Oral Cavity, Pharynx, and Esophagus
Objective 3
Compare and contrast deciduous and permanent teeth. Identify the dental formulas for both deciduous and permanent teeth. Recognize the structures in a tooth. Describe the anatomy and functions of the tongue. Describe or identify on a diagram the location of the parotid, submandibular, and sublingual glands and ducts. Compare and contrast serous and mucous cells of the salivary glands. Identify the nasopharynx, oropharynx, and laryngopharynx and describe the functions of each with regard to the passage of food/liquids and air. Describe the structure of the esophagus. Identify the location and function of upper and lower esophageal sphincters. Understand how the location of skeletal and smooth muscle contributes to voluntary and involuntary control of swallowing (glutition). Model the process of deglutition and identify the structures involved. Describe how the larynx and glottis prevent aspiration of liquids and solids into the trachea.
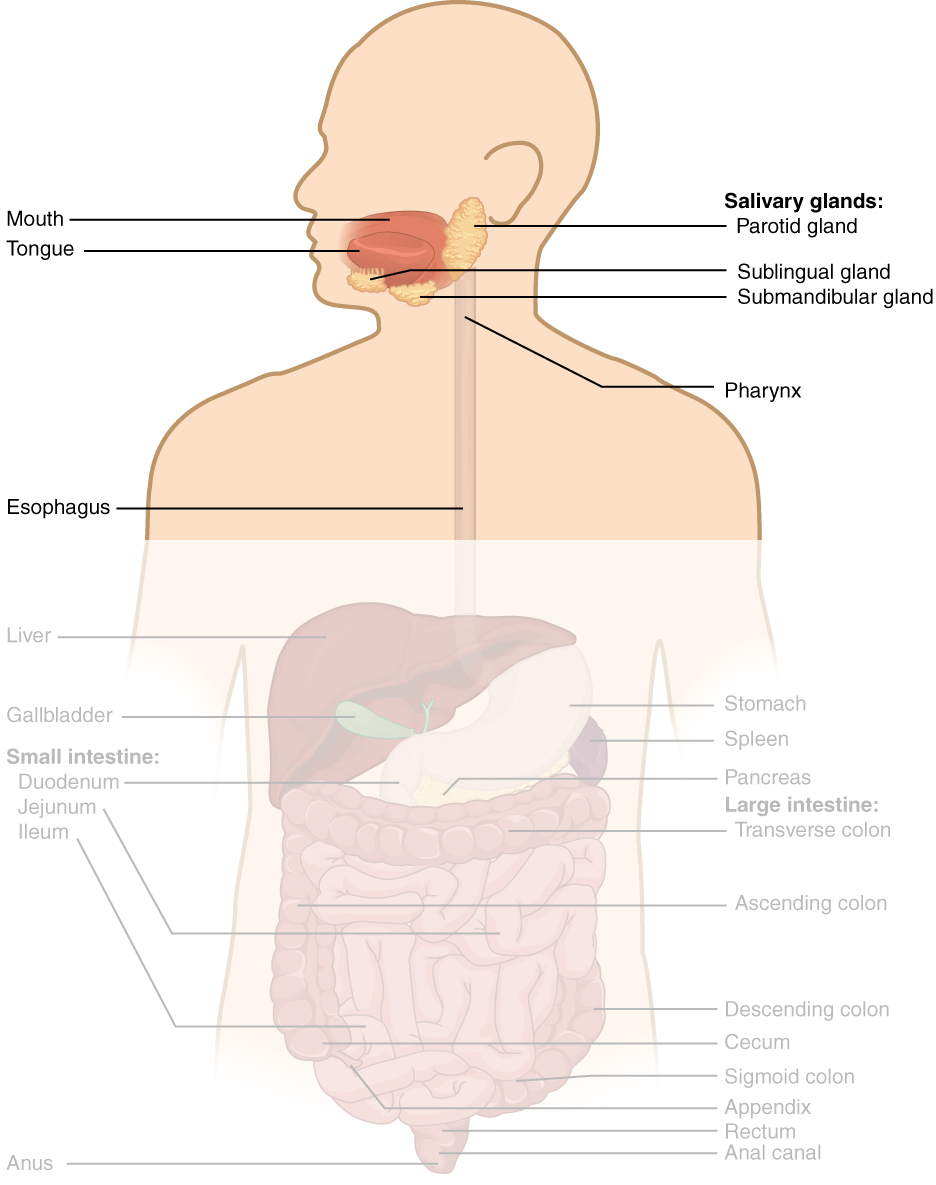
Now that we’ve taken a quick tour of the gross and microscopic anatomy of the GI tract, let’s look in detail at each of the parts of the tract, starting at the top: the oral cavity, the place where food and drink enter the digestive system.
