Ovarian Cycle
Objective 6
Identify the stages of ovarian follicular development, oogenesis, and how both fit into the overall ovarian cycle. Describe female gamete transport and the organs involved.
Follicular Development
Female gametes (ova, singular ovum) begin as oocytes which mature in the ovaries. The structure that encloses an oocyte and promotes its maturation is called an ovarian follicle. In general, the female reproductive system matures only one follicle in one ovary per menstrual cycle, beginning with menarche (first menstruation) and continuing through menopause (last menstruation). Occasionally, one follicle will mature and rupture from each ovary, which can result in fraternal (non-identical) twins.
During fetal development, oogonia (oogenic stem cells) in the developing ovaries undergo their last cell division and then remain in a quiescent state as primary oocytes until menarche. Each primary oocyte is surrounded by a single layer of follicular cells.
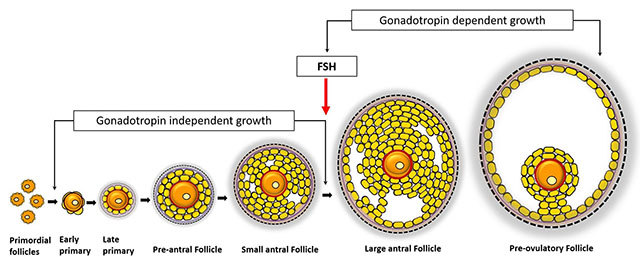
Beginning at menarche, once per cycle, several (5-12) primordial follicles begin to change. The follicular cells surrounding the primary oocyte divide and differentiate into granulosa cells. Once there are several concentric layers of granulosa cells surrounding the primary oocyte, the primordial follicle is called a primary follicle (pre-antral follicle). At some point in the primordial-follicle-to-primary-follicle process, one of the developing follicles is “chosen” to continue development (we have no idea how this occurs), while the remaining follicles that had started to develop (4-11) will degenerate (their chance to mature fully has now passed). As the granulosa cells continue to divide, a fluid-filled space (follicular antrum, filled with follicular fluid) develops, at which point the primary follicle becomes a secondary follicle (antral follicle). More than one antrum may develop, which will coalesce and enlarge to form a single fluid-filled space. Finally, when follicular fluid volume predominates over granulosa cells, the follicle is called a mature follicle (Graafian follicle) (about 2 cm in diameter) and is ready to rupture, releasing the oocyte inside, a process called ovulation.
