Liver and Gallbladder
Objective 7
Describe or identify on a diagram the gross anatomy of the liver: liver lobes, coronary ligament, falciform ligament, round ligament (ligamentum teres). Identify on a diagram and be able to describe the liver’s blood supply: hepatic artery, hepatic portal vein, hepatic vein. Identify on a diagram and be able to describe the function of the cells and structures in a liver lobule: hepatocytes, Kupffer cells, hepatic sinusoids, bile canaliculi, central vein, portal triad (hepatic triad). Describe or identify on a diagram the structures associated with bile production, storage and release: hepatic duct, cystic duct, gallbladder, common bile duct, sphincter of the ampulla. Explain how each structure is involved in the production, storage and release of bile. Diagram the enterohepatic circulation of bile salts.
The liver is tied with the brain for the title “second-largest organ of the body”. Do you recall which organ is larger?
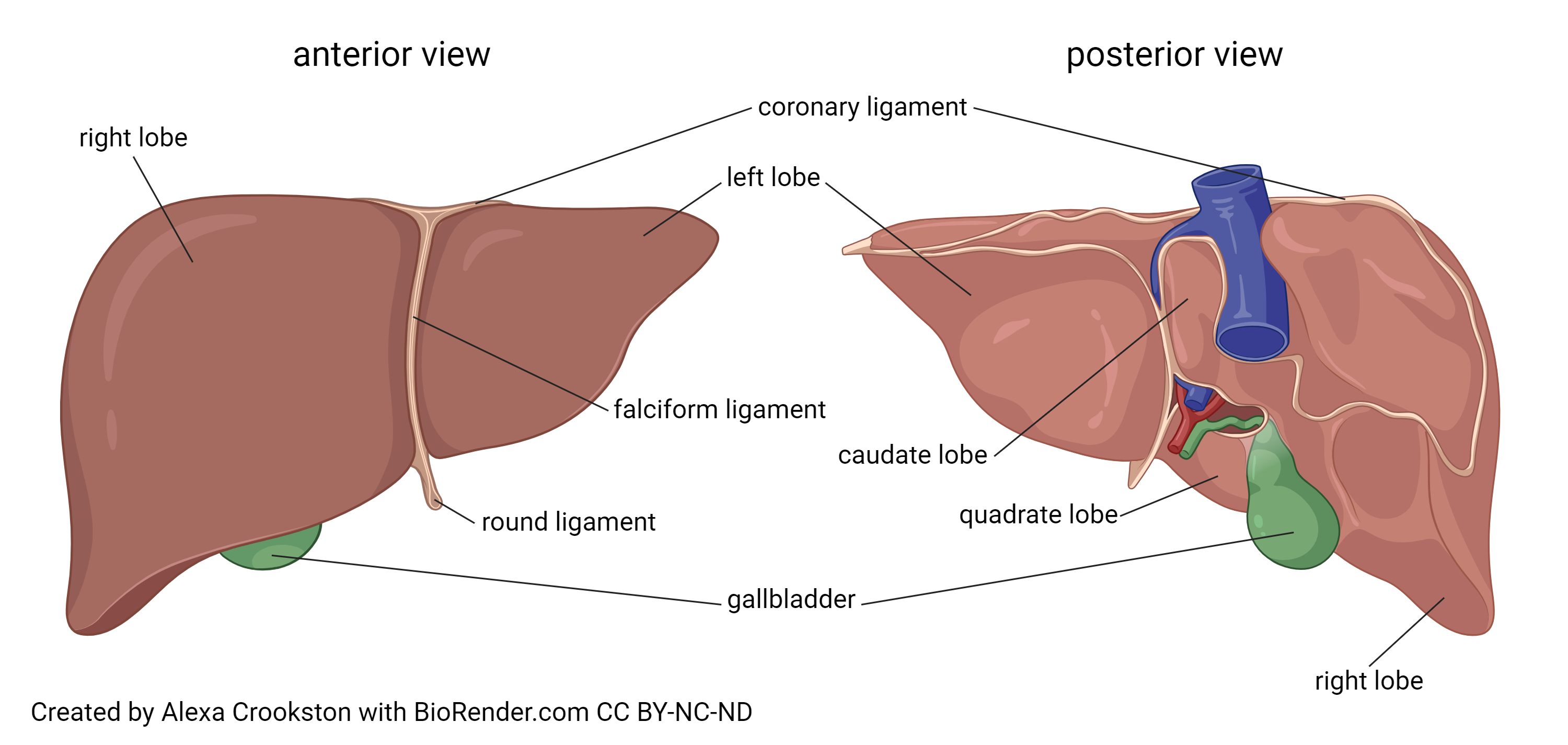
Grossly, the liver is divided into four lobes. The right and left lobes are visible from the anterior (ventral) surface of the body. The caudate (Latin: “tail-shaped”) and quadrate (Latin: “square”) lobes are only seen when looking from the posterior or inferior surfaces.