The Oral Cavity
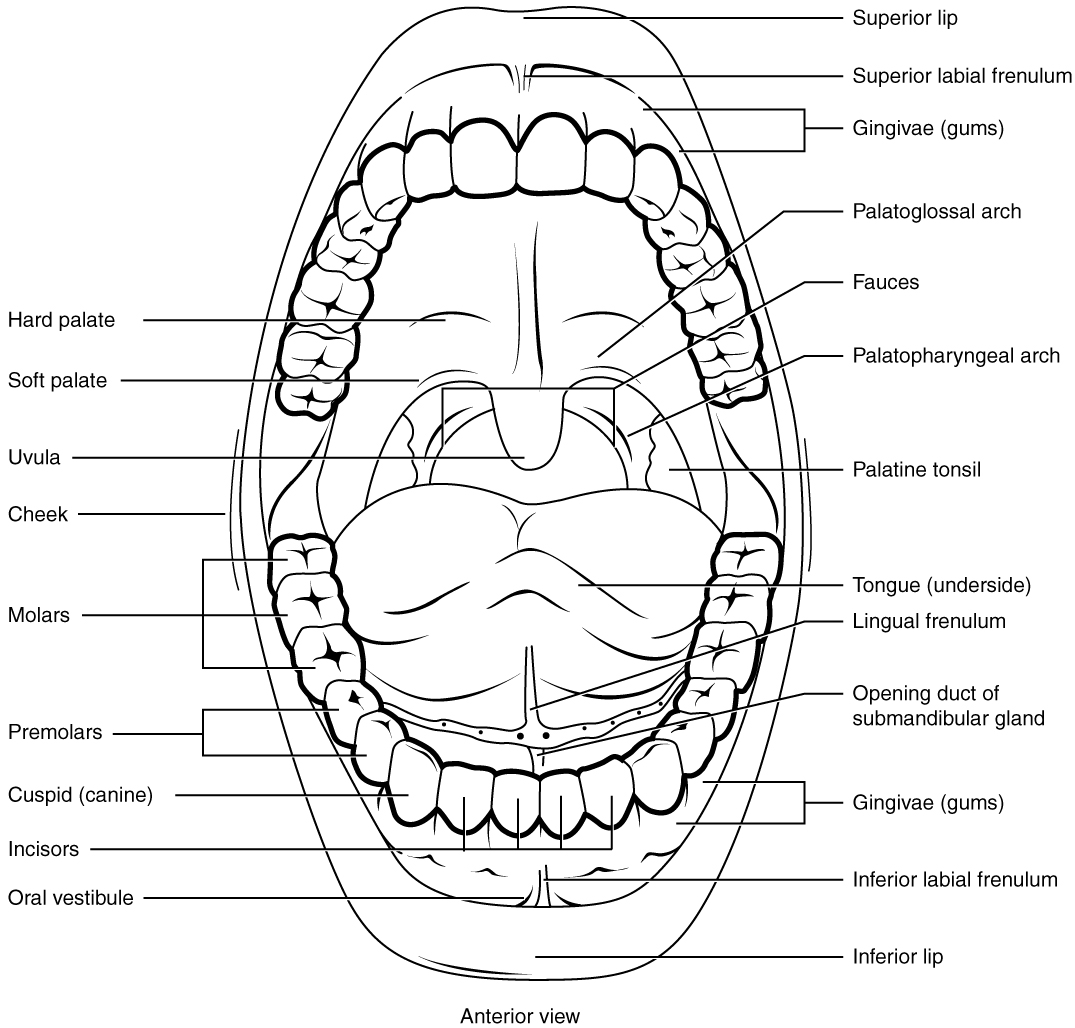
The borders of the oral cavity are the:
- cheeks or buccal surface (Latin, bucca, “cheek”) – forming the sides
- hard and soft palates – forming the “roof”
- tongue or lingual surface (Latin: lingua, “tongue”) – forming the “floor.”
