Homologous Structures in the Male and Female
Objective 4
Compare and contrast homologous structures of the male and female reproductive systems.
Normal human gestation (time from conception to birth) is 40 weeks. At 5-6 weeks, embryos have an indifferent gender; that is, male and female embryos appear exactly the same. After that, a small region (gene) on the Y chromosome becomes active. The name of the gene is the sex-determining region Y (SRY).
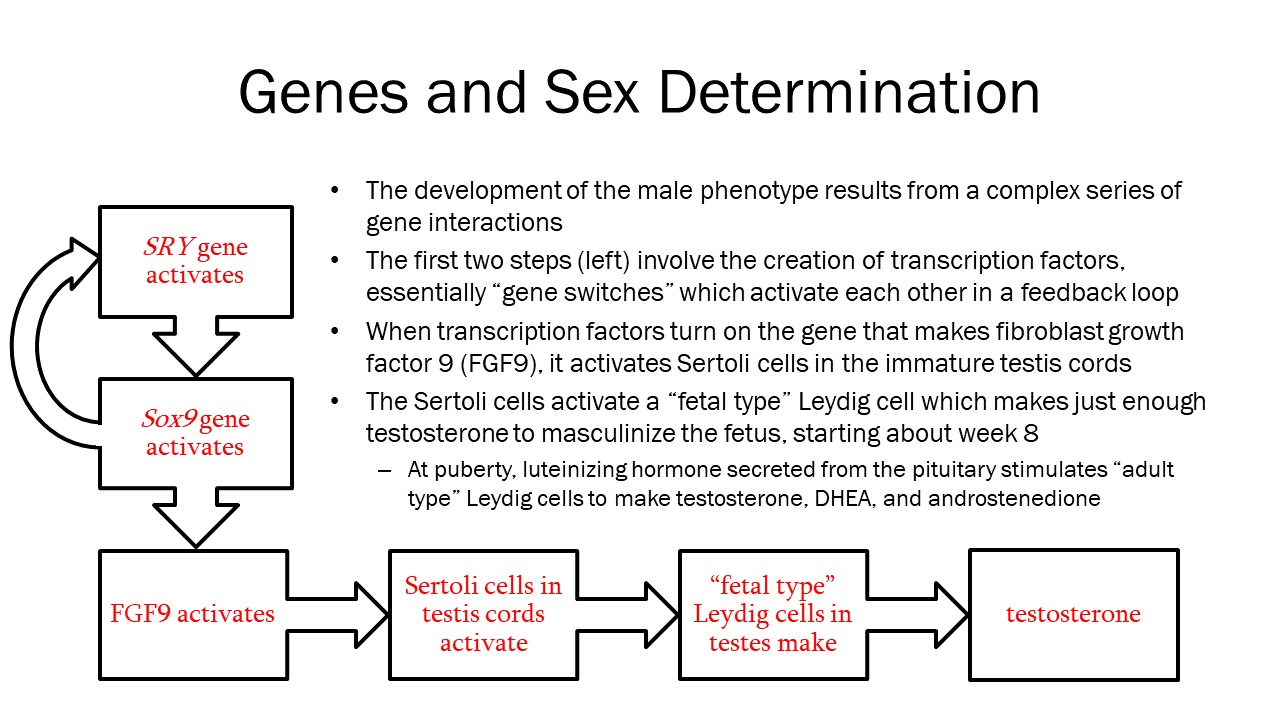
Remember, the chromosomal designation for female is XX and male is XY. Male embryos have a Y chromosome and, on that Y chromosome, the SRY gene. Female embryos don’t have a Y chromosome and, therefore, don’t have an SRY gene. If the SRY gene is present and active (not mutated), the embryo will develop male reproductive anatomy. If the SRY gene is not present or is inactive, the embryo will develop female reproductive anatomy. The same embryonic structures develop into one thing if SRY is present, something else if it’s not.