The liver is held in place by three strips of connective tissue (ligaments). The falciform ligament (Latin: “sickle-shaped”), the coronary ligament, and the round ligament (also called by its Latin name, ligamentum teres). The falciform ligament and coronary ligament both attach to the diaphragm, which keeps the liver in a position in the superior part of the abdominal cavity and mostly to the right side of the body.
The liver has a close relationship to its neighbors in the abdominal cavity: the pancreas, and the duodenum. These three organs work together, as we’ll see.
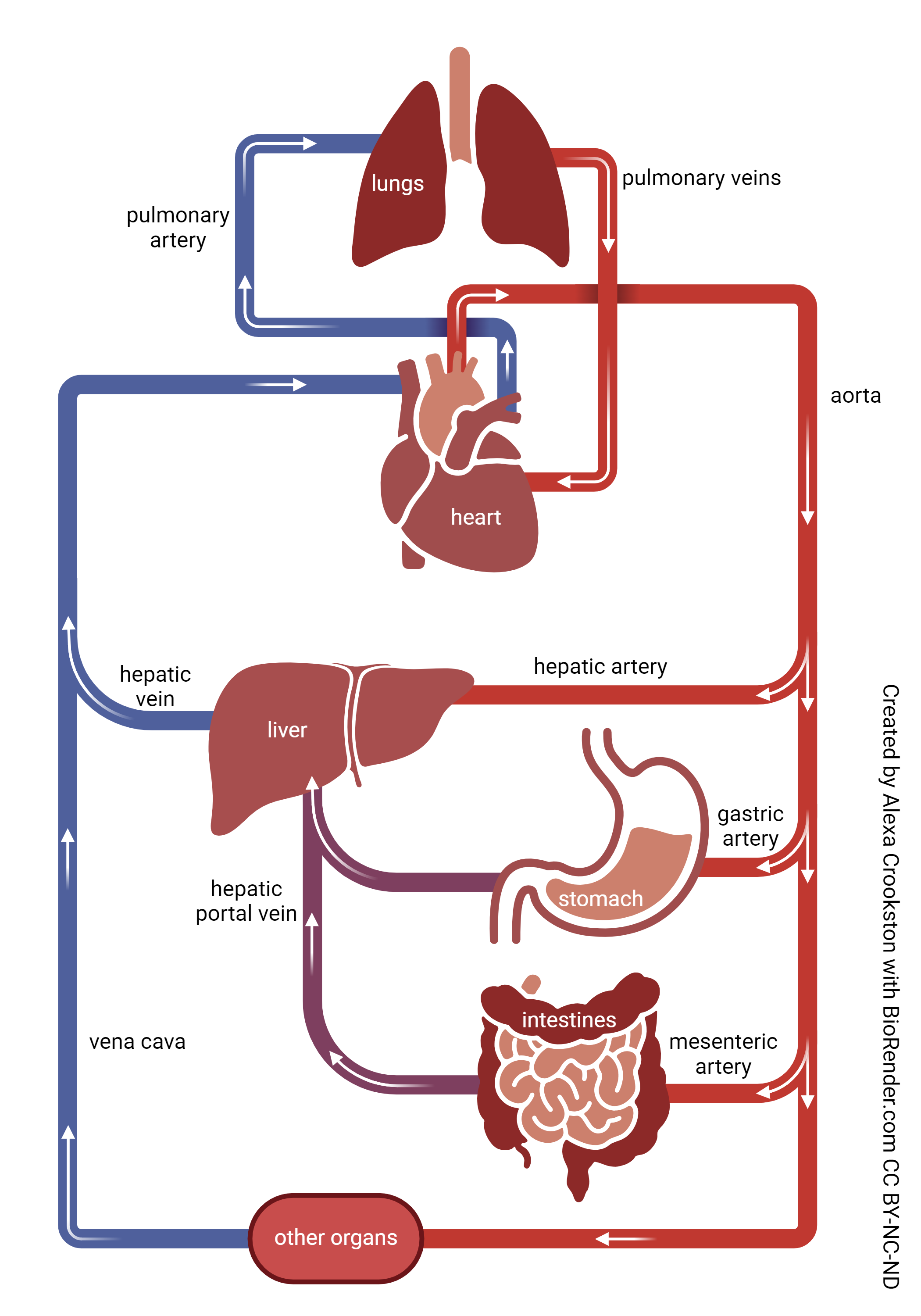
The liver’s blood supply is different than most other organs. The cells of the liver, like any other cells of the body, need oxygen and glucose, and they get oxygenated blood from the left ventricle of the heart, via the aorta, and abdominal aorta, to the hepatic artery (also called proper hepatic artery).