There are four shapes of teeth. These shapes are the basis for the full names of the teeth:
- incisors (Latin incisus, “cut into”) – sharp cutting teeth
- cuspids (canine) teeth (Latin cuspis, “point, spear”)
- bicuspids (premolars)
- molars (Latin molere, “grindstone”)
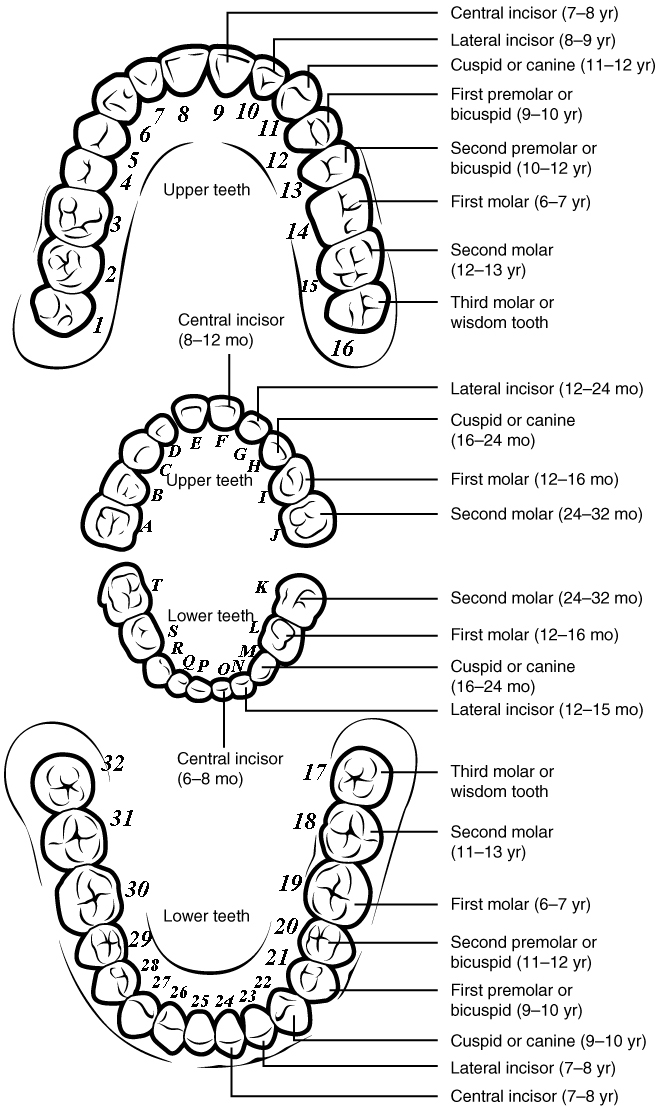 It is also common to refer to teeth by number. There are 32 teeth in a human mouth with full dentition: 8 upper right, 8 upper left, 8 lower left, 8 lower right. The most common numbering scheme in the US is from the American Dental Association and is shown here. Remember that the maxilla refers to the upper jaw, and mandible to the lower jaw.
It is also common to refer to teeth by number. There are 32 teeth in a human mouth with full dentition: 8 upper right, 8 upper left, 8 lower left, 8 lower right. The most common numbering scheme in the US is from the American Dental Association and is shown here. Remember that the maxilla refers to the upper jaw, and mandible to the lower jaw.
Numbering starts with the most distal maxillary molar on the patient’s right. The numbers continue around the upper jaw until the most distal left maxillary molar (#16). Then, the numbers continue on the left side with the most distal left mandibular molar (#17) and around the mandibular set of teeth to the most distal right mandibular molar (#32). Also note the names of the teeth on the image.
In children, teeth begin to erupt at about 6 months. This is also the time when infants are weaned (this is, of course, no coincidence, and is seen in all mammals).
Children have only 20 deciduous teeth (Latin decidere, “to fall off”, same as deciduous trees lose their leaves).
The scheme for designating these teeth uses letters A-T.
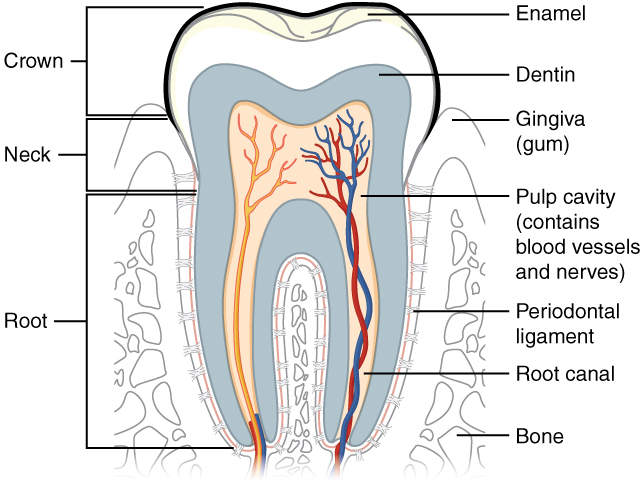
Now that we’ve got the teeth all numbered, lettered and classified, let’s look at the internal structure of a tooth.
The part of the tooth above the gumline and visible is the crown. The part just below the gumline is the neck. The part that attaches the tooth to the periodontal ligaments and then to the jawbone (maxilla or mandible) is the root.
The outer part of the tooth, forming the occlusal surface and all four sides of the tooth, is the enamel, made up of the mineral’s calcium phosphate and calcium carbonate. Enamel is harder than bone, because it is almost all mineral with little organic matrix.
Deep to the enamel is dentin, which forms the bulk of the tooth. It is also harder than bone, but not as hard as enamel. Also, dentin contains dentinal tubules which allow fluid to move. Normally, the enamel covers dentin and keeps fluid from moving. When the dentin is exposed, fluid can move (as if the dentinal tubules are tiny drinking straws) and the nerves of the root send a strong pain signal to the brain.
The dentin of the root is covered by cementum and is connected to bone by a series of periodontal ligaments, a dense fibrous connective tissue. The periodontal ligaments have proprioception (i.e. pressure receptive nerves) and are resistant to anesthesia, which is why we can feel the pressure on our teeth during dental procedures even when the pain fibers are anesthetized.