Confusingly, the same identifiers (primary, secondary) are used for both follicle stages and oocyte stages. It might be a good idea to remember that primordial, primary, secondary, and mature follicles contain a single primary oocyte (in other words, a secondary follicle does not contain a secondary oocyte).
Ovulation & Hormonal Control of the Ovarian Cycle
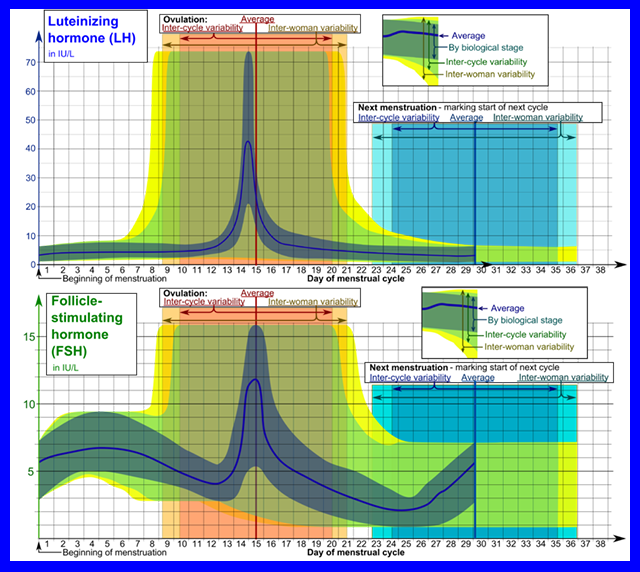
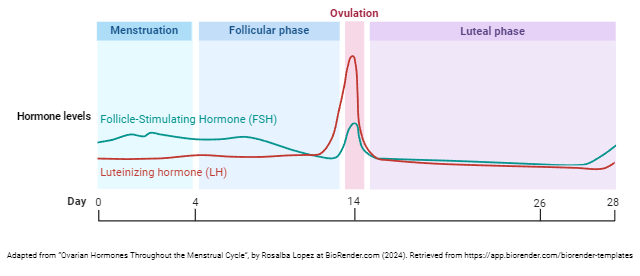
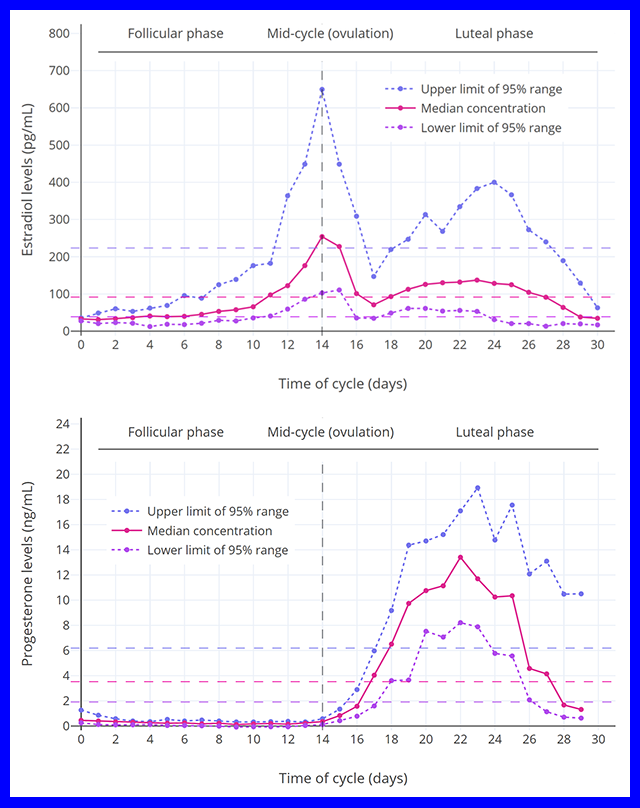
These graphs show “real data” for the levels of luteinizing hormone and follicle-stimulating hormone during women’s menstrual cycle. Note the variability in these curves; when we present the data that you need to remember, we will take the idealized version of these curves. In textbooks, the fluctuation in hormone levels is presented as a rigid process when in reality it’s not that consistent.
In this image, the basic steps of follicular development are shown. These are not meant to represent a follicle moving around, but rather the stages a follicle goes through as it develops. It starts at upper right with primordial follicles (each with a primary oocyte); then the primary follicle (with a primary oocyte); then the secondary follicle (with a primary oocyte); then the mature follicle (with a primary oocyte); and finally shows follicular rupture (releasing a secondary oocyte) — ovulation — at upper left.
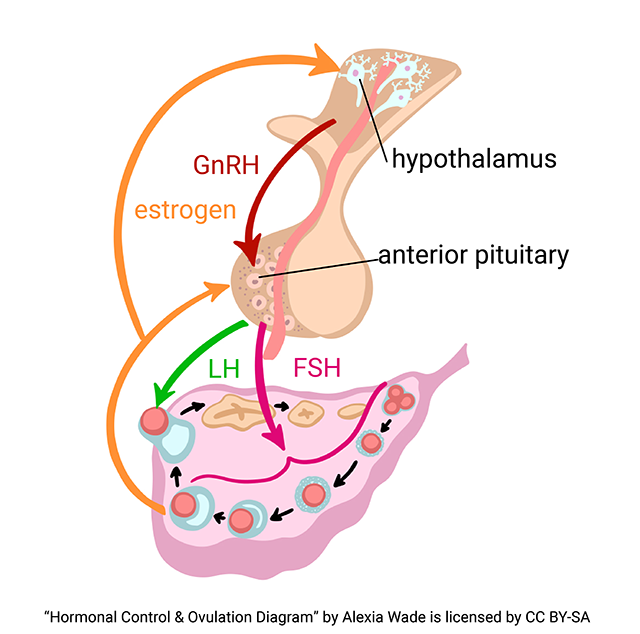
Recall, from Unit 14, The Endocrine System, that the hypothalamus releases gonadotropin releasing hormone (GnRH) into the hypophyseal portal system and the anterior pituitary (adenohypophysis) responds by releasing follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
FSH is released by the anterior pituitary early in the cycle. It promotes the maturation of primordial follicles into primary follicles, a primary follicle into a secondary follicle, and the secondary follicle into a mature follicle. Meanwhile, this developing follicle secretes increasing amounts of estrogen, which stimulates the hypothalamus to release more GnRH, which tells the anterior pituitary to release more FSH and LH. When high estrogen levels from the mature follicle reach a certain point, the anterior pituitary secretes a sudden burst of LH, causing the mature follicle to rupture and release the oocyte, which is now (finally!) called a secondary oocyte. In short, pituitary hormones (FSH & LH) control the ovarian cycle and ovarian hormones (estrogen) control the pituitary gland.
