Histology of Arteries and Veins | Starling’s Law of the Capillary
Objective 5
Relate the histology of blood vessels with their location and function. Explain how the structure of capillaries and the pressure differences within the capillaries results in the delivery of nutrients on the arteriole side and absorption of wastes on the venule side.
Histology of the Arteries and Veins: The Tunics
In keeping with their discrete functions — arteries carry blood away from the heart, veins carry blood towards the heart — arteries and veins have different structural features.
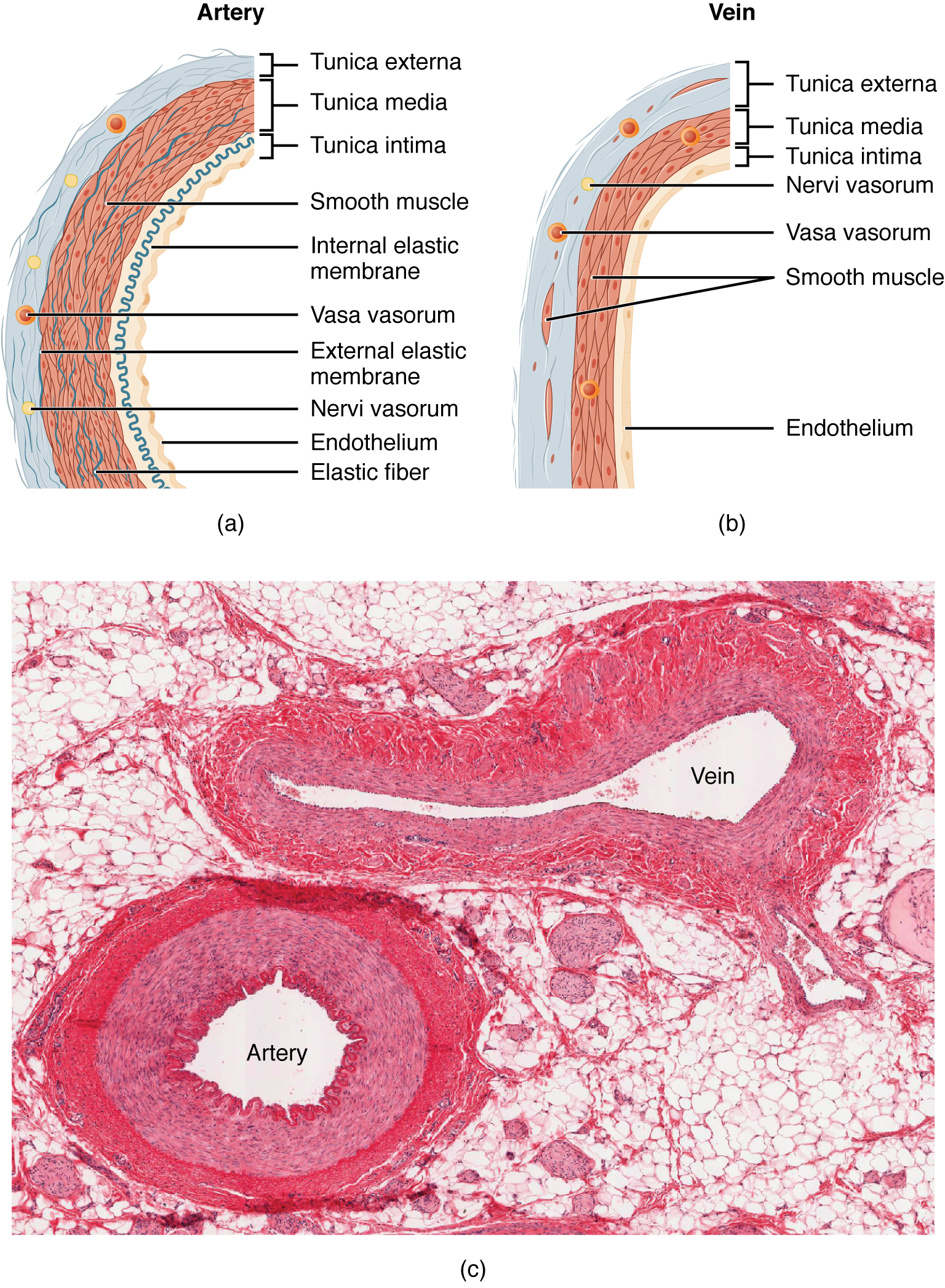
Arteries carry blood under extremely high pressures, as high as 200 mm Hg or more under certain circumstances. Accordingly, they have a thick smooth muscle layer (tunica media) which allows them to resist pressure. The largest arteries (elastic arteries) have, as the name tells us, fibers made of the protein elastin in the tunica media. The innermost layer of an artery is called the tunica intima (from the same root as the word “initimate”). The external, outermost layer of an artery is called the tunica externa.