A second source of blood to the liver is related to its function as a detoxification and energy storage organ. This supply comes from the venous drainage of the stomach and intestines, through a vessel called the hepatic portal vein. This brings glucose-rich but oxygen-poor blood from the absorptive cells of the digestive organs to the liver for processing.
The venous drainage of the liver is through hepatic veins to the inferior vena cava and thence to the right atrium of the heart.
Blood Flow Through Liver
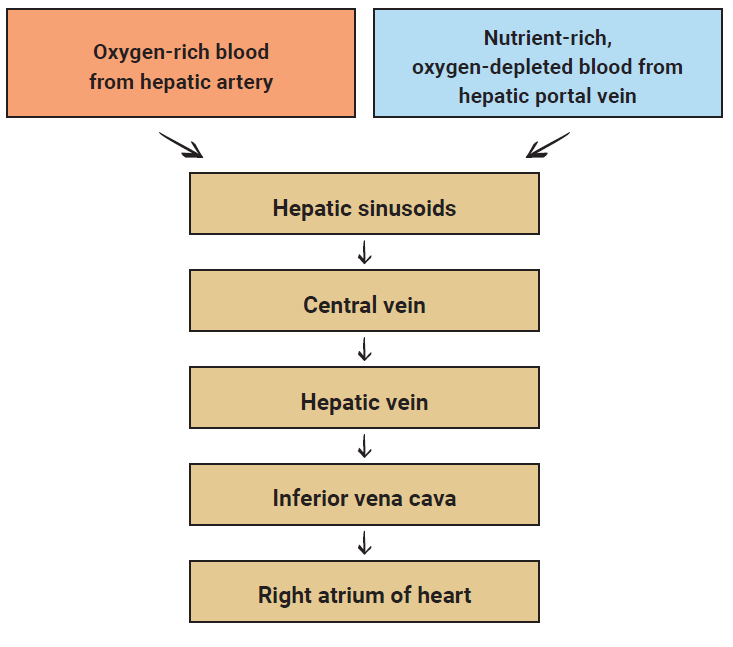
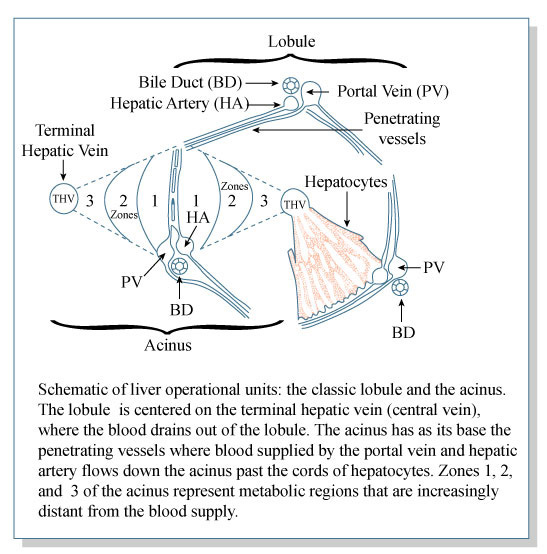
In order to carry out its functions of blood cleansing and nutrient metabolism, the liver routes blood through functional units called liver lobules. Blood from the hepatic artery and hepatic portal vein is passed alongside the cells of the liver, and then collects in small central veins which gather from the entire liver to form the hepatic vein.