The pain fibers and blood vessel are enclosed in the pulp cavity, a chamber formed by dentin with one to three outlets (apical foramina), one for each tooth root. Remember from the nervous system units that the pain signals carried by these nerve fibers are carried on the trigeminal nerve (cranial nerve V).
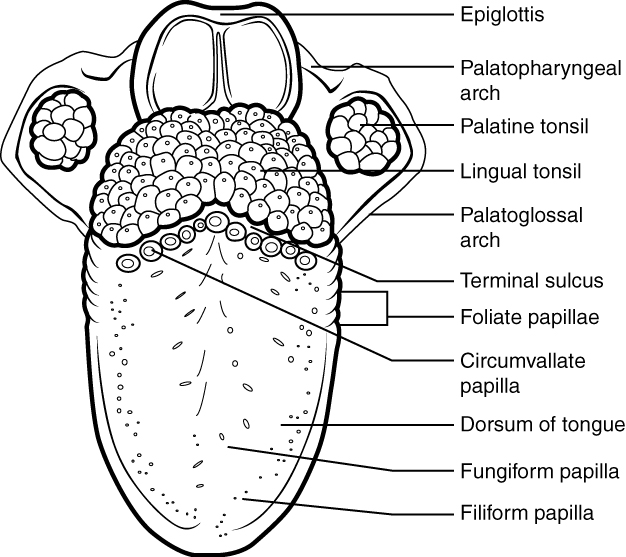
The tongue forms the floor of the oral cavity. It is made up of skeletal (voluntary) muscle covered by an epithelium.
The surface of the tongue has a characteristic roughness, because of four types of small elevations (Latin papilla, “nipple”, pl. papillae).
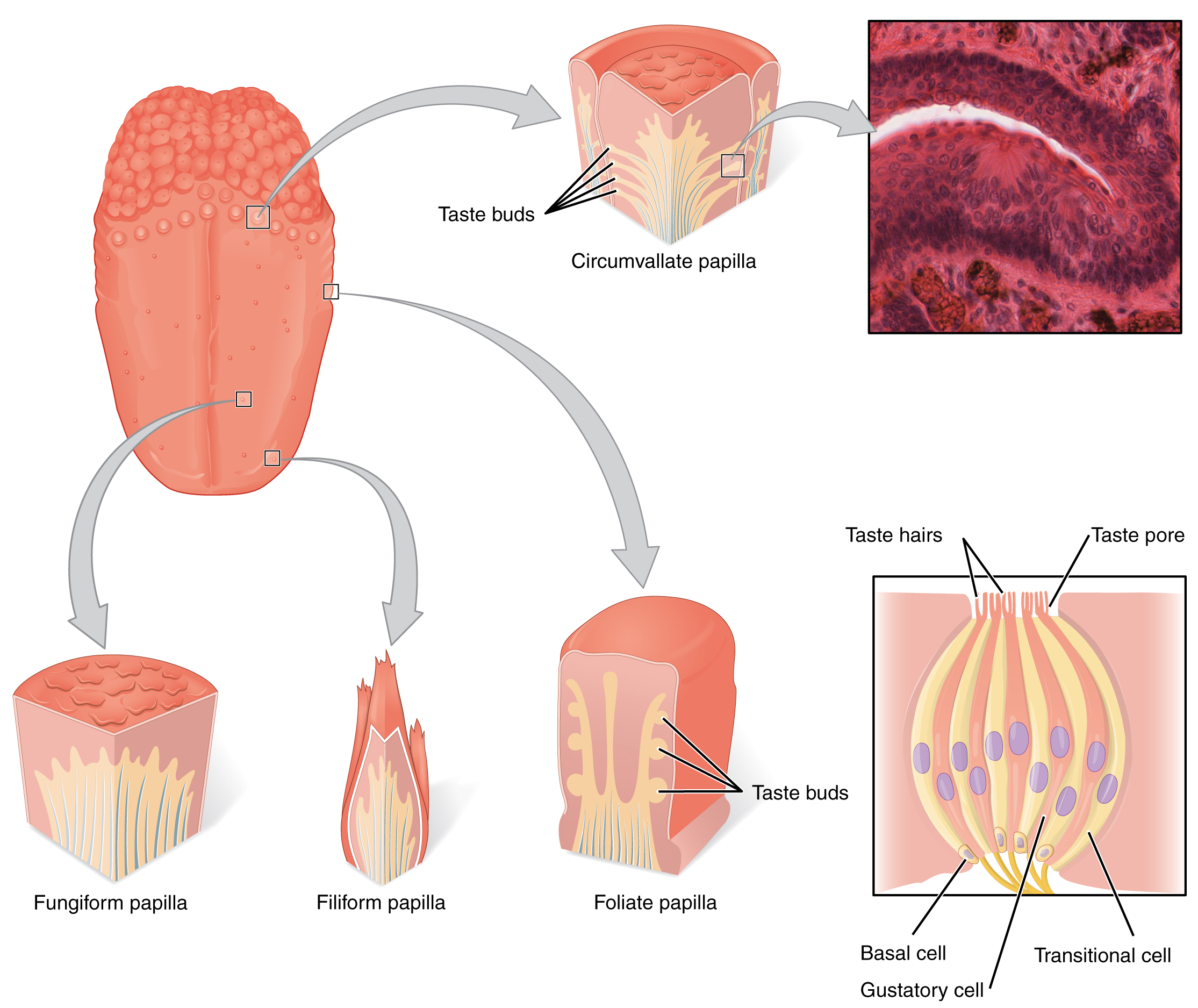
Filiform papillae, which look like little threads (Latin filum, “thread”) cover most of the tongue surface. These are non-taste structures that give the tongue a rough texture.
