Motor Systems | Autonomic Motor
Objective 2
Describe the circuitry of the autonomic motor pathways.
General Features
Motor systems require an effector. The output of the nervous system is either contraction of a muscle or changing the secretion of a gland.
The somatic motor system (Objective 1) contracts skeletal muscle. The autonomic motor system (visceral motor system) contracts smooth muscle, contracts cardiac muscle, or changes the secretion of glands.
Remember from Unit 11 Objective 2 that the sympathetic and parasympathetic nervous systems have different anatomy. We will learn in this objective that they have different signaling molecules as well. Both pathways consist of two neurons: a preganglionic neuron, with its cell body in the central nervous system and its axon terminals in an autonomic ganglion; and a postganglionic neuron, with its cell body in an autonomic ganglion and its axon terminals sending a chemical signal to the effector organ (cardiac muscle, smooth muscle, or a gland).
Sympathetic Nervous System
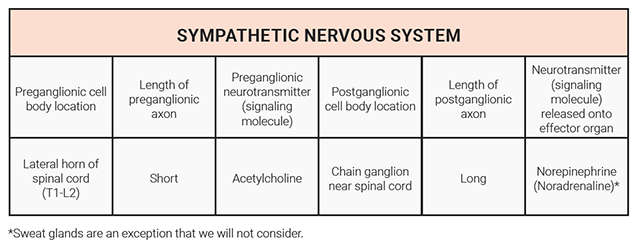
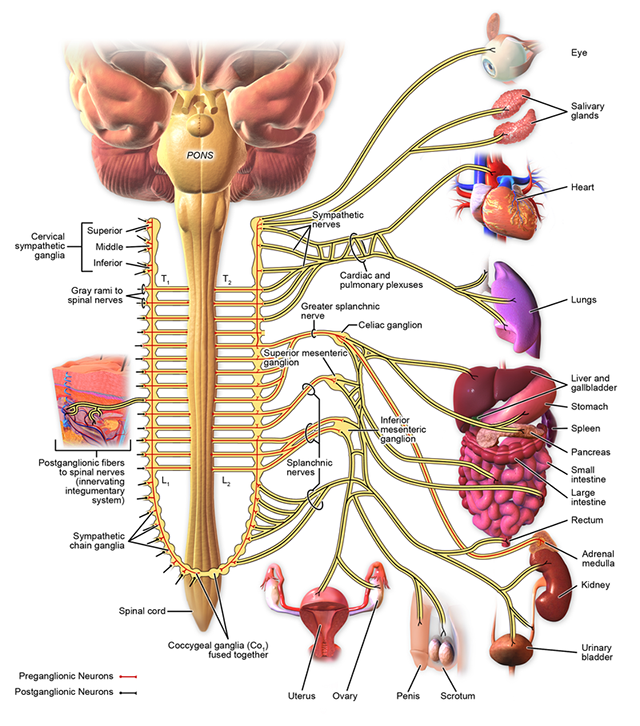
The sympathetic nervous system, sometimes called the “fight-flight-freeze” system, is tuned to activate the entire body at once. The preganglionic cell bodies are located in the lateral part of the gray matter at the first thoracic level (T1) through the second lumbar level (L2) of the spinal cord. These neurons send out short axons which enter the nearby sympathetic chain ganglia where they release acetylcholine onto the postganglionic neurons. The axon of the postganglionic neurons travels a long distance to the organs where it releases norepinephrine (noradrenaline) onto smooth or cardiac muscle.
 Let’s say a tiger entered the room where you were reading this. What would you need to do? Your pupils would dilate, your mouth would go dry, your heart rate would increase, the air passages of the lungs would dilate to take in more air, and you would sweat. All these functions are controlled by norepinephrine released from the postganglionic neurons of the sympathetic nervous system. At the same time, the digestive organs would shut down and as much blood as possible would be shunted to the skeletal muscles so you could run if needed.