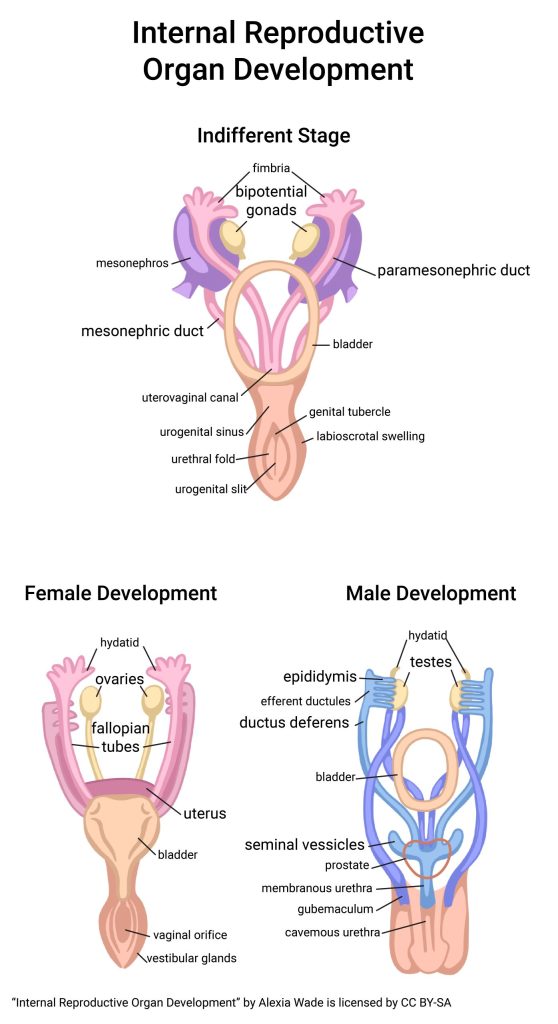
The image above shows the development of internal reproductive structures. In the early (5-7 week) embryo, a pair of bipotential gonads and two pairs of ducts have formed – the mesonephric ducts and the paramesonephric ducts. Under the influence of SRY gene products, the bipotential gonads will differentiate into testes, the mesonephric ducts will become seminal vesicles, ducti deferens, and epididymes, and the paramesonephric ducts will deteriorate. If the SRY gene is not present or is defective (no SRY gene products), the bipotential gonads will differentiate into ovaries, the mesonephric ducts will degenerate, and the paramesonephric ducts will become uterine tubes, uterus, cervix, and vagina.
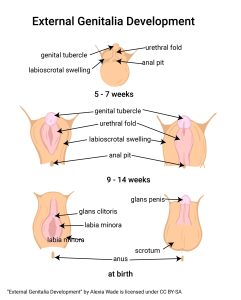
This image shows the development of external reproductive structures, which occurs concurrently with the internal structures. Externally, the early (5-7 week) embryo’s gender cannot be determined. In both genders, a genital tubercle, urethral fold, and labioscrotal swellings are visible. As with the internal structures, under the influence of SRY gene products, the genital tubercle differentiates into the glans penis, the urethral fold becomes the spongy urethra, and the labioscrotal swellings develop into the corpus spongiosum and scrotum. With no SRY gene products, the genital tubercle differentiates into the glans clitoris, the urethral fold becomes the labia minora, and the labioscrotal swellings develop into the labia majora.
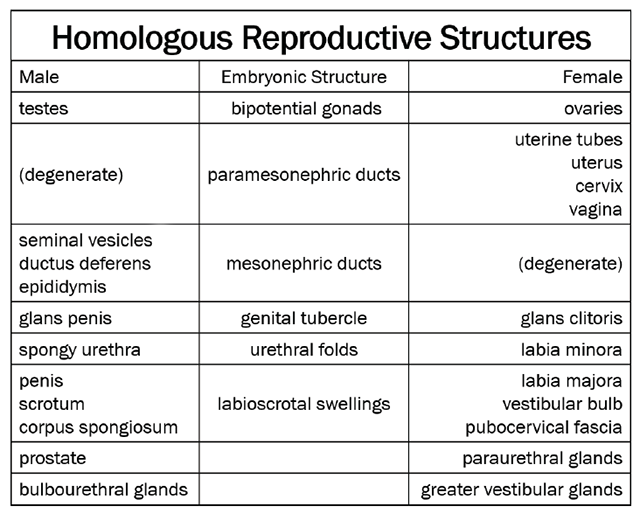
This table lists the embryonic structure (where known), as well as the female and male “end results” for each.
Clinical Connection: Intersex
 Because expression errors from a single gene (like SRY) are always possible, it should not surprise you that individuals exist whose gonad development is somewhere in between male and female. These individuals used to be called hermaphrodites or pseudohermaphrodites; the current term is intersex. They are born with reproductive anatomy that doesn’t fit typical definitions of male or female. For example, a person might appear to be female on the outside but have male-typical anatomy on the inside, or vice-versa. Some appear have both male and female external genitalia and/or may have both ovarian and testicular tissue. A surprisingly large number of people are born intersex — about 1.7% of the population or 5.6 million people in the US (about as common as having red hair). Some are identified at birth, more won’t show up until later in life, and some live their entire life unaware.
Because expression errors from a single gene (like SRY) are always possible, it should not surprise you that individuals exist whose gonad development is somewhere in between male and female. These individuals used to be called hermaphrodites or pseudohermaphrodites; the current term is intersex. They are born with reproductive anatomy that doesn’t fit typical definitions of male or female. For example, a person might appear to be female on the outside but have male-typical anatomy on the inside, or vice-versa. Some appear have both male and female external genitalia and/or may have both ovarian and testicular tissue. A surprisingly large number of people are born intersex — about 1.7% of the population or 5.6 million people in the US (about as common as having red hair). Some are identified at birth, more won’t show up until later in life, and some live their entire life unaware.