Gustatory receptor cells are clustered in taste buds. Taste buds are scattered over the surface of the oral cavity, but are found on the tongue in three groupings:
- Fungiform papillae (Latin fungus, “mushroom”) as the name suggests, look like little mushrooms.
- Foliate papillae (Latin folium, “leaf”) are leaf-shaped papillae found along the lateral surface of the posterior tongue.
- Vallate (or circumvallate) papillae (Latin vallatus, “surrounded by a wall”) form a V-shaped row along the posterior tongue. There are usually 7-12 of these, and it’s easier to see them on a friend’s tongue than on your own.
The tongue also has a set of lingual glands, which secrete mucus plus an enzyme, lingual lipase, which helps break down fatty foods in the mouth.
Saliva (“spit”) is secreted by specialized glands called salivary glands. Saliva plays an important accessory role in digestion, ensuring that food is pre-digested and soft before it is swallowed. Saliva also has an important role in defending the GI tract from microbial invaders.
There are three major salivary glands presented here, and a group of minor glands (labial, buccal, palatal, lingual) that we won’t discuss beyond the sentence you just read.
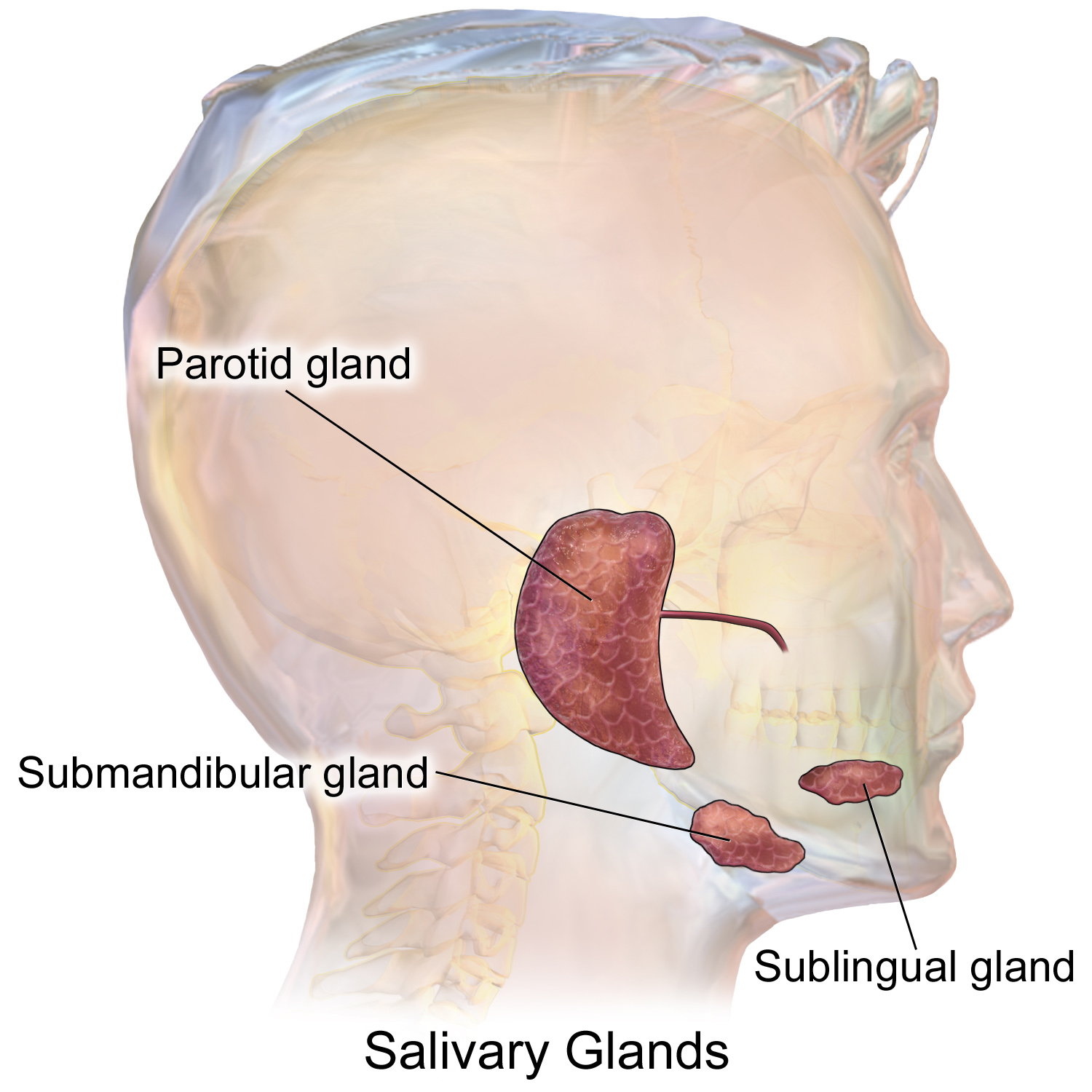 The major salivary glands, their locations, and their ducts, are:
The major salivary glands, their locations, and their ducts, are:
- parotid gland — the largest gland, inferior and anterior to the ears, parotid duct;
- sublingual gland — beneath the tongue, lesser sublingual ducts;
- submandibular gland — floor of the mouth medial and inferior to the mandible, submandibular ducts.