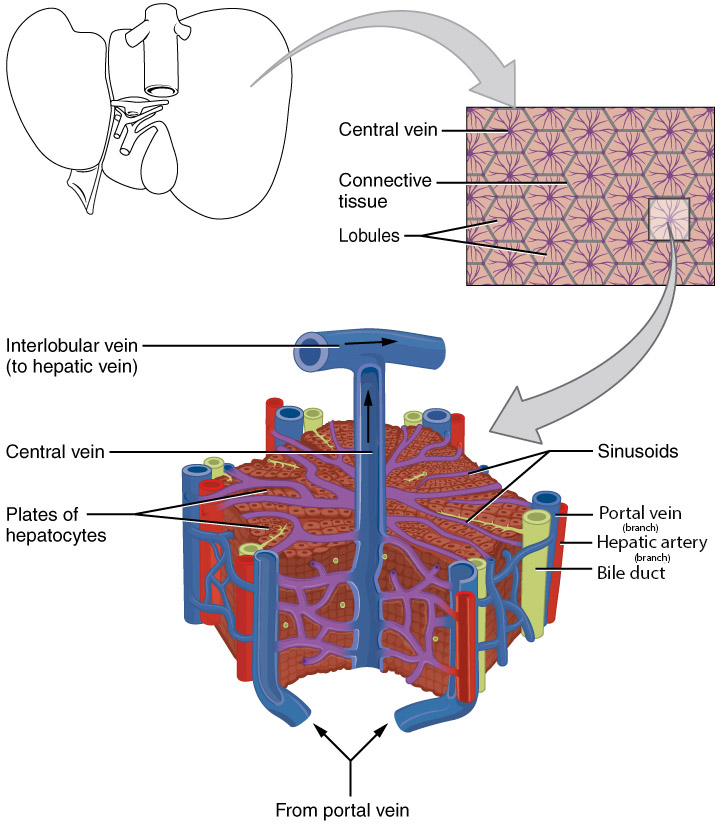
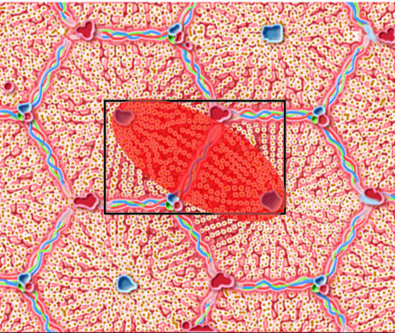 For years, physiologists have assumed that the hexagonal (six-sided) hepatic lobule is the functional unit of the liver. That’s certainly how we’ve presented it. This was based on animal studies, mostly using pigs. Now, the thinking is that in the human liver, the real functional unit is a hepatic acinus, two 1/6 slices of the lobule working together, as shown.
For years, physiologists have assumed that the hexagonal (six-sided) hepatic lobule is the functional unit of the liver. That’s certainly how we’ve presented it. This was based on animal studies, mostly using pigs. Now, the thinking is that in the human liver, the real functional unit is a hepatic acinus, two 1/6 slices of the lobule working together, as shown.
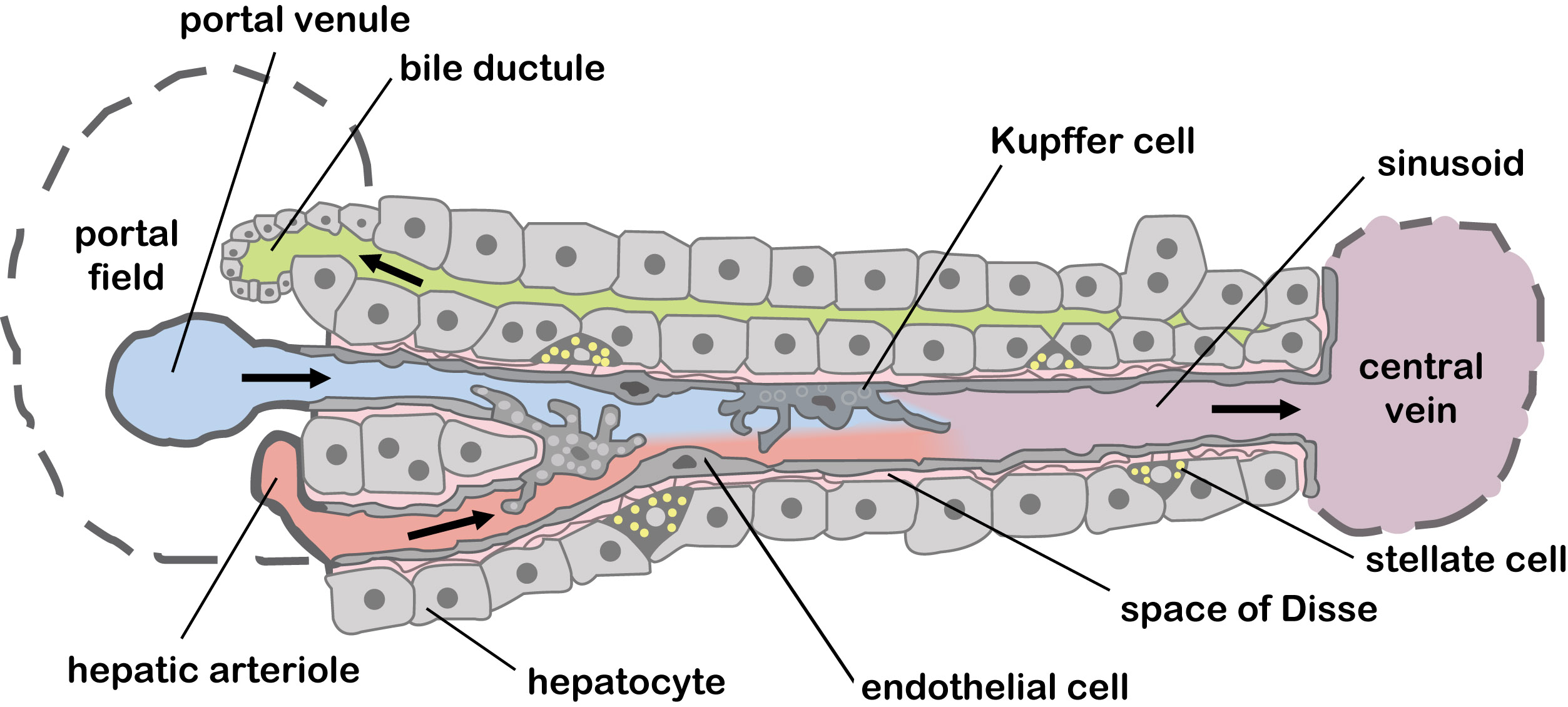
There are two main cell types in the liver.
- Hepatocytes inactivate toxins, produce bile, and also produce a variety of blood proteins. They also play a role in the metabolism of carbohydrates, lipids, and proteins.
- Kupffer cells are just a special name for a type of macrophage found in the liver. They destroy aged red blood cells and any invaders that reach the liver from the intestinal drainage.
The skin, liver and kidneys work together to activate vitamin D from its precursor forms.