Hormonal Control of the Uterine Cycle
Again, we present “real data” on the variation in estrogen and progesterone levels during the reproductive cycle.
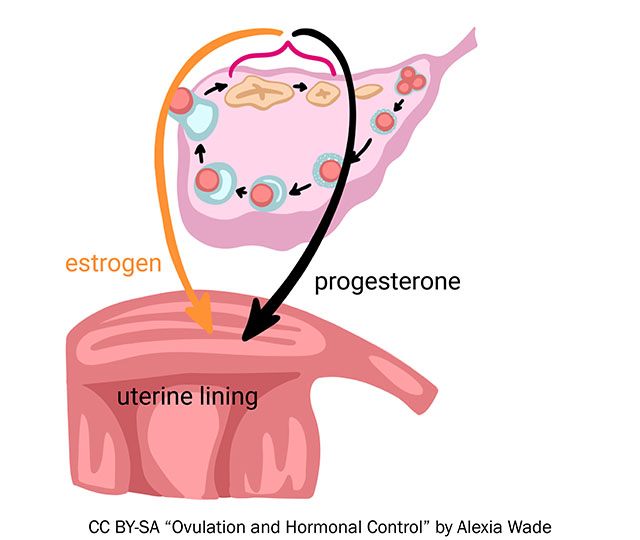
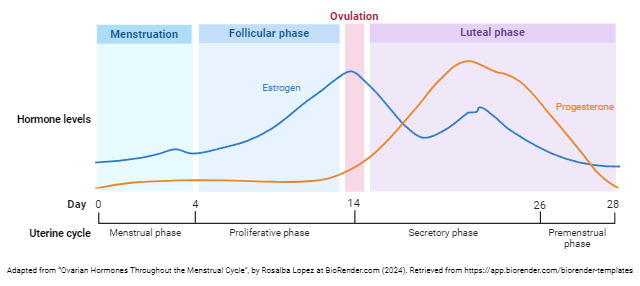
Let’s set aside the just-ovulated secondary oocyte for a few moments and consider what happens to the ovarian remnants of the ruptured mature follicle. A just-ruptured follicle is called a corpus hemorrhagicum (CH). Within a few hours, the CH fills with a yellowish, waxy substance and is called a corpus luteum (CL) (Latin: “yellow body”) (step 6 in the image). The corpus luteum secretes progesterone and estrogens whose job it is to prepare the woman’s body, the uterine lining specifically, for implantation of the fertilized gamete.
