Nephron Loop, Collecting Ducts, and Water Reabsorption
Objective 6
Describe the mechanisms used to maintain normal blood osmolarity. Trace the path filtrate takes on its way to the collecting ducts and explain what happens to the solute concentration in the process. Explain the purpose of the countercurrent multiplier and how it assists with water reabsorption. Describe urea recycling.
Water Balance in the Kidney
An individual’s intake and use of water can be variable throughout the day, but the total volume of fluid in the body remains fairly constant. To control intracellular and extracellular fluid balance the body uses the urinary system to excrete or conserve water and solutes. With fluid excess, the body will dump more water, making the urine more dilute. In times of dehydration, the body will conserve water, but still excretes excess solutes, thus forming more concentrated urine.
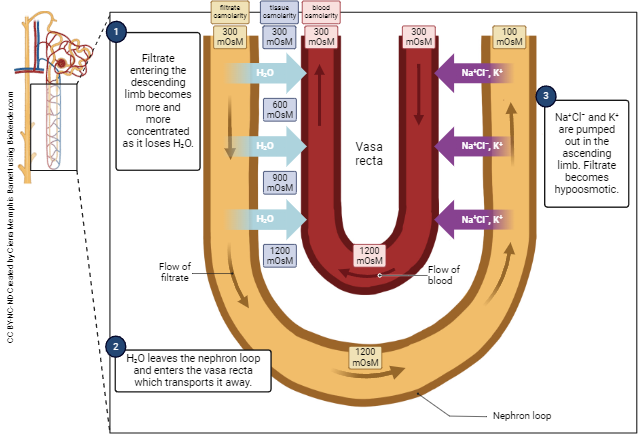
The unit, milliosmole per liter (mOsm/L), reflects the number of particles of any size in a solution. The total concentration of solutes in the blood is held constant at about 300 mOsm/L. The glomerular filtrate entering the proximal convoluted is also about 300 mOsm/L, but the concentration of the urine can vary between about 100 mOsm/L and 900 mOsm/L depending on the body’s needs.
The way the body works to conserve water during episodes of dehydration is a little more complex. It involves the creation of a solute concentration gradient in the interstitial space of the renal medulla, a process known as countercurrent multiplication. It also involves the reabsorption of water from this area back into the blood, a process called countercurrent exchange.
There are some important concepts to know in order to understand these two mechanisms. First, they are called “countercurrent” mechanisms because the fluids are flowing in opposite directions. This can get a little complicated because it can refer to filtrate flowing down the descending limb of the nephron loop and then back up the ascending limb, but can also refer to the way blood in the vasa recta flows around the nephron loop. The specific flow of both filtrate and blood contributes the water conservation occurring in and around the nephron loop.
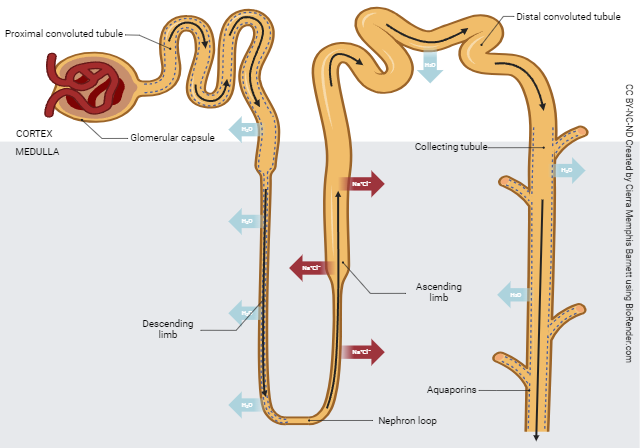
Changing the type of cells that line different parts of the nephron loop creates an interstitial concentration gradient in the medulla. This is the countercurrent multiplier.
Countercurrent Multiplier
After leaving the glomerulus, the filtrate becomes progressively more concentrated the deeper it goes into the medulla. This is because the descending limb of the nephron loop is not permeable to solute, is permeable to water, and the surrounding interstitial area has an increasingly higher solute concentration. Thus, water passes out of the filtrate as it flows down the descending limb. Simple osmosis is at work here. As water leaves, the filtrate can reach a concentration of more than 1000 mOsm/L. That’s three to four times the normal concentration of the blood.
The cells of the ascending limb of the nephron loop actively transport solutes into the interstitial space, but the ascending limb is not permeable to water. Because solutes are leaving the filtrate but water is not, it becomes less concentrated (more dilute) as it flows up the ascending limb. The concentration here can get as low as 50 mOsm/L.
As the filtrate moves through the distal convoluted tubule and into the collecting ducts, even more water (and solutes to some degree) can be reabsorbed. Hormones, like ADH, can cause the insertion of aquaporin channels that allow water to leave the tubules and move into the salty interstitial space where it can be picked up by the capillaries that surround the loop and tubules. The final product is a urine concentration that can range from 100mOsm/L to 900 mOsm/L. This wide range illustrates how the kidneys work to maintain homeostasis in the blood by using the urine as a way to dump what isn’t needed or is in excess.