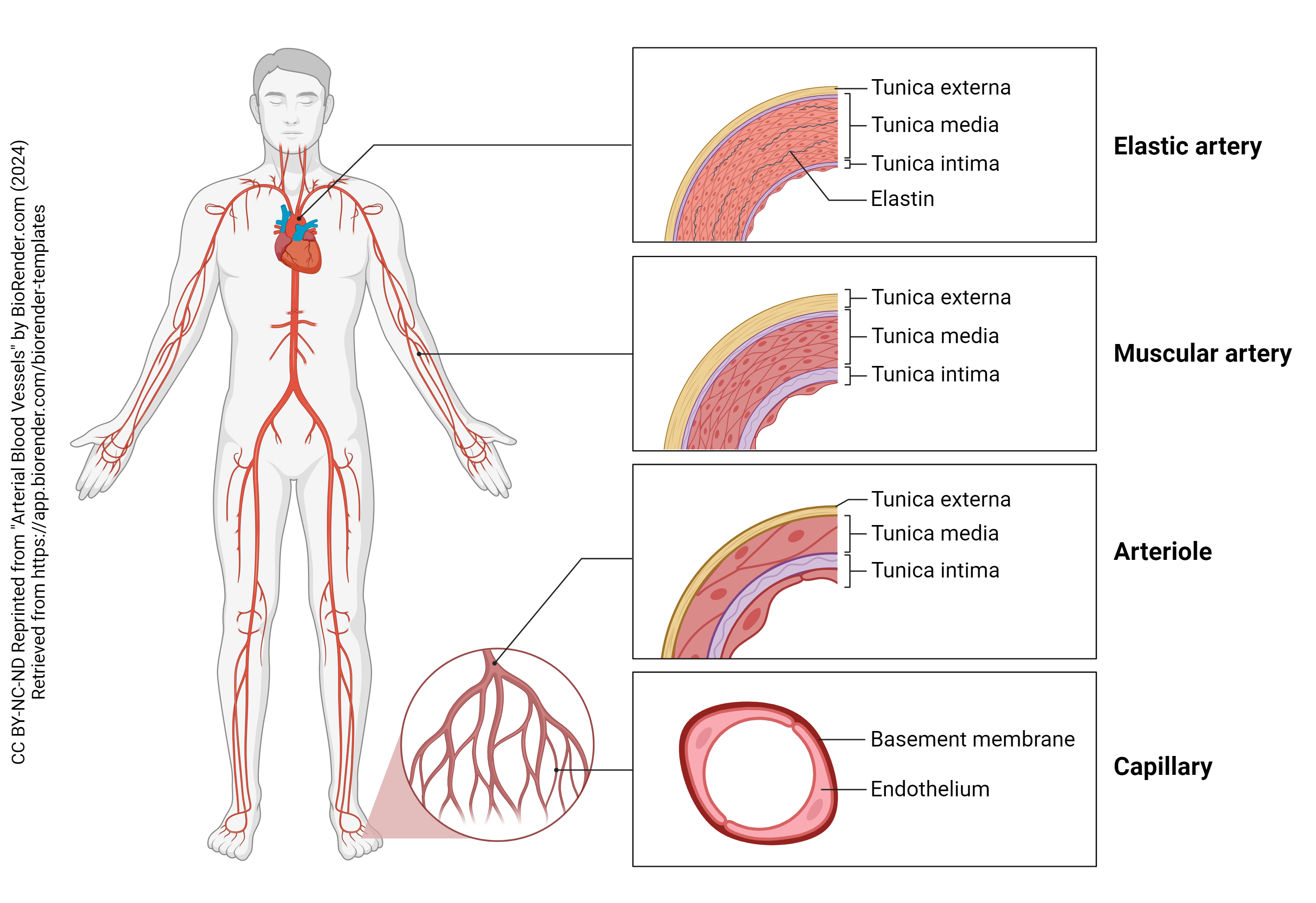 Arteries can change their diameter when responding to changing conditions. In a way, we knew this already, because the sympathetic nervous system directs blood flow to the heart, lungs, and skeletal muscles while the parasympathetic nervous system directs blood flow to the digestive organs. Even at the very end of the arterial tree, in the small arterioles, there are mechanisms for directing blood flow where it is needed. This is the basis for the technique functional magnetic resonance imaging (fMRI): when a part of the brain is doing calculations, that part receives more blood supply than the parts of the brain with lower metabolic activity.
Arteries can change their diameter when responding to changing conditions. In a way, we knew this already, because the sympathetic nervous system directs blood flow to the heart, lungs, and skeletal muscles while the parasympathetic nervous system directs blood flow to the digestive organs. Even at the very end of the arterial tree, in the small arterioles, there are mechanisms for directing blood flow where it is needed. This is the basis for the technique functional magnetic resonance imaging (fMRI): when a part of the brain is doing calculations, that part receives more blood supply than the parts of the brain with lower metabolic activity.
Regulating Capillary Blood Flow
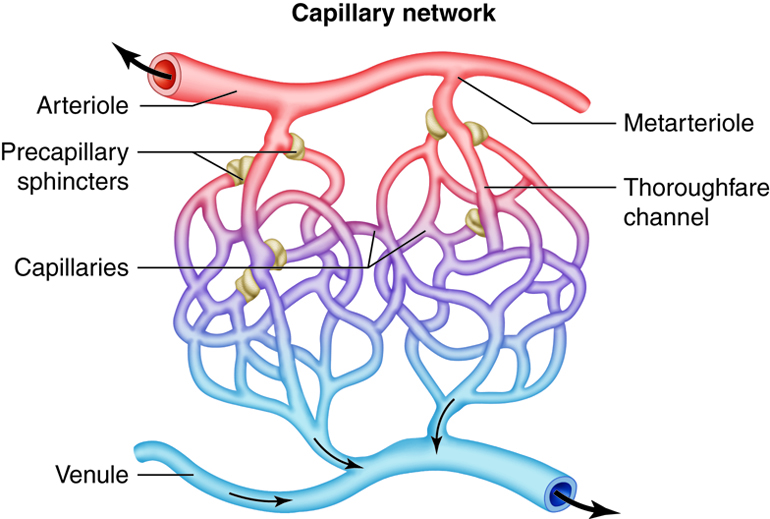
Arterioles meet venules (the smallest part of the venous network) at capillaries. Capillaries are the site of oxygen and glucose diffusion into tissue cells, and the diffusion of waste products into the blood to be carries to the liver, kidneys, and other organs that detoxify the blood.