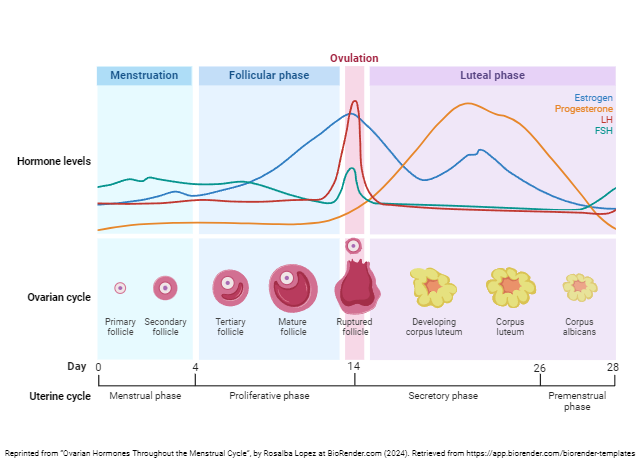
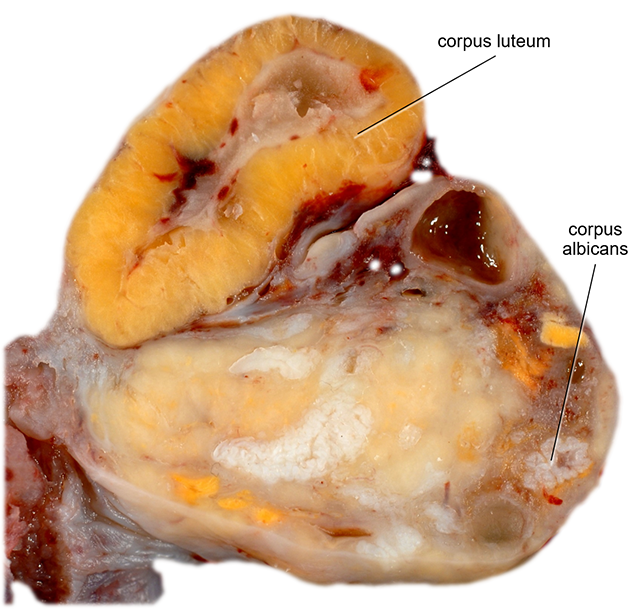
If fertilization does not occur or the embryo does not implant, the corpus luteum “burns out” – it stops secreting hormones, disintegrates (step 7 in the image), and becomes a corpus albicans (CA) (Latin: “white body”), a knot of scar tissue with no endocrine function.
Gamete Transport
Now let’s go back to the just-ovulated secondary oocyte and consider how it gets from the ovary into the uterus and what might happen along the way.
When the secondary oocyte is released at ovulation, it is immediately swept up by the fimbriae (Latin: “fringe”) into the uterine tube and begins a slow journey along the length of the tube (7-14 cm). At a travel rate of about 1-2 cm per day, it takes about a week for the secondary oocyte to traverse the length of the uterine tube and reach the uterus.
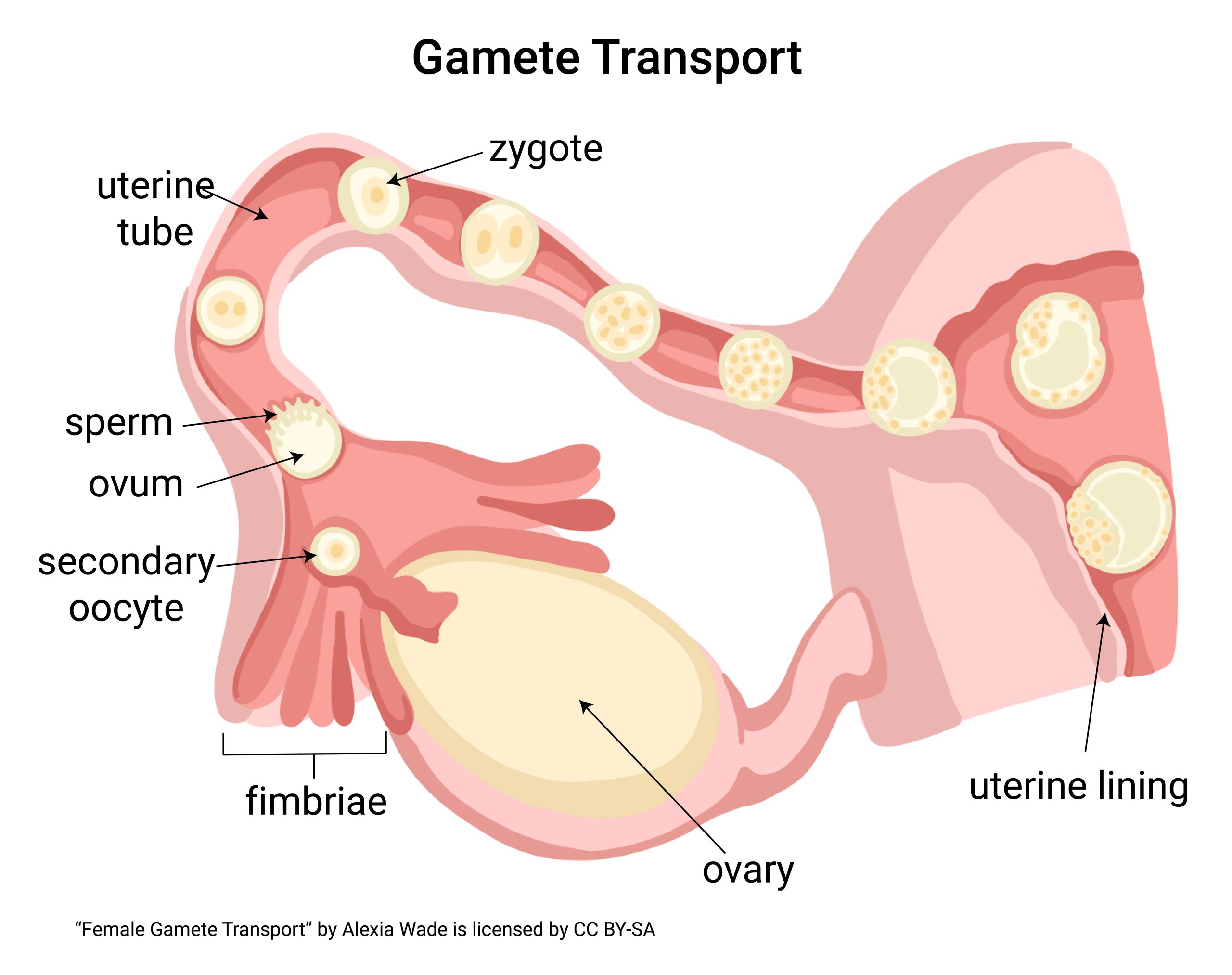
Somewhere in that journey, the secondary oocyte encounters sperm, or it doesn’t. If it does (usually closer to the uterine tube, within the first third of the journey), the secondary oocyte rapidly undergoes a final cell division to become an ovum (egg). The ovum is the female gamete that will be fertilized by one spermatozoon to become a zygote. The zygote then continues its journey out of the uterine tube and into the uterus, where it will find an implantation site. If the secondary oocyte does not encounter a sperm, it continues through the uterine tube into the uterus and becomes part of that cycle’s menstrual flow.