Another tricky, but useful thing happens at the nephron loop. About half of the urea, which is a waste product from the breakdown of nitrogen containing compounds like proteins and ammonia, is reabsorbed. You should be asking yourself why the body would reabsorb a waste product. The reason is due to the osmotic pull urea has on water. As urea leaves the nephron loop, water chases it. The urea is then reabsorbed along with the tag-along water. Eventually the urea will make it back to the nephron loop where it will be allowed to pass through and be dumped in the urine or perhaps will be reabsorbed again to facilitate even more water reabsorption. This is why we refer to the process as “urea recycling.”
To summarize, as filtrate moves down the loop, water leaves and some solutes come in, making the filtrate more concentrated. As the filtrate moves up, the solutes leave but the water stays in.
This creates a gradient in the interstium around the loop. The saltiness from the solutes leaving the ascending limb helps to pull the water from the descending limb. That is what is meant by countercurrent multiplier. The more solutes you have, the more that pass out into the tissue and the more the water is drawn out after them. Kinda magical, if you think about it.
Countercurrent Exchange
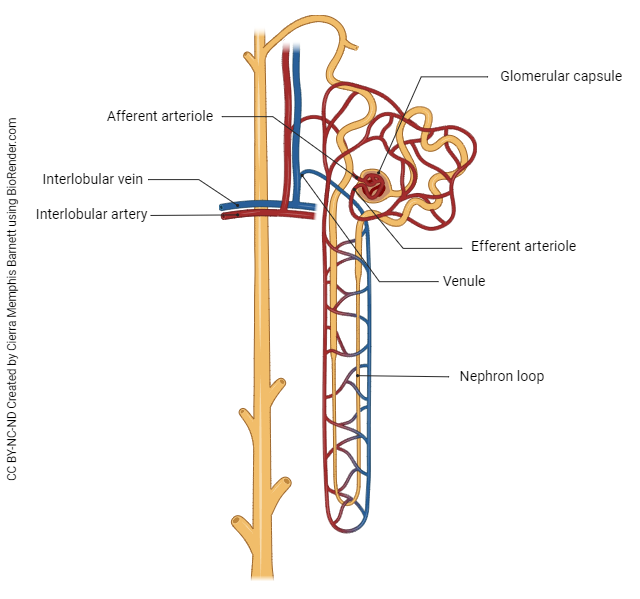
But the magic doesn’t stop there. Remember that the nephron is surrounded by a system of vessels called peritubular capillaries. The arrangement of peritubular capillaries that dip into the medulla and surround the nephron loop is called the vasa recta. In addition to supplying the cells of the medullary space with nutrients and oxygen, the vasa recta facilitate easy reabsorption of water. Blood in the vasa recta flows parallel to the nephron loop, but in the opposite direction (counter-current).
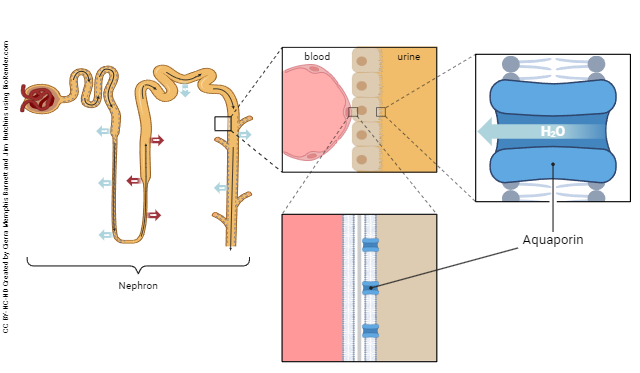
By running countercurrent to the flow of filtrate in the nephron loop, the vasa recta are able to pick up increased amounts of solutes on the ascending side of the nephron loop which facilitates increased reabsorption of water by osmosis on the descending side of the nephron loop. This exchange of water and solutes facilitated by the nephron loop and vasa recta is referred to as the countercurrent exchange. Hormones, like ADH, play an important role in this reabsorption. ADH causes the formation of aquaporin channels in the tubules, allowing water to move out into the area of tissue that is high in solutes. From there, it will be reabsorbed by the vasa recta, thus returning to the bloodstream.
Through these mechanisms, the kidneys are able to reabsorb an incredible amount of water without spending a lot of energy to do it. As a result, the body stays adequately hydrated while expelling unwanted solutes and waste products as urine.
Media Attributions
- U19-023 Countercurrent Exchange © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U19-024 Nephron and Blood Vessels © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U19-025 H20 and NaCl Exchange in Nephron © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U19-026 Aquaporins in Nephron © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license