This capillary exchange is regulated by controlling blood flow into the capillaries. Controlling blood flow is the job of smooth muscle collars called precapillary sphincters, which respond to chemicals released by increased metabolism. When the tissue “gets busy”, that means it needs more oxygen and glucose, and it makes more waste. The precapillary sphincters open up to allow more blood flow and more nutrient and waste exchange.
Histology of the Capillaries
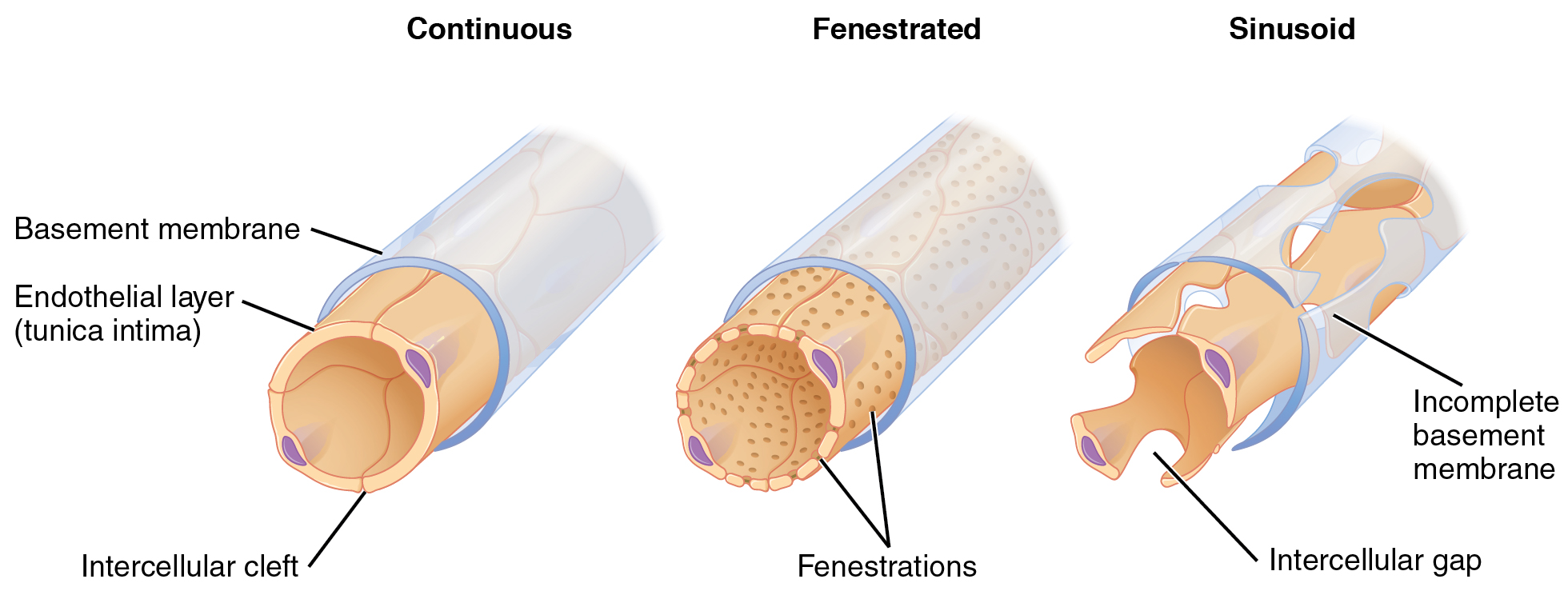
There are at least three kinds of capillaries which differ in the structure of the tunica intima (endothelial cell layer).
Continuous capillaries have tiny intracellular clefts that don’t let anything bigger than a hormone through. Water, glucose, and gases can also pass through these tiny openings. These are found in the brain, skin, and lungs. As we have seen already, in the brain, there is a tight regulation of what can go in and out of the capillary. Recall that the continuous capillaries and astrocyte end-feet form the blood-brain barrier which doesn’t even let most molecules through. Only gases, glucose, neurotransmitter precursors, and amino acids are allowed through the blood-brain barrier. In the skin, white blood cells have to force their way through the clefts to get into the connective tissue to defend the body. As monocytes squeeze through the capillaries in the skin and connective tissue, they transform into macrophages. Neutrophils also squeeze through these tiny spaces when called by chemical signals: pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs). In the lungs, continuous capillaries need only let oxygen and carbon dioxide pass to perform their critical exchange function.
Fenestrated capillaries are found in the filtration part of the kidney; in the intestines; in the pancreas; and in some endocrine glands. The Latin word fenestra means “window” and these little windows let larger molecules pass without restriction. For example, in the part of the kidney called the glomerulus, the fenestrated capillaries keep cells from moving out of the capillary but allow larger molecules to pass freely through the basement membrane and the kidney podocytes that support the filtration system structurally. Along with cells, albumin and other medium- and large-sized proteins are held back by this system.
Sinusoidal capillaries are in your liver, spleen, lymph nodes, bone marrow and endocrine glands. In these organs, we want cells to be able to move freely from the inside to the outside of the capillary. For example, the liver and spleen examine red blood cells and destroy them if they are over three months old. Dendritic cells bring signals from the “war zone” to the “ready room” inside the lymph nodes and recruit T lymphocytes to begin an adaptive immune response. Newly-created cells in the bone marrow, the product of hematopoiesis, must be able to make it into the bloodstream.
