast Anatomy © Lynch, Patrick J. adapted by Brad Winterton is licensed under a CC BY (Attribution) license

