Immune System Basics
Objective 8
Define the terms epitope and antigen and describe how the immune system reacts to antigens. Define innate immunity and adaptive immunity. Explain the difference between active and passive immunity, and natural and artificial immunity.
Epitope, Antigen, and Antibody
We have already used the term antigen, but we will now take a closer look at what antigens are and how they interact with the immune system. An antigen can be defined simply as a substance that is recognized as foreign. Foreign substances can react with products of the immune system.
There are four main characteristics that determine the antigenicity of a substance.
- it must be recognized as foreign
- it must have structural complexity
- it must be large enough (greater than 10,000 Da, or about 100 amino acids)
- it must be organic (that is, a carbon-containing compound)
Recognition as foreign is the most important of these four. A potential antigen could fit all of the other criteria but if the body does not see it as foreign, it will leave it alone. We’ll discuss how the body recognizes “foreign” vs “familiar” in Objective 12. For now, it’s important to note that “familiar” depends on context. If a substance is removed from its normal location in the cell, it can go from being familiar to foreign. An example of this is in autoimmune diseases. For example, in multiple sclerosis, a normal protein in myelin is released into the surrounding extracellular fluid and since it’s not surrounded by lipid, the body recognizes it as foreign even though in context it was once familiar.
A hapten is an antigen which does not meet the criterion of size. That is, it is too small to cause an antibody response by itself. Haptens combine with familiar components of the body to create a novel, foreign antigen. For example, in some people nickel ions (Ni2+) can combine with keratin, the main protein of skin, to form a novel antigen which is recognized as foreign. This is the basis for an allergic reaction to nickel in cheap jewelry.
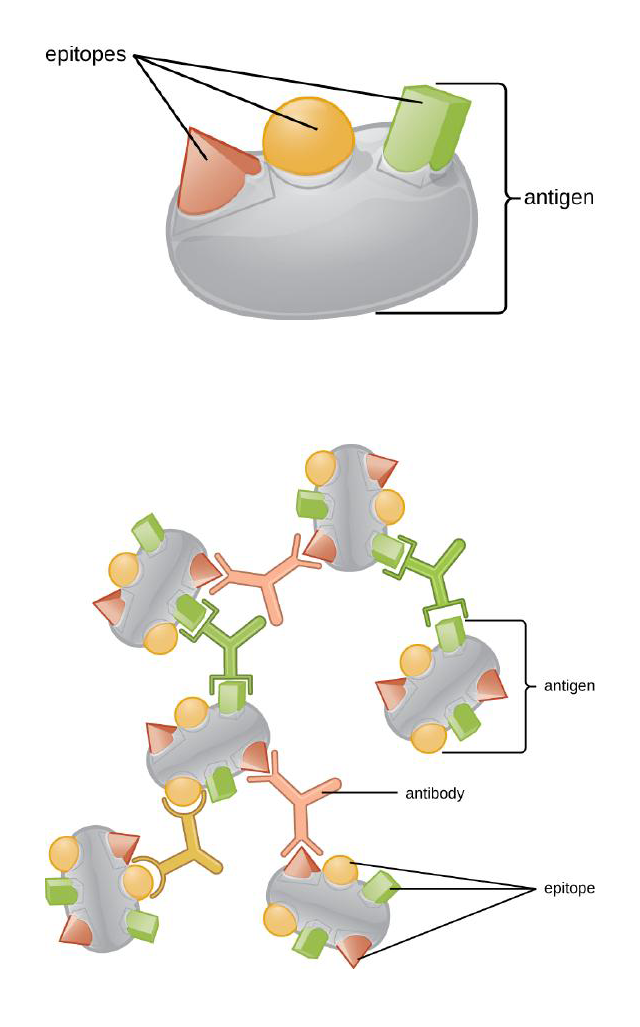
On the other end of the size scale, a large antigen may have several places where it can react with the immune system. The Greek word for “place” is topos and “epi-“ is a prefix meaning “on top of” so these individual places on a big molecule, each of which can trigger its own immune response, are called antigenic determinants or epitopes.
Not all antigens are dangerous. Most of what the body is exposed to in an average day is harmless and largely ignored by the immune system. All cells of the body contain markers and other surface proteins that could make them antigenic, but the body is able to recognize its own cells. This process is called self-recognition. When the immune system recognizes self-antigens and then leaves them alone we use the term self-tolerance. We will see how tolerance develops in Objective 12.