Review of Pressures in the Systemic Circuit
Recall that in Objective 3 we ended with a discussion of how pressure varies in different parts of the systemic circuit. In order to understand how capillaries work, we need to revisit that concept.
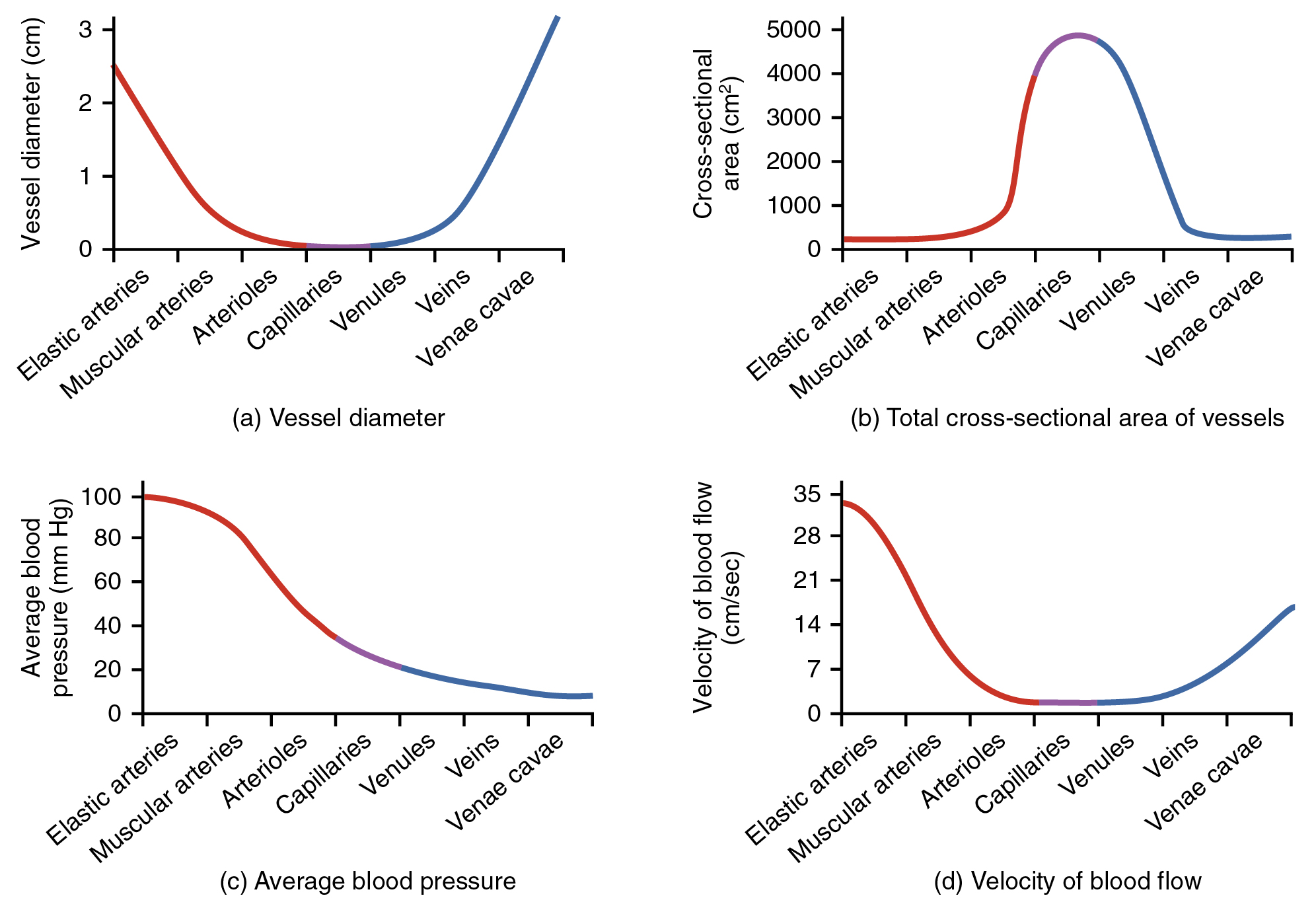 Vessel diameter varies through the systemic circuit (panel a). The aorta is of course the biggest artery of the body, and as it begins to branch, its branches get progressively smaller. Finally, as an arteriole narrows to become a capillary, it reaches its smallest diameter, about 8-10 μm. The red blood cell (RBC), at 7-8 μm diameter, is a tight fit! Sometimes, RBCs must fold to get through a capillary, which is where their biconcave disc shape comes in. As the RBC passes from the capillary into the venule, the size of the surround vessel becomes progressively larger, like rivulets feeding into creeks feeding into rivers, until the venae cavae which are slightly larger in diameter than the aorta.
Vessel diameter varies through the systemic circuit (panel a). The aorta is of course the biggest artery of the body, and as it begins to branch, its branches get progressively smaller. Finally, as an arteriole narrows to become a capillary, it reaches its smallest diameter, about 8-10 μm. The red blood cell (RBC), at 7-8 μm diameter, is a tight fit! Sometimes, RBCs must fold to get through a capillary, which is where their biconcave disc shape comes in. As the RBC passes from the capillary into the venule, the size of the surround vessel becomes progressively larger, like rivulets feeding into creeks feeding into rivers, until the venae cavae which are slightly larger in diameter than the aorta.