Clinical Connection: Cryptorchidism
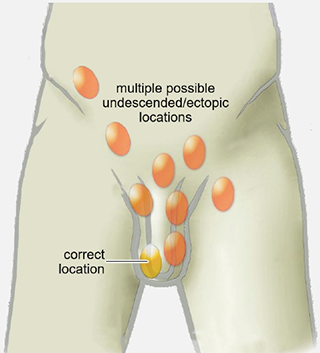 The descent of male testes from an embryonic position in the abdomen into the scrotal sac is important clinically for two primary reasons. During fetal growth, testes move first to the inguinal canal between weeks 8 and 12, then downward through the inguinal canal during weeks 12 to 28, and finally from the inguinal canal into the scrotum during weeks 28 through 40. The failure of one or both testes to descend fully into the scrotum by birth is called cryptorchidism or, more simply, undescended testis (UDT).
The descent of male testes from an embryonic position in the abdomen into the scrotal sac is important clinically for two primary reasons. During fetal growth, testes move first to the inguinal canal between weeks 8 and 12, then downward through the inguinal canal during weeks 12 to 28, and finally from the inguinal canal into the scrotum during weeks 28 through 40. The failure of one or both testes to descend fully into the scrotum by birth is called cryptorchidism or, more simply, undescended testis (UDT).
Cryptorchidism occurs in 3-4% of full-term male births; about three-quarters of these are unilateral (left-sided more common than right) and about one-quarter are bilateral (both testes fail to descend fully). In pre-term male births, the 3-4% figure increases to 30% (by the time these infants reach what would have been their birth dates, most have resolved and the prevalence is once again about 3-4%). In about 75% of cases, the missing testis completes its descent into the scrotum by the age of three months; about 25% will require surgery, usually done between six and twelve months of age.
Resolving cryptorchidism is important because the condition increases the risk, later in life, of the following conditions:
- Testicular cancer – An undescended testis has an eight times greater risk of developing testicular cancer. While this increase is significant, the risk of testicular cancer is remains below 1 per 100.
- Testicular torsion – While rare, testicular torsion is ten times more likely in an undescended testis.
- Infertility – Because sperm production functions best at 2-3°C below body temperature, an undescended testis is too warm to carry out this process efficiently. While bilateral cryptorchidism clearly presents a significant challenge to male fertility, even a unilateral case can lower sperm count enough to prevent successful conception.
Clinical Connection: Inguinal Hernia
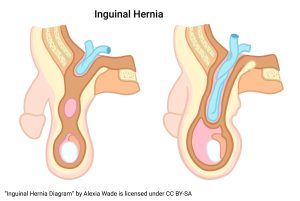 The second reason the descent of male testes through the inguinal canal into the scrotal sac is important clinically relates to the risk of inguinal hernia. After passage of the testis, the inguinal canal becomes the spermatic cord and remains, mechanically, a weak point in the lower abdominal wall. An inguinal hernia occurs when a loop of bowel finds its way into the remnants of the inguinal canal. It stands to reason, then, that inguinal hernias are seven times more common in men than women (oddly, they occur 4.5 times more frequently on the left side than the right).
The second reason the descent of male testes through the inguinal canal into the scrotal sac is important clinically relates to the risk of inguinal hernia. After passage of the testis, the inguinal canal becomes the spermatic cord and remains, mechanically, a weak point in the lower abdominal wall. An inguinal hernia occurs when a loop of bowel finds its way into the remnants of the inguinal canal. It stands to reason, then, that inguinal hernias are seven times more common in men than women (oddly, they occur 4.5 times more frequently on the left side than the right).
Sometimes, the herniated loop of bowel can be carefully reduced manually (pushed out of the inguinal canal back into the abdominal cavity), but will frequently herniate again, necessitating surgery. Herniated tissue that becomes trapped quickly becomes a medical emergency resolved only by abdominal surgery to reduce the hernia, resect a section of necrotic bowel (often), and structurally reinforce the body wall to prevent recurrence.
Media Attributions
- U20-010b SRY Gene and Sex © Hutchins, Jim is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-011 Internal Reproductive Organ Development © Wade, Alexia is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-012 External Genitalia Development © Wade, Alexia is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-013 Table of Homologous Structures Male Female © Winterton, Brad is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-014 Intersex Diagram © Wade, Alexia is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-015 Undescended Testicle © Lamiot adapted by Brad Winterton is licensed under a CC BY-SA (Attribution ShareAlike) license
- U20-016 Inguinal Hernia © Wade, Alexia is licensed under a CC BY-SA (Attribution ShareAlike) license