An important part of white blood cell development, especially with lymphocytes, is antigen recognition. Entire groups of immune cells, called clones, are produced from parent white blood cells. As these cells develop and mature they are exposed to self-antigens. If they react to these antigens they are selected out of the population (negative selection) and undergo apoptosis. This step in development is referred to as clonal deletion and leaves the immune system with only those cells that will not react to harmless cells in the body. Abnormalities in self-recognition, self-tolerance or clonal deletion can lead to autoimmune disorders.
The way the body protects itself from potentially harmful antigens is similar to how we seek to protect our homes from potential intruders. The goal is to feel safe at home. Likewise, the body wants to remain safe from potential pathogens that could cause disease. We refer to this as immunity. When the immune system is prepared and functioning in a way that would allow it to keep out invaders or respond appropriately if those invaders get in, we say the individual is immunocompetent. When barriers and immune responses are not sufficient to protect against pathogens we say the person is immunocompromised or immunodeficient.
Innate Immunity
Physical barriers and non-specific responses to potential pathogens comprise one division of the immune system known as the innate immune system or innate immunity (inborn immunity). This would be like the walls of your home, the locks on your doors, and even a guard dog. Regardless of what is trying to break into your home, these features would react the same. A raccoon getting through a window or a masked human intruder are probably going to get the same reaction from your dog: growling, barking, and maybe even biting.
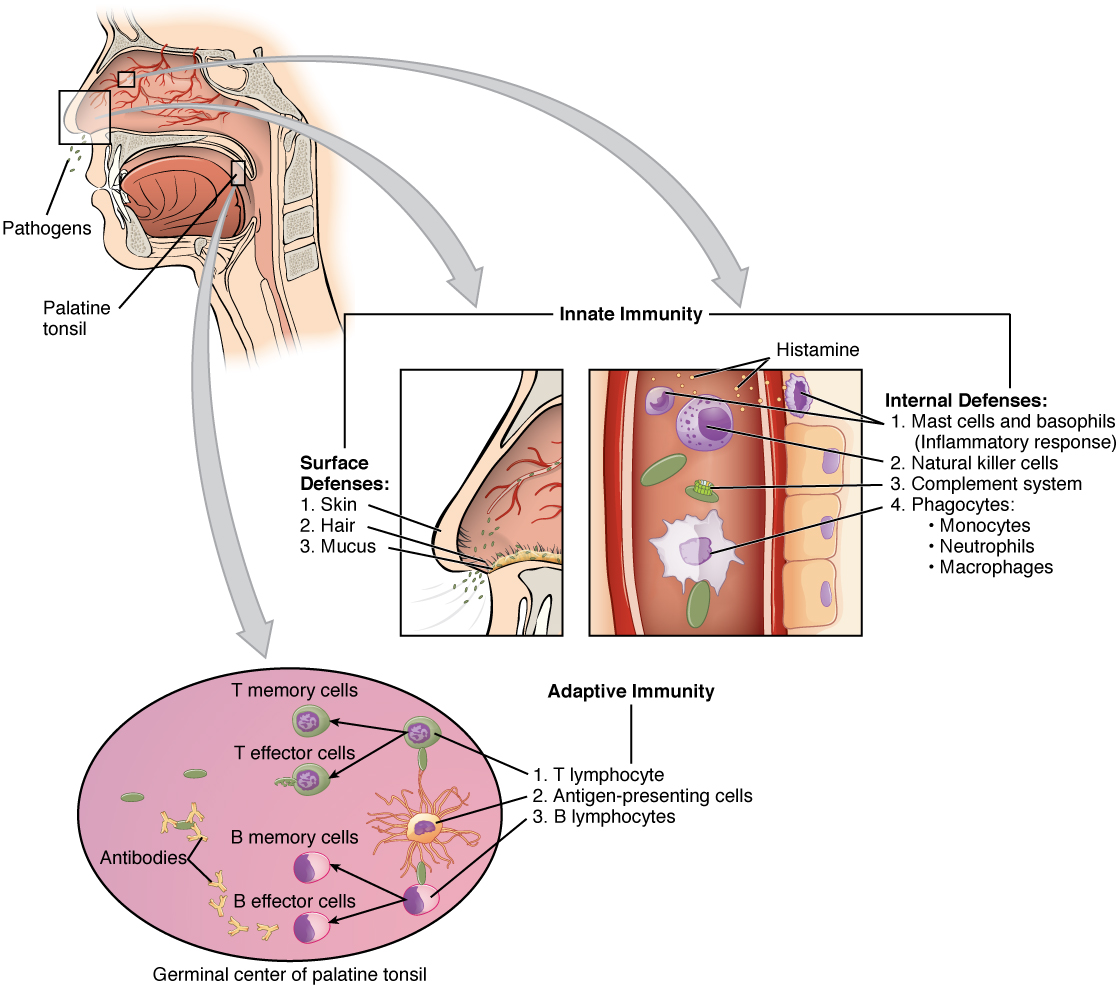
In the body, innate immunity consists of a number of different cellular and chemical barriers which non-specifically protect the body and respond to pathogenic organisms. In addition to being non-specific, innate immunity is non-adaptive, meaning that the response doesn’t change from exposure to exposure. Components of innate immunity are intact at birth and include the skin and mucous membranes, cilia, antimicrobial chemicals, phagocytes, inflammation, and fever.