There’s only one aorta, and only two venae cavae, so they don’t have much total cross-sectional area (panel b). There are over 10 billion capillaries, and even though each individual one has a tiny cross-sectional area, the total of all of them adds up to a lot.
πr2 = area
radius = ½ x diameter
4 μm = 4 x 10–6 m is the radius of a single capillary
π x (4 x 10–6 m)2 = 5 x 10–11 m2 = 5 x 10–7 cm2 is the cross-sectional area of each capillary
(5 x 10–7 cm2) x (1010) = 5 x 103 cm2 = 5000 cm2 is the total cross-sectional area of all capillaries
Finally, velocity of blood flow (panel d) is not too interesting to us right now, so we’ll ignore it.
Starling’s Law of the Capillary
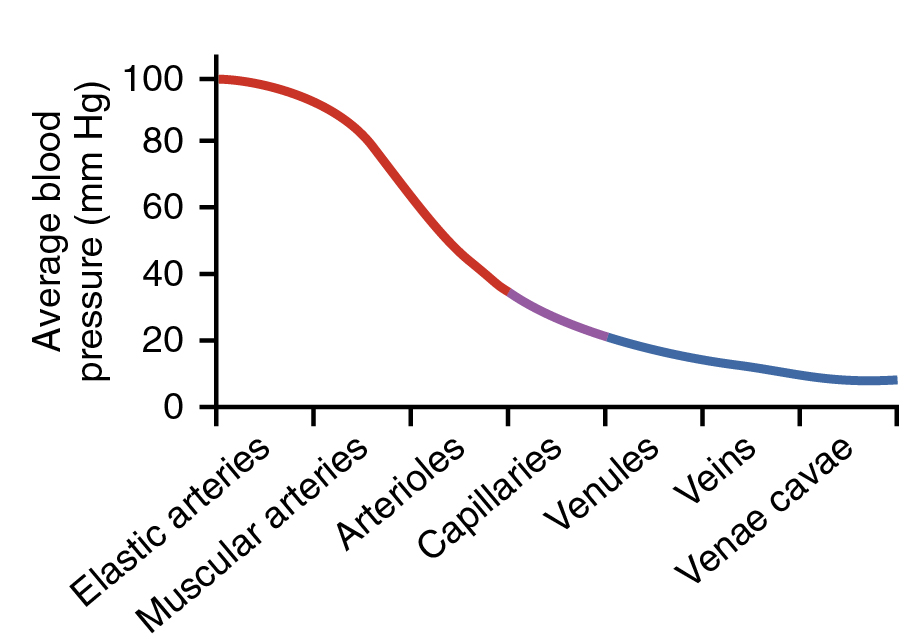 We do, however, want to focus on changes in blood pressure in the systemic circuit (panel c) because changes in blood pressure are going to be how capillaries work.
We do, however, want to focus on changes in blood pressure in the systemic circuit (panel c) because changes in blood pressure are going to be how capillaries work.
Note that because of a slight change in diameter, the pressure on the arteriole side of the capillary is about 35 mm Hg and the pressure on the venule side of the capillary is about 18 mm Hg. These pressures tend to push water out of the capillary, because the pressure outside the capillary is zero.
Recall from Units 2 and 4 that when water can move, and water is at higher concentration on one side of a semipermeable membrane, it creates an osmotic pressure which is the result of the net movement of water from where it’s at low concentration to where it’s at high concentration.
Albumin and other soluble proteins, which cannot move across the capillary membrane, reduce the water concentration inside the capillary. In the extracellular fluid surrounding the capillary, however, there is very little protein. That means water is at higher concentration in the extracellular fluid than in the capillary. The osmotic pressure does not change much, because this protein concentration does not change much, no matter where you are in the capillary. It stays a pretty constant 25 mm Hg pushing water into the capillary, unless something reduces the blood concentration of protein (e.g. starvation), in which case it drops, with disasterous effects on capillary exchange.