One of the jobs of hepatocytes is to produce bile, a greenish liquid substance that is stored in the gallbladder. When bile is released into the GI tract, it helps to emulsify fats so they can be transported across the intestinal cell and dumped into the lymph vessel (lacteal) in the center of each villus.
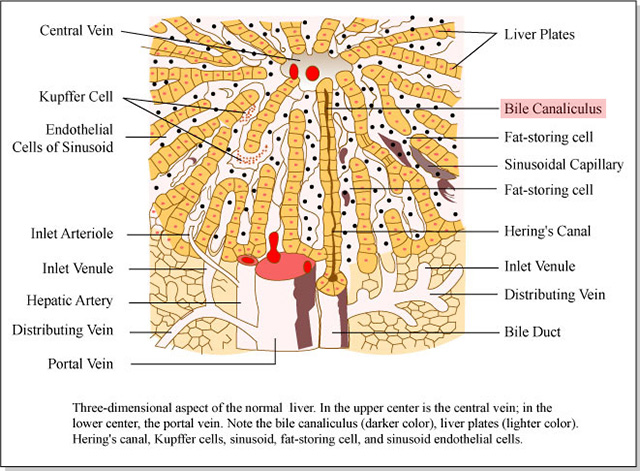 Bile is produced and secreted by hepatocytes, and it travels in tiny vessels called bile canaliculi to join together as a bile duct.
Bile is produced and secreted by hepatocytes, and it travels in tiny vessels called bile canaliculi to join together as a bile duct.
Bile is on the production side of the liver. On the supply side, remember that two blood vessels supply blood to the liver: the hepatic artery, carrying oxygenated blood, and the hepatic portal vein, carrying deoxygenated blood from the GI tract. The branches of bile ducts, hepatic artery, and hepatic portal vein generally run together as three vessels, a hepatic triad.
We have described the production of bile at the cellular (hepatocyte) level. Now let’s see how bile is stored and released.
Bile secreted by individual hepatocytes flows into bile canaliculi, then into the larger bile duct. Remember that the bile duct is part of the portal triad. From there, the bile ducts in the right lobe flow into the right hepatic duct; bile ducts in the left lobe flow into the left hepatic duct. These, in turn, feed into the common hepatic duct. A branch of the common hepatic duct, the cystic duct, leads to the gallbladder. The gallbladder is a hollow bag which stores and concentrates bile.