Adaptive Immunity
The other division of the immune system is the adaptive immune system, also known as adaptive immunity or acquired immunity. As the name implies, this system is able to change over time, or adapt to different situations. This could be compared to an unpleasant experience with intrusive neighbors, pushy door to door salespeople, or perhaps your in-laws. After a bad experience or two, you decide to install a doorbell camera so you can see who is attempting to come in. The next time the offending party arrives at your house, you recognize them, remember the last experience, and react quickly to prevent another ruined afternoon.
Components of adaptive immunity include: T lymphocytes, B lymphocytes, plasma cells, and antibodies. (See Objective 9 for a more complete description of each of these.) The ability to recognize and uniquely respond to specific invaders is the main function of adaptive immunity. As a person is exposed to more and more antigens, their adaptive immune system creates a bank of cells and antibodies that remember and can respond quickly to those specific antigens if they return. Having these components in place is a major contributor to immunity.
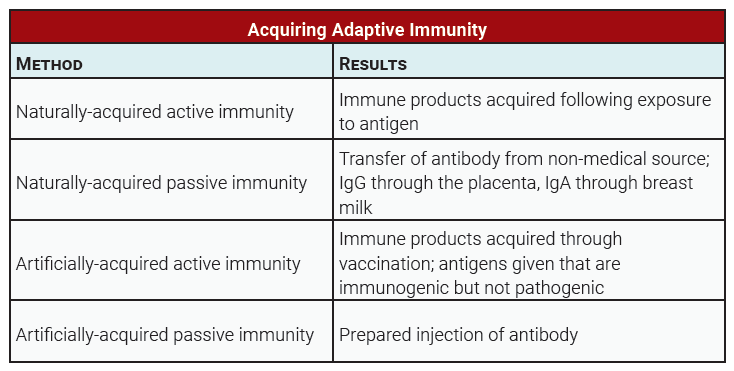
Adaptive immunity can be acquired in a number of different ways: actively or passively, and naturally or artificially. Active acquisition of immunity means that someone’s immune system was stimulated, and they generated a cellular and antibody-mediated response as well as memory. Active immunity provides long-term immunity. Passive immunity simply means the products of immunity were given to them. Passive is a short-lived response; the acquired cells die or the antibodies are eventually lost.
Active vs Passive Immunity

Active immunity is like baking a pie. An individual pulls out the recipe book, makes the crust and filling, and bakes the pie. Passive immunity is simply buying a pie. The end result is the same, there is a pie, but with active immunity, memory is gained, and immune products can be made over and over again.
Natural vs Artificial Immunity

Acquiring adaptive immunity, whether actively or passively, can be a natural process or artificial. Simply getting sick from another person or the passing of antibodies through breast milk from mom to baby are examples of natural immunity. Once someone in a lab coat somewhere gets involved, the process becomes artificial. Injecting a person with antibodies taken from donors or giving a person a vaccine can confer immunity, but these are examples of artificial immunity. Note that even though a vaccine is an artificial introduction of antigen to a person’s immune system, the process of responding and building up the components of the adaptive immune system is an active process, not passive.
Media Attributions
- U15-039 Epitopes and Antibody Cross-linking © Allen, Summer; Auman, Ann; Brelles-Marino, Graciela; Feldman, Myriam Alhadeff; Flowers, Paul; Pinchuk, George; Rowley, Ben; Sutherland, Mark; Franklund, Clifton and Paterson, Ann adapted by Jim Hutchins is licensed under a CC BY (Attribution) license
- U15-040 Innate and Adaptive Responses © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U15-041 Breastfeeding a Baby © Nosik, Anton is licensed under a CC BY (Attribution) license
- U15-042 Polio Vaccination USAID © Helmer, Kendra / USAID is licensed under a CC BY-NC (Attribution NonCommercial) license
- U15-043 Acquiring Adaptive Immunity Table © Hutchins, Jim is licensed under a CC BY-SA (Attribution ShareAlike) license