Let’s say a tiger entered the room where you were reading this. What would you need to do? Your pupils would dilate, your mouth would go dry, your heart rate would increase, the air passages of the lungs would dilate to take in more air, and you would sweat. All these functions are controlled by norepinephrine released from the postganglionic neurons of the sympathetic nervous system. At the same time, the digestive organs would shut down and as much blood as possible would be shunted to the skeletal muscles so you could run if needed.
The response of the nervous system generally is too quick and transient to run for very far or for very long. The sympathetic nervous system also stimulates a gland on top of the kidney, the adrenal medulla, to release epinephrine (adrenaline) which travels in the bloodstream and activates the same receptor as norepinephrine.
Noradrenaline or norepinephrine? Adrenaline or epinephrine?
You might have noticed, and been confused by, the interchangability of the terms “adrenaline” and “epinephrine” and the similar terms “noradrenaline” and “norepinephrine“.
The “nor–” prefix is the easiest one to deal with. Adrenaline is made by adding a methyl (–CH3) group to noradrenaline.
Both noradrenaline and adrenaline bind to the same receptor, called the adrenergic receptor.
In general, noradrenaline is used as a neurotransmitter, released from noradrenergic neurons. In general, adrenaline is a hormone, released into the bloodstream from the adrenal medulla.
Adrenaline is chemically identical to the signaling molecule epinephrine. Thus, in clinical practice, we use an “EPIPEN®” which is a trademarked name for an autoinjector syringe loaded with epinephrine. The EPIPEN® is used to treat a life-threatening allergic reaction called anaphylaxis which we’ll discuss further in Unit 15.
How did we get in this situation? No one knows, and no one seems to be able to do anything about it. The terms mean the same thing (ad– and epi– mean “on top of”; renal and nephr are root words which both mean kidney). Apparently, a group of scientists refused to adopt the other group’s preferred name at the beginning of the 20th century so the name used depends on which group you affiliated with.
Adrenaline = epinephrine
Noradrenaline = norepinephrine
Both signaling molecules act at adrenergic receptors
Parasympathetic Nervous System
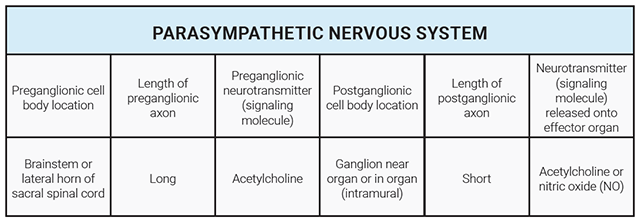
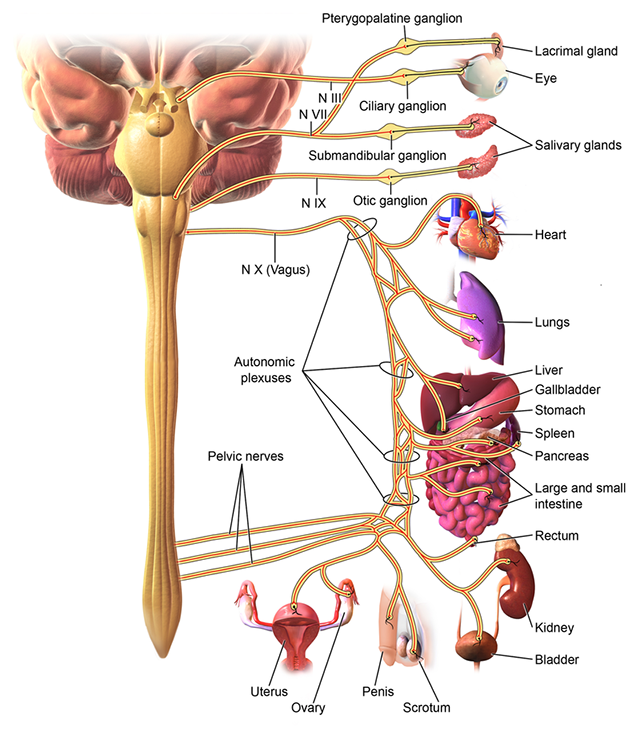
The anatomy, and therefore the physiology, of the parasympathetic nervous system is completely different. There is a long preganglionic neuron whose axon goes directly to the organ and a short postganglionic axon with the neuronal cell body generally found in the wall of the organ. The postganglionic neurons are found in clusters called intramural (“inside the wall”) ganglia. This allows the parasympathetic nervous system to control its targets organ-by-organ rather than bodywide.