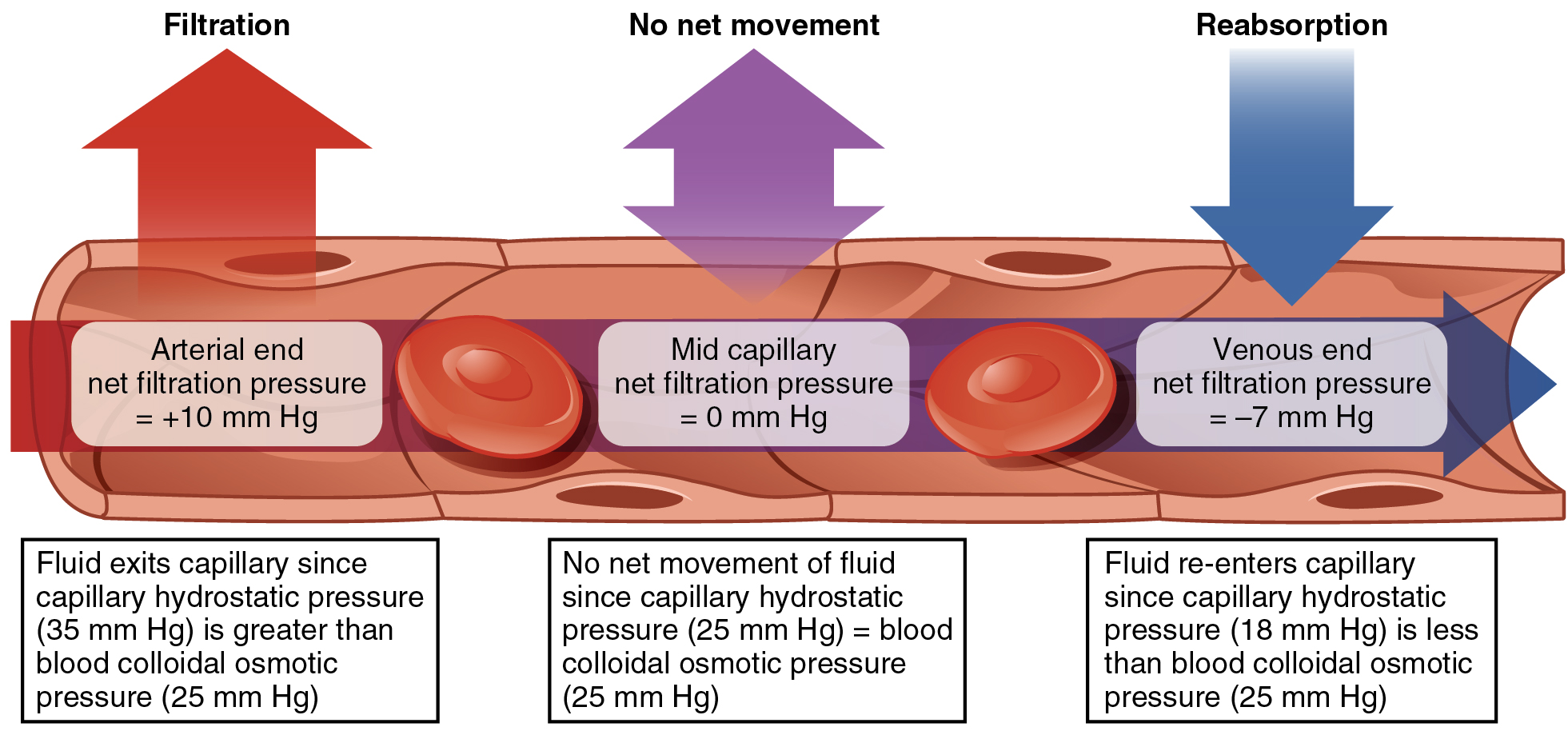
There are three scenarios here. Let’s take them one at a time.
On the arteriole side of the capillary, the hydrostatic pressure (i.e. the blood pressure) is about 35 mm Hg, pushing water and other small molecules out. The blood osmotic pressure is 25 mm Hg, pushing water and other small molecules in. The net pressure (35 out – 25 in) is 10 mm Hg out of the capillary.
In the middle of the capillary, the hydrostatic pressure is about 25 mm Hg. The blood osmotic pressure is still 25 mm Hg. The net pressure pressure (25 out – 25 in) is zero and nothing much moves here.
On the venule side of the capillary, the hydrostatic pressure is about 18 mm Hg. The blood osmotic pressure is still 25 mm Hg. The net pressure pressure (18 out – 25 in) is – 7 mm Hg (the minus sign indicates the pressure has reversed, and the net pressure pushes materials into the capillary).
Therefore, on the arteriole side, fluid (including oxygen and glucose) moves out of the capillary.
On the venule side, fluid (including H+, CO2, urea, and other wastes) moves into the capillary.
Regulating Blood Flow in Veins
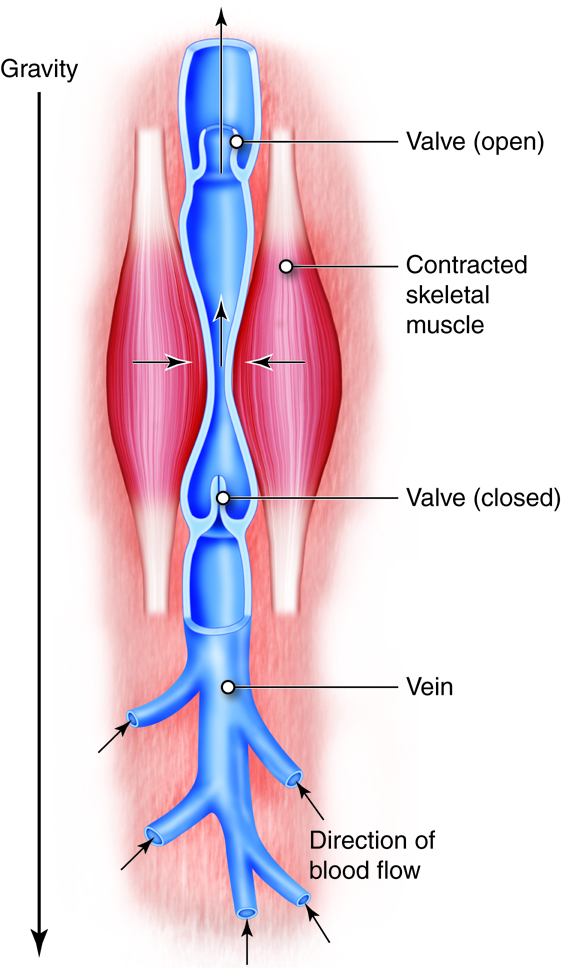 Pressure in veins is so low, however, that we need special features to keep blood moving back to the heart.
Pressure in veins is so low, however, that we need special features to keep blood moving back to the heart.
If anyone reading this has done plumbing work, you know that often, you must install a valve called a backflow preventer. One-way valves act as backflow preventers in the venous system. As people age, this system breaks down and venous blood can pool in parts of the body, especially the lower extremity. The resulting increase in pressure increases the size of the veins; they become varicose. They can also leak blood into the surrounding tissue, which causes discoloration and itching.