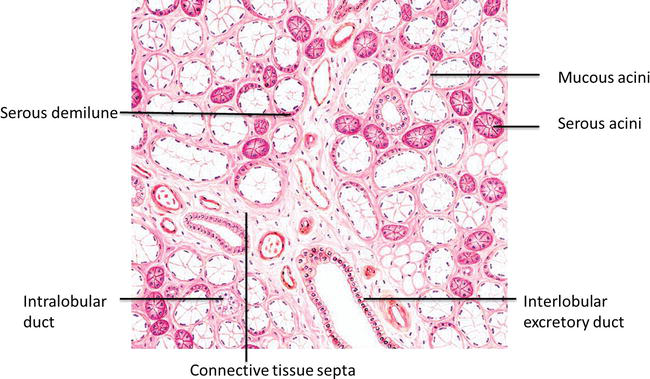
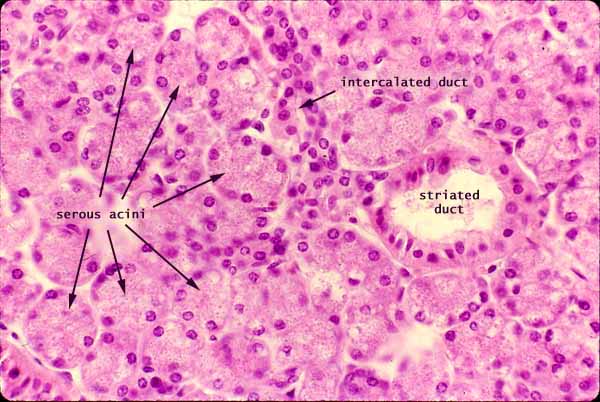
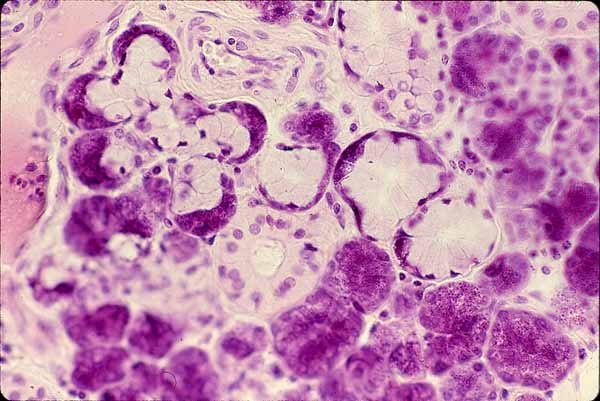
Microscopically, there are two kinds of acini (cell groupings; sing. Latin acinus, “berry”) found in the salivary glands. Mucous acini make mucus. Serous acini make enzymes in a watery fluid. Saliva is almost all water (99.5%). The remaining 1/200 of saliva is mucus and enzymes.
Enzymes in saliva include:
- Lysozyme — which breaks down invading microbes
- Immunoglobulin A (IgA) — recall from Unit 15 that IgA is the immunoglobulin found in the body’s secretions
- Salivary amylase (Latin amylum, “starch”) — this enzyme begins the breakdown of starchy foods into sugars, which is why starchy foods (such as potatoes) taste sweet, even though they have little free sugar; the sugar is released by salivary amylase.
The three main salivary glands differ slightly in their secretions. We can describe these in terms of being “watery” or “mucus–y” or a combination. The parotid gland is a “watery” secretion. The sublingual gland is a “mucus-y” secretion. The submandibular gland is a combination of the two types of secretions.