The preganglionic cell bodies for head, thoracic, and abdominal organs are found in the brainstem. Their axons travel in a cranial nerve (for the head) or in the vagus nerve (for the thorax and abdomen). Recall that the tenth cranial nerve is called the vagus nerve because it wanders all over the thoracic and abdominal cavities. As it wanders, it releases acetylcholine on the intramural ganglion neurons.
The preganglionic cell bodies for abdominal, retroperitoneal, and genital regions are found in the sacral spinal cord. They form pelvic splanchnic nerves which go to the digestive organs (abdominal), kidneys (retroperitoneal), bladder, and genitals.
The postganglionic neurons have cell bodies in the intramural ganglia. Their axons release acetylcholine, but this time, the same neurotransmitter acts on a different type of receptor, called the muscarinic acetylcholine receptor. We will take a closer look at this receptor in Unit 13.
The parasympathetic nervous system is sometimes called the “rest and digest” system.
Compare and Contrast Sympathetic vs Parasympathetic Nervous Systems
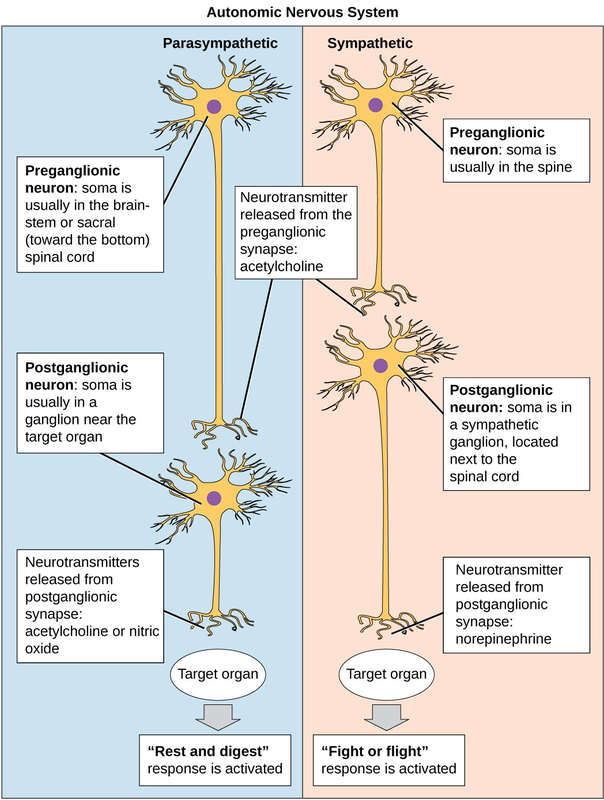
This diagram summarizes the features of the sympathetic and parasympathetic nervous system that we have discussed to this point.
Innervation of the Heart
Let’s turn to a specific and important example: the innervation of the heart.