Also, the contraction of muscle around the veins helps pump blood back to the heart. This is why paralyzed patients must sometimes have their extremities moved manually. Loose blood clots, or emboli, are a leading cause of death in paraplegics. In the section on veins (Objective 7), we will see why clots from the lower extremities often lodge in the lungs (pulmonary emboli).
Histology of the Veins
Venules have very little smooth muscle; unlike arteries, they are essentially pipes that cannot change diameter in response to changing conditions.
As we return blood to the heart via the venous part of the systemic circulation, veins become larger and larger and develop a thin layer of smooth muscle, but it is never as prominent as it is in arteries.
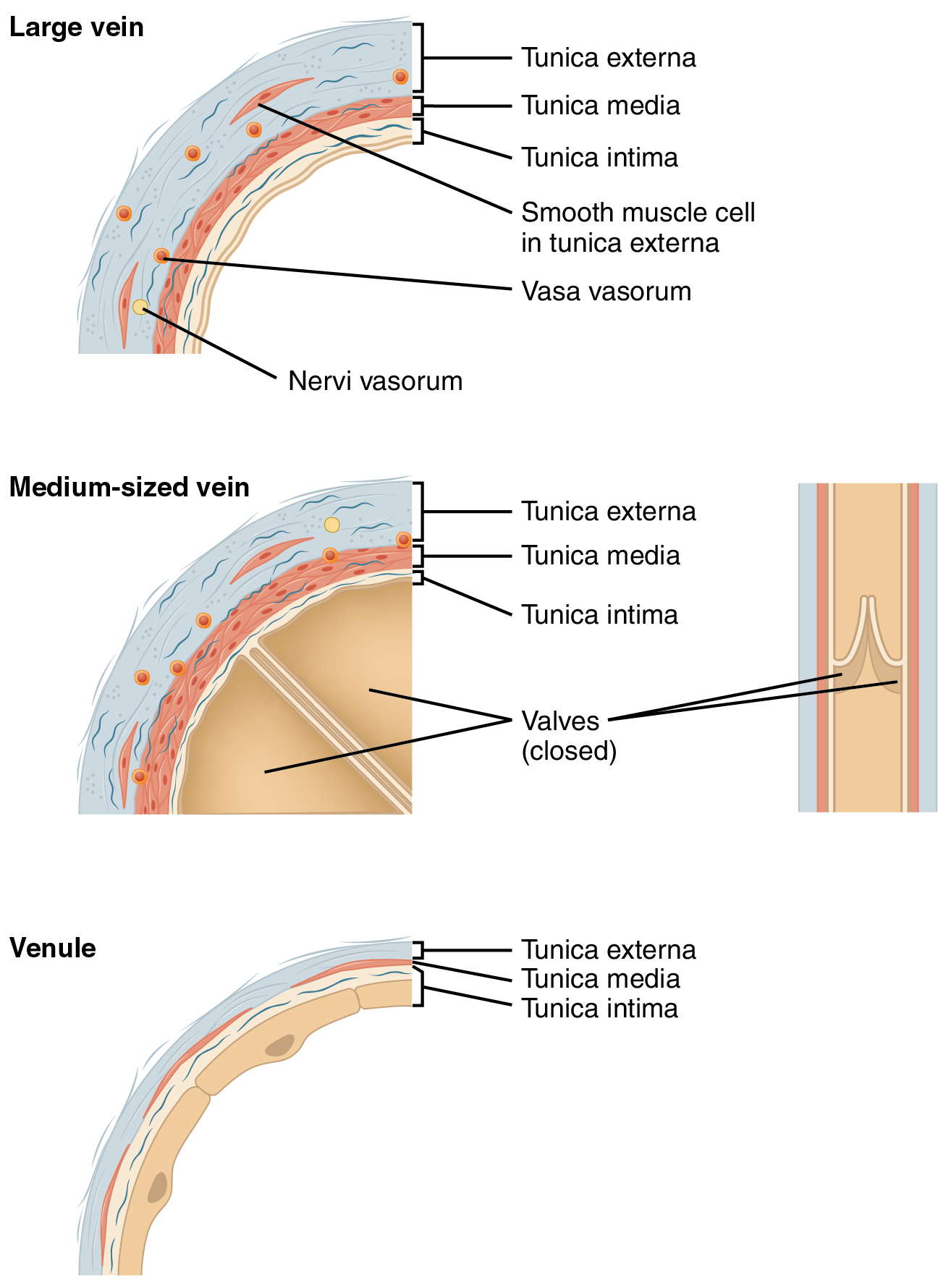
The tunica externa (connective tissue layer) is very thick. Veins are primarily structural elements that do not respond much to changing conditions.
Similarly, because veins prioritize channeling blood over managing it, the tunica interna (endothelial cell layer) is quite thick and difficult for chemicals and cells to penetrate.