The Pharynx
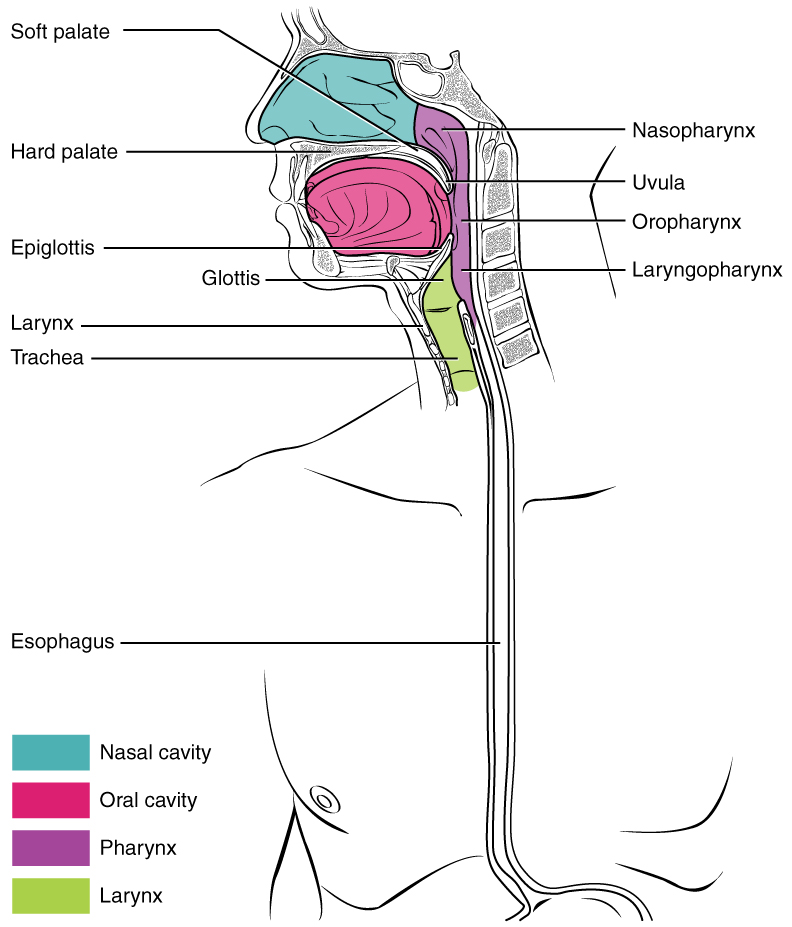
The pharynx is the point of transition between the oral cavity and esophagus. It is divided into three parts, which we studied in the respiratory system. We will recap that information here.
The nasopharynx connects the paranasal sinuses to the pharynx, allowing air to pass from the nose to the trachea.
The crowning achievement of Little Brotherhood is to make milk come out your sister’s nose at the dinner table with a well-timed joke. This is possible because of the nasopharynx. In this case, the mouth is closed to swallow. Air rushing out of the lungs to create a laugh forces the epiglottis into a position that closes off the esophagus. The liquid present in the mouth, having nowhere else to escape, is forced through the nasopharynx and out the nostrils.
The oropharynx joins the nasal cavity and oral cavity to the gut tube and trachea.
The laryngopharynx, as the name suggests, is adjacent to the larynx (“voicebox”). Here, the epiglottis covers the trachea when swallowing food or drink, and covers the esophagus when breathing. Think of the epiglottis as a kind of “sorting paddle” that determines whether a substance is gas (goes to the trachea) vs. liquid or solid (goes to the esophagus).
The Esophagus
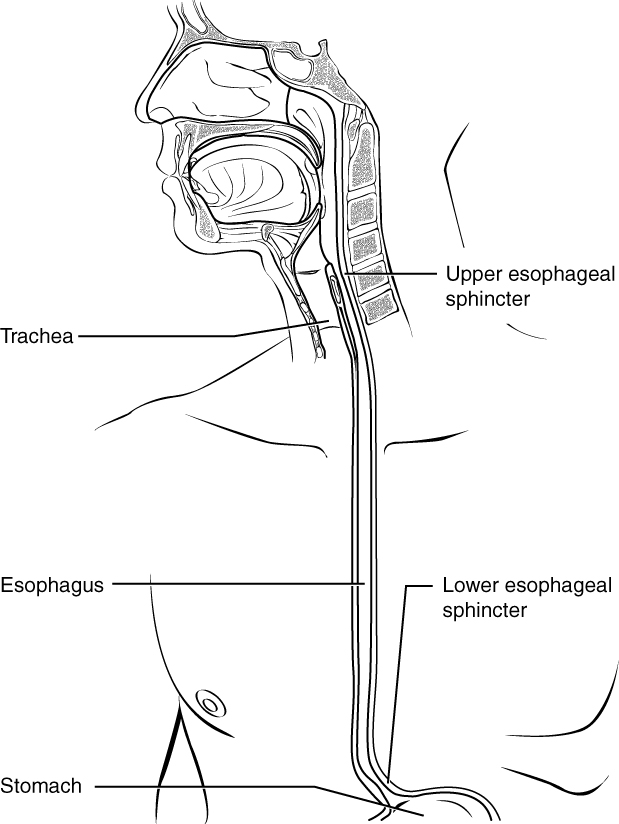
After food and drink pass through the laryngopharynx, the next part of the GI tract they encounter is the esophagus, a muscular tube located in the mediastinum of the thorax.