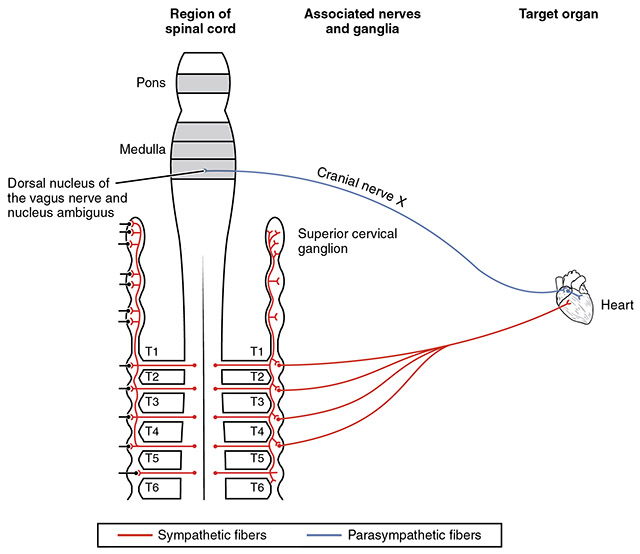
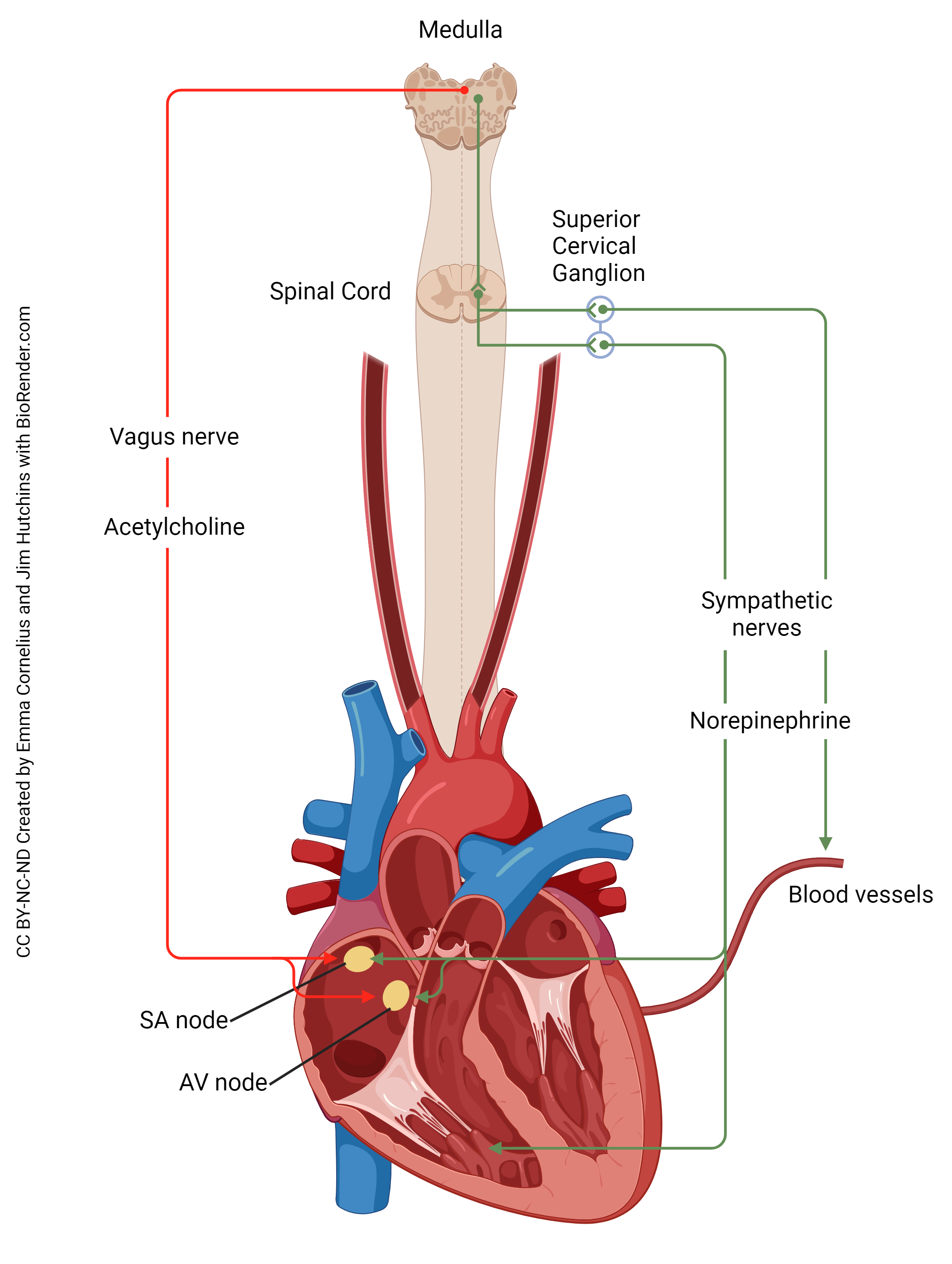
Recall that cranial nerve X, the vagus nerve, is named this because it wanders all over the thoracic and abdominal cavities. Therefore, cell bodies of the parasympathetic nervous system which innervate the heart are located in the dorsal motor nucleus of the vagus and their axons travel through the vagus nerve to reach the heart. Parasympathetic (“rest and digest”) action is to slow the heart, and it does this by releasing acetylcholine onto the pacemaker cells in the heart that we will study in Unit 16.
For the sympathetic innervation of the heart, preganglionic cell bodies are found in the lateral horn of the spinal cord (green region of the diagram) at upper thoracic levels (there is some variability, but T1-T5 would be a good estimate). These send out axons which synapse in the T1-T5 sympathetic chain ganglia but also in some chain ganglia not directly linked to the spinal cord: the superior cervical ganglion, middle cervical ganglion, and inferior cervical ganglion. All these ganglia contain postganglionic cell bodies of neurons whose axons travel in the cardiac accelerator nerve to the pacemakers of the heart, where they release norepinephrine (noradrenaline) to speed up the heart. This is exactly what you want to do in a sympathetic (“fight or flight”) response.
Innervation of the Iris: Controlling Pupil Size
We’ll take a detailed look at another organ, the iris (colored part of the eye) which defines a hole in the middle called the pupil. As you’ve probably discovered, the pupil gets larger and smaller in response to light (reaction) but also in response to focusing (accommodation) and emotional events.