High Blood Pressure (Hypertension) Due to Atherosclerosis
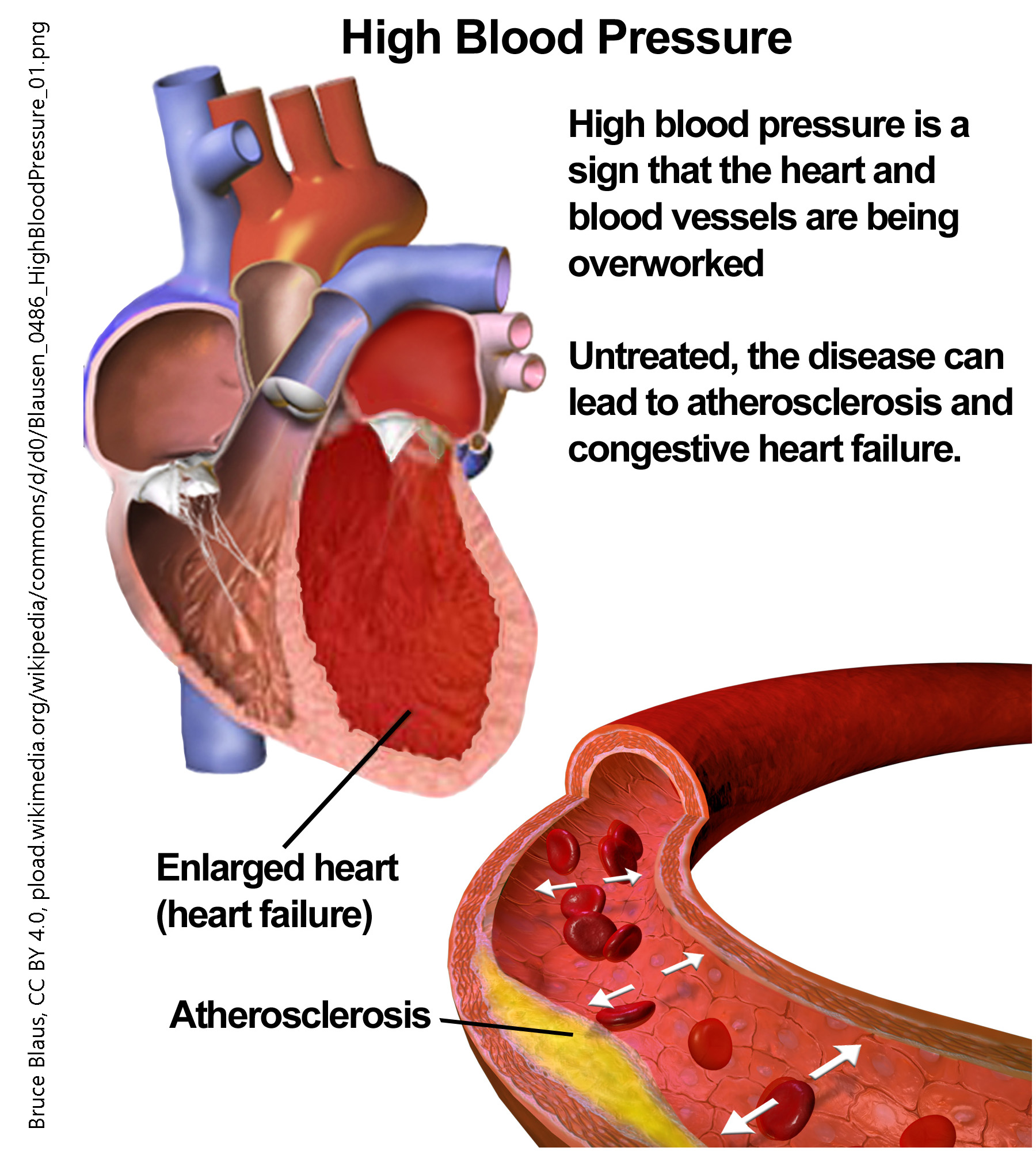 In plumbing and other applications where we control the flow of fluid, Poiseuille’s Law says that the flow rate varies as the fourth power of diameter (i.e., diameter x diameter x diameter x diameter). That means small changes in diameter, such as when an atherosclerotic plaque begins to form, can have a huge impact on how much blood flows through the artery. As we saw in the section on Starling’s Law, increasing the diameter of a capillary (or blood vessel) can also decrease pressure (again, proportional to the fourth power of the diameter) while decreasing the diameter of a blood vessel can increase pressure. (A fire hose, pressure washer, or sink sprayer works on this principle: as the water is forced through a narrow opening, the pressure increases.)
In plumbing and other applications where we control the flow of fluid, Poiseuille’s Law says that the flow rate varies as the fourth power of diameter (i.e., diameter x diameter x diameter x diameter). That means small changes in diameter, such as when an atherosclerotic plaque begins to form, can have a huge impact on how much blood flows through the artery. As we saw in the section on Starling’s Law, increasing the diameter of a capillary (or blood vessel) can also decrease pressure (again, proportional to the fourth power of the diameter) while decreasing the diameter of a blood vessel can increase pressure. (A fire hose, pressure washer, or sink sprayer works on this principle: as the water is forced through a narrow opening, the pressure increases.)
That means that atherosclerotic plaques both decrease blood flow and increase pressure. Because of Poiseuille’s Law, small changes in the diameter of a blood vessel result in large changes in blood flow and blood pressure.
Media Attributions
- U16-031 Structure of Blood Vessels © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U16-032 Arterial Blood Vessels © BioRender is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U16-034 Capillary Network © Open Learning Initiative Anatomy & Physiology is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- U16-035 Types of Capillaries © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U16-036 Relationships among Vessels in the Systemic Circuit © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U16-036c Small Blood Pressure for Starling © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter adapted by Jim Hutchins is licensed under a CC BY (Attribution) license
- U16-037 Capillary Exchange © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U16-038 Structure of a Vein and Valves © Open Learning Initiative Anatomy & Physiology is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- U16-039 Comparison of Veins and Venules © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U16-040 High Blood Pressure © BruceBlaus is licensed under a CC BY (Attribution) license