The esophagus is where we first encounter the general structure of the gut tube that we presented earlier. Remember that the gut tube has four layers (from the lumen out): mucosa, submucosa, muscularis, serosa.
Because the esophagus is simply a muscular tube that moves food from the pharynx to the stomach, it doesn’t have an absorptive surface. The epithelial sublayer of the mucosa is a nonkeratinized stratified squamous epithelium. The muscularis mucosae of the mucosa is relatively thick.
The muscularis is thick and muscular. Like most parts of the gut tube, there are two layers in the muscularis: a circular layer that closes off the lumen when contracted; and a longitudinal layer that contracts in waves (peristalsis) to move things along.
The “valve” that allows substances to pass from the pharynx to esophagus is the upper esophageal sphincter. The “valve” between the esophagus and stomach is the lower esophageal sphincter.
The superior 1/3 of the esophagus is striated muscle under voluntary control; the lower 2/3 is smooth muscle under autonomic control. Interestingly, dogs have striated muscle all along the esophagus, which allows them to yak stuff up more easily.
Swallowing
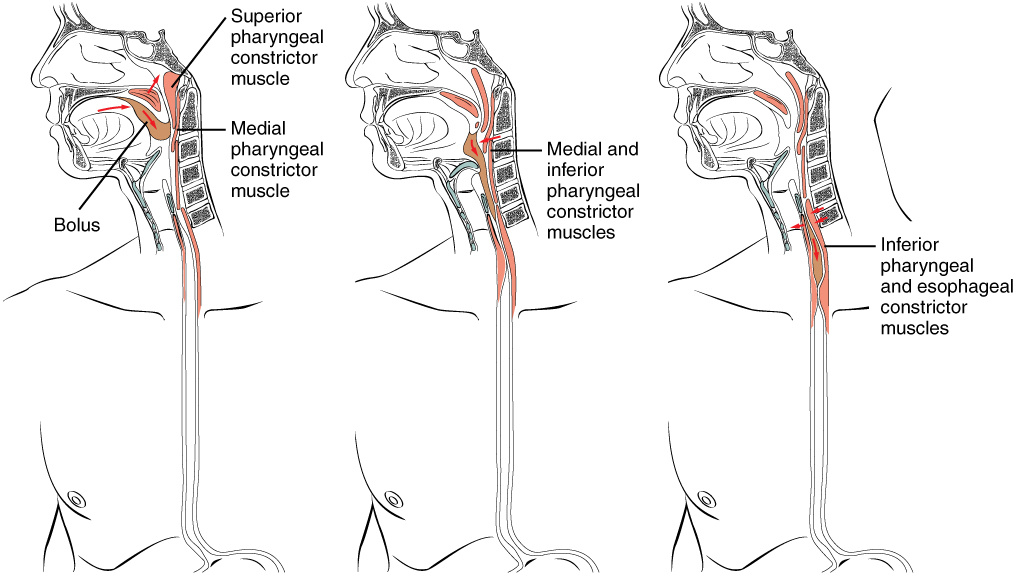
Now that we know the know the structures of the upper GI tract, we can explore the process of swallowing.
Deglutition is the process of swallowing. Remember that the pharynx and the first third of the esophagus is striated (voluntary) muscle.
Starting at about 1/3 of the way down the esophagus, smooth muscle takes over and the process is under autonomic control.
The process that moves food, later chyme, later feces, in the GI tract is called peristalsis.18-16
Swallowing has three phases:
- Voluntary — the stage we control consciously.
- Pharyngeal — when the bolus (Greek βωλος, “clod”) of food is in the oro– and laryngo- pharynx. This is the stage where food and water are kept out of the trachea.
- Esophageal — the upper esophageal sphincter opens, and the autonomic process of peristalsis begins.
Media Attributions
- U18-005 Upper GI © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter adapted by Justin Burr is licensed under a CC BY (Attribution) license
- U18-006 Oral Cavity © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U18-007 Teeth © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U18-008 Tooth Structure © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U18-009 Tongue © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U18-010 Taste Buds © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U18-011 Salivary Glands © BruceBlaus is licensed under a CC BY (Attribution) license
- U18-012 Serous Mucous Acini Salivary © Gupta, Sonia and Ahuja, Nitin is licensed under a CC BY (Attribution) license
- U18-013 Serous Acini © King, David G. is licensed under a CC BY (Attribution) license
- U18-014 Mixed Salivary Gland © King, David G. is licensed under a CC BY (Attribution) license
- U18-015 Pharynx © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U18-016 Esophagus © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U18-017 Swallowing © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license