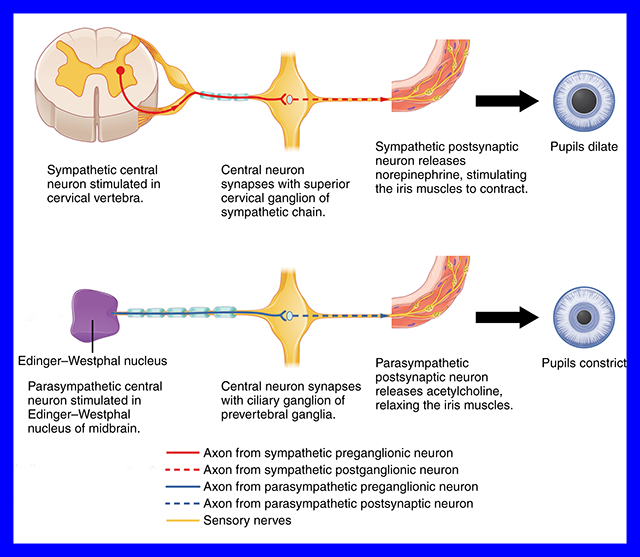
The sympathetic nervous system causes the pupil to dilate. You can easily confirm this by pissing off your cat or your partner. (Probably best not to piss off both at the same time.) The circuitry for this response is as follows:
- Preganglionic neurons are found in the lateral horn of the upper thoracic spinal cord
- Their axons release acetylcholine onto cells in the superior cervical ganglion
- The postganglionic axons take an ill-defined, meandering course along blood vessels to the oculomotor nerve (CN III)
- The axon terminals release norepinephrine (noradrenaline) onto the iris dilator muscle, smooth muscle fibers that run radially in the iris to cause it to enlarge the pupil (mydriasis)
For the parasympathetic innervation of the iris:
- Preganglionic neurons are found in the midbrain
- Their axons release acetylcholine onto cells in the ciliary ganglion, near the eye
- The postganglionic axons travel in the oculomotor nerve (CN III) a short distance to reach the iris
- There, they release acetylcholine onto the iris sphincter muscle, smooth muscle fibers which run circumferentially around the rim of the pupil and cause it to shrink (miosis)
 In medieval Italy, women got the idea that men were so stupid that they could be made to fall in love with you just because your pupils were dilated — and therefore men responded to simple autonomic responses indicating the woman was actually, you know, interested in what he had to say. To achieve this state, they would take a drug called belladonna, extracted from the deadly nightshade Atropa belladonna. (“Belladonna”, in Italian means literally, “beautiful woman” even if she’s not named “Donna”.)