Bile Storage & Release
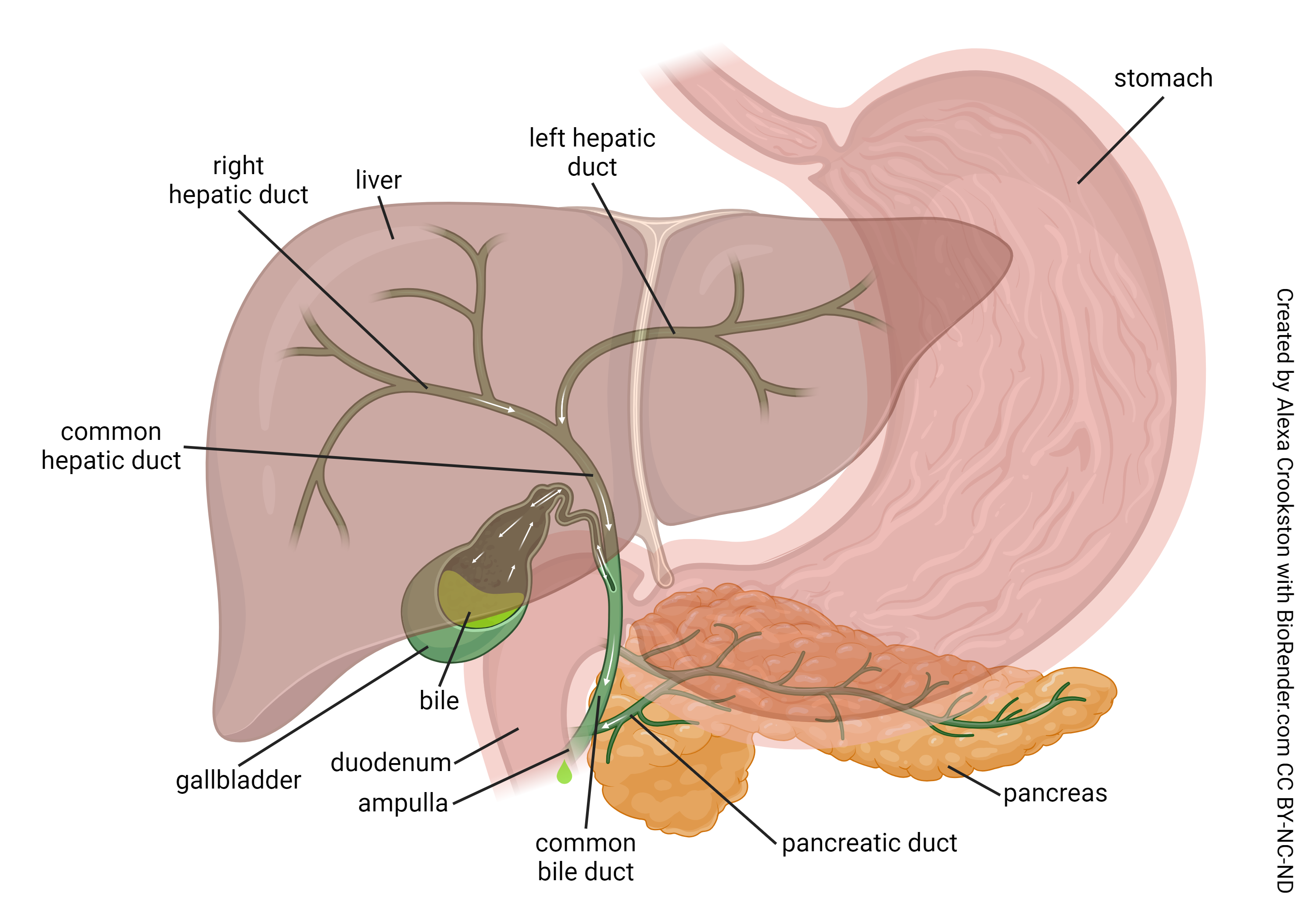
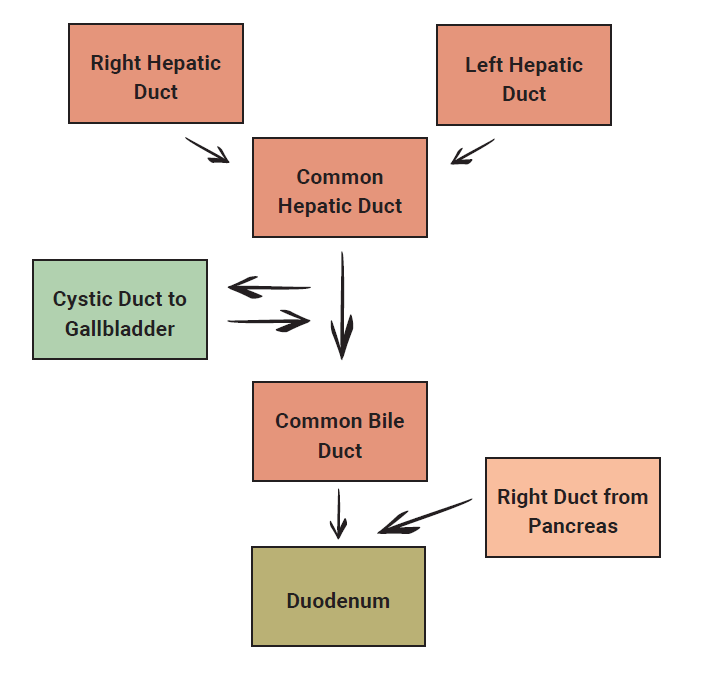
When the GI tract signals the presence of fats in a meal, the smooth muscle (autonomic) of the gallbladder swings into action, squeezing the gallbladder and releasing stored bile. This bile flows out the cystic duct (again) and then into the common bile duct to join pancreatic juices (more later). The mixture is released into the duodenum at the sphincter of the hepatopancreatic ampulla. (The “old” name for this, the sphincter of Oddi — “ah-dee” — is easier to remember, and more fun to say). The ampulla (Latin: “bottle”) is a mixing chamber for pancreatic juices and bile; the sphincter controls release of this mixture into the duodenum.
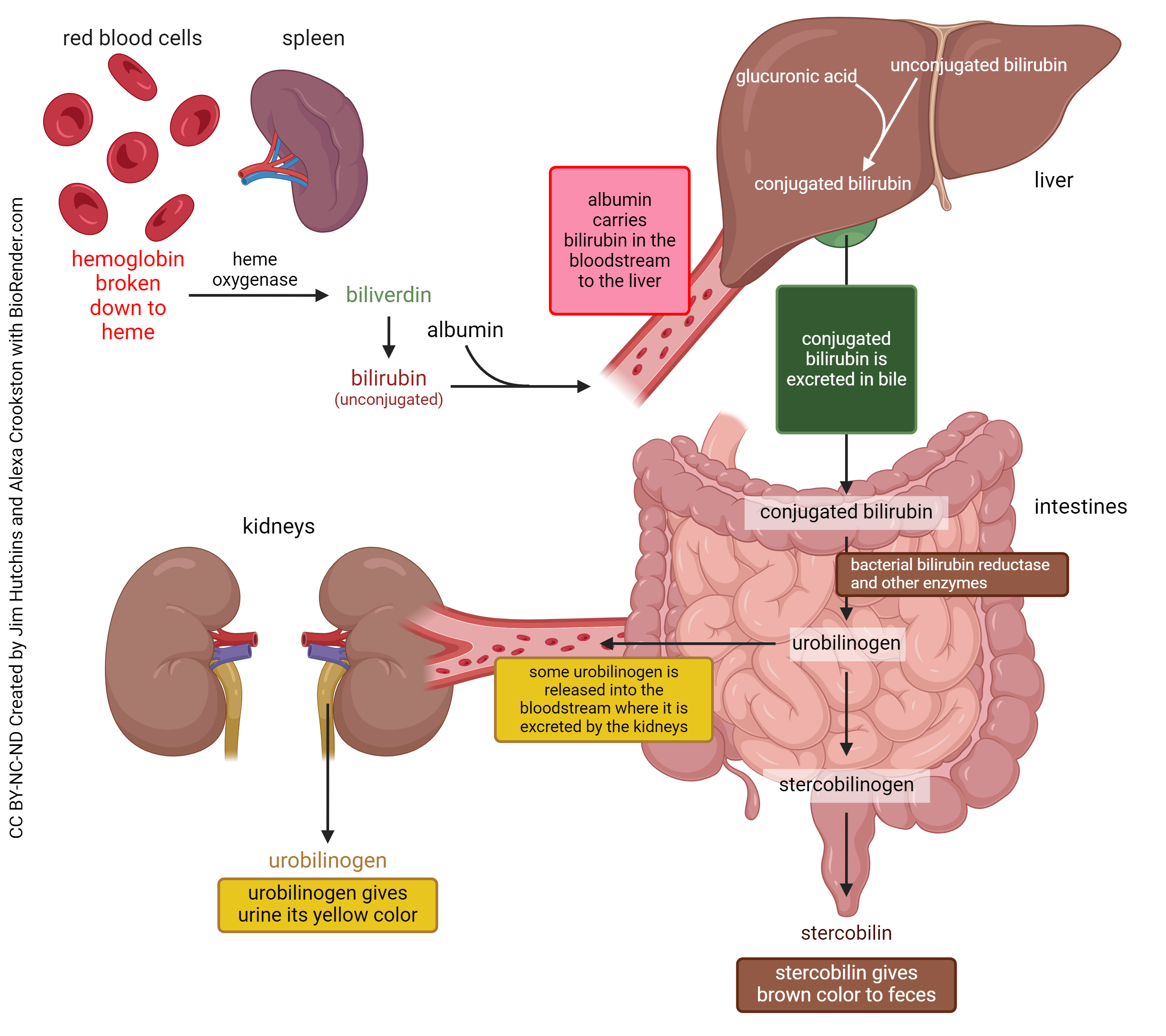
Now, a few specifics about the enterohepatic circulation of bile salts. Recall, the iron-containing molecule heme is found as an oxygen carrier in hemoglobin, myoglobin, and cytochromes. About 85% of the body’s heme is found in red blood cell hemoglobin. There are a lot of red blood cells, and they have an average lifetime of about 120 days, therefore, heme is constantly being broken down. The spleen (and other cells, if needed) use the enzyme heme oxygenase to convert heme to biliverdin. Biliverdin spontaneously converts to bilirubin. Bilirubin made this way is referred to as “unconjugated” and gloms onto the blood protein albumin and is carried to the liver.