Remember, although we commonly hear the term ovum or egg used to describe the female gamete at all stages of the female reproductive cycle, the medically accurate terms are primary oocyte from before birth through all stages of follicular development in the ovary (years), secondary oocyte upon release from the ovary via ovulation until it encounters a sperm in uterine tube (minutes to a few days), and ovum from the sperm encounter until the male and female nuclei unite to form zygote (about 24 hours). This is explained more fully in the section on meiosis and gametogenesis.
Media Attributions
- U20-024 Folliculogenesis © Tnhath is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-025 Data LH and FSH © Häggström, Mikael adapted by Jim Hutchins is licensed under a Public Domain license
- U20-026 Hormonal Control and Ovulation © Wade, Alexia is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-027 LH and FSH Throughout the Menstrual Cycle © Lopez, Rosalba and Hutchins, Jim is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U20-028 Estrogen and Progesterone Data © MedGirl131 adapted by Jim Hutchins is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-029 Uterus Hormonal Control © Wade, Alexia is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-030 Ovarian Hormones Throughout the Uterine Cycle © Lopez, Rosalba and Hutchins, Jim is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U20-031 Ovarian Hormones Throughout the Menstrual Cycle © Lopez, Rosalba is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U20-032 Ovary Showing Corpus Luteum and Corpus Albicans © Uthman, Ed adapted by Brad Winterton is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-033 Gamete Transport © Wade, Alexia is licensed under a CC BY-SA (Attribution ShareAlike) license