In medieval Italy, women got the idea that men were so stupid that they could be made to fall in love with you just because your pupils were dilated — and therefore men responded to simple autonomic responses indicating the woman was actually, you know, interested in what he had to say. To achieve this state, they would take a drug called belladonna, extracted from the deadly nightshade Atropa belladonna. (“Belladonna”, in Italian means literally, “beautiful woman” even if she’s not named “Donna”.)
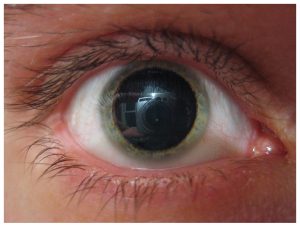 You probably figured out already how dangerous this is, because we call the plant the deadly nightshade after all. It’s much safer to use a purified form of belladonna called atropine. Atropine is in everyday use in the clinic. For example, you’ve probably been given atropine eye drops to dilate your pupils during an eye exam. Atropine is also used to regulate the heartbeat. Now we understand how this works: atropine blocks the receptors for acetylcholine in the heart, causing it to speed up. Atropine also blocks the receptors that make the pupil small in the iris sphincter muscle, causing it to become bigger.
You probably figured out already how dangerous this is, because we call the plant the deadly nightshade after all. It’s much safer to use a purified form of belladonna called atropine. Atropine is in everyday use in the clinic. For example, you’ve probably been given atropine eye drops to dilate your pupils during an eye exam. Atropine is also used to regulate the heartbeat. Now we understand how this works: atropine blocks the receptors for acetylcholine in the heart, causing it to speed up. Atropine also blocks the receptors that make the pupil small in the iris sphincter muscle, causing it to become bigger.
Media Attributions
- U12-018 Table of Autonomic Locations Sympathetic v2 © Hutchins, Jim and Bizzell, Lizz is licensed under a CC BY-SA (Attribution ShareAlike) license
- U12-019 Sympathetic Innervation © BruceBlaus is licensed under a CC BY (Attribution) license
- U12-019a Shita and Her New Tiger Friends Attack © Lie, Haakon is licensed under a CC BY-ND (Attribution NoDerivatives) license
- U12-020 Table of Autonomic Locations Parasympathetic v2 © Hutchins, Jim and Bizzell, Lizz is licensed under a CC BY-SA (Attribution ShareAlike) license
- U12-021 Parasympathetic Innervation © BruceBlaus is licensed under a CC BY (Attribution) license
- U12-022 Sympathetic vs Parasympathetic © CNX OpenStax is licensed under a CC BY (Attribution) license
- U12-026 Heart Autonomics © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U12-025 Autonomic Innervation of the Heart v2 2172 px © Cornelius, Emma and Hutchins, Jim is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U12-027 Pupil Autonomics © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter adapted by Jim Hutchins is licensed under a CC BY (Attribution) license
- U12-028 Belladonna © Plbmak is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U12-029 Mydriasis © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter adapted by Jim Hutchins is licensed under a CC BY (Attribution) license