Unconjugated bilirubin is insoluble in blood. In the liver, it is conjugated to the small molecule glucuronic acid, making it water-soluble. In this form, it makes up a major portion of bile.
Conjugated bilirubin is sent to the intestines where intestinal bacteria remove the glucuronic acid and convert it to urobilinogen. Some of this urobilinogen is reabsorbed back into the circulation. The rest is further broken down by bacteria into stercobilinogen and then stercobilin, which gives feces their characteristic brown color.
Clinical Connection
Problems arise when this process goes awry.
One way in which this can happen is if bile is obstructed, and is no longer released in normal quantities through the hepatopancreatic sphincter. In this case, little or no conjugated bilirubin is converted stercobilin, so the feces would be pale in color.
At the same time, the conjugated bilirubin backs up in the liver and eventually leaks out into the circulation. Bilirubin can then end up in the tissues of the body leaving the patient with a yellowish pigment in their skin and even the whites of their eyes. This symptom is called jaundice (from the French jaune, yellow). The kidneys work to clear this unwanted bilirubin which leaves the urine with a dark brown color.
The liver of newborn babies is often slow to become fully functional. Other conditions such as drug and alcohol abuse, viral infections (such as hepatitis) and even trauma can damage the liver, leaving it less able to perform its many functions. In any of these cases, bilirubin can leak from the liver and into the circulation, resulting in jaundice.
Media Attributions
- U18-043 Liver © Crookston, Alexa is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U18-044 Simple Circulatory System © Crookston, Alexa is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U18-045 Blood Flow through the Liver © Burr, Justin is licensed under a CC BY-SA (Attribution ShareAlike) license
- U18-046 Liver Microscopic © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U18-047a Cenveo Liver Acinus © Cenveo is licensed under a CC BY (Attribution) license
- U18-047b Mechanisms of Drug Actions © MIT OpenCourseWare is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- U18-048 Cells of Liver © Frevert U, Engelmann S, Zougbédé S, Stange J, Ng B, et al. is licensed under a CC BY (Attribution) license
- U18-047c Mechanisms of Drug Action © MIT OpenCourseWare adapted by Jim Hutchins is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- U18-050 Gallbladder and Extrahepatic Bile Ducts © Crookston, Alexa is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U18-051a Bile Storage and Release © Burr, Justin is licensed under a CC BY-SA (Attribution ShareAlike) license
- U18-051b Bile Processing © Hutchins, Jim and Crookston, Alexa is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license

