Glomerular Filtration
Objective 4
Describe the structures by which blood is filtered through the glomerular membrane. Compare and contrast the composition of blood and glomerular filtrate. Identify the pressures that contribute to the glomerular net-filtration pressure. Describe the three regulatory mechanisms to control the glomerular filtration rate (GFR).
 The first step of filtering blood occurs at the glomerulus. Filtering occurs by size; smaller substances pass into the filtrate and larger substances remain behind. Imagine you made an interesting version of macaroni and cheese. Deciding to be healthier, you add frozen peas and shredded carrots to your macaroni as it's cooking. A very impressive three-layer strainer helps you strain the water from this concoction. The first layer has holes large enough that the macaroni stays in the strainer, but everything else gets through. The next layer has even smaller holes that keep the peas behind, the water and small carrots pass through. The last strainer has very small holes. These holes keep the carrots behind. The water has successfully been drained while you have kept the part you want to eat. You may not want to try this anytime soon unless you are feeling very experimental.
The first step of filtering blood occurs at the glomerulus. Filtering occurs by size; smaller substances pass into the filtrate and larger substances remain behind. Imagine you made an interesting version of macaroni and cheese. Deciding to be healthier, you add frozen peas and shredded carrots to your macaroni as it's cooking. A very impressive three-layer strainer helps you strain the water from this concoction. The first layer has holes large enough that the macaroni stays in the strainer, but everything else gets through. The next layer has even smaller holes that keep the peas behind, the water and small carrots pass through. The last strainer has very small holes. These holes keep the carrots behind. The water has successfully been drained while you have kept the part you want to eat. You may not want to try this anytime soon unless you are feeling very experimental.
 Just like our three-layered strainer, the glomerulus in the kidneys also has three layers to keep some substances out of the filtrate while allowing smaller substances to pass through. The three layers of tissue that form the filtration membrane are comprised of:
Just like our three-layered strainer, the glomerulus in the kidneys also has three layers to keep some substances out of the filtrate while allowing smaller substances to pass through. The three layers of tissue that form the filtration membrane are comprised of:
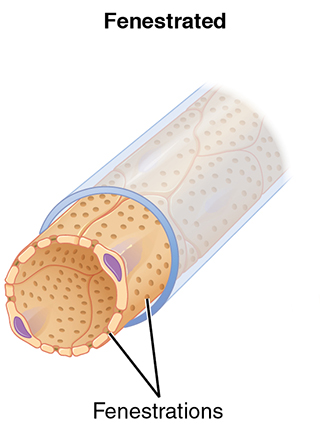
- the endothelium of the glomerular capillaries. These specialized capillaries are fenestrated capillaries, so they are much more permeable than the more common continuous capillaries of the vascular system.
- a layer of connective tissue (basal lamina) is sandwiched between the endothelium and the podocytes.
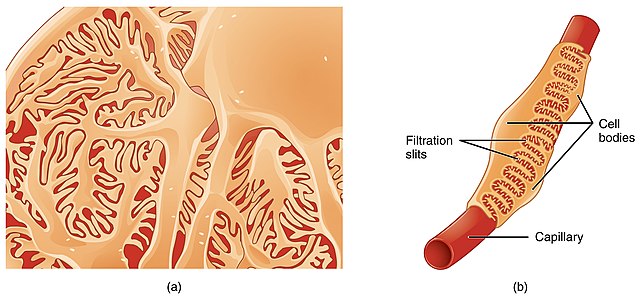
- the outermost layer of the capsule is formed by the visceral layer of the glomerular capsule. This tissue is formed by unique cells called podocytes. These cells have numerous foot-processes (pedicels) that extend from the podocytes. The pedicels have small spaces between them called filtration slits. The permeability of the membrane can be controlled by the amount of space provided by the foot-processes of podocytes.
The capillary endothelium allows for the passage of fluid and blood solutes (such as ions, glucose, and urea) into the glomerular capsule but does not allow formed elements (blood cells and platelets) to pass through. Very few proteins can pass through this three-layer membrane.
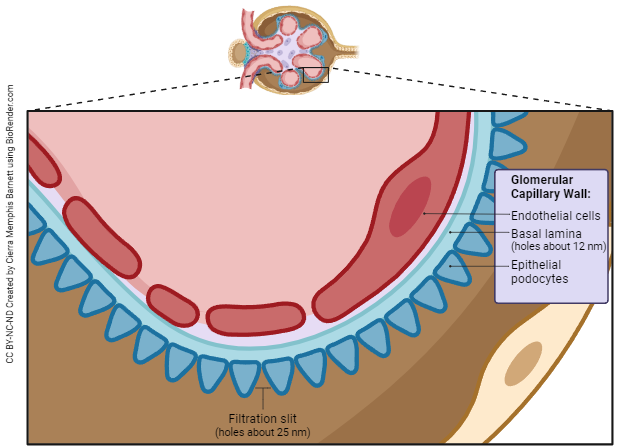
By working together, these three layers of the glomerular membrane effectively restrict the passage of any substance larger than 40,000 molecular weight (40 kDa) into the glomerular filtrate. Capillary blood pressure is the primary driving force that pushes fluids and solutes through the glomerular membrane.
Glomerular filtrate is blood minus the formed elements and the majority of plasma proteins. Normally, 16-20% of the plasma in the afferent arterioles becomes filtrate.
The Glomerular Filtration Rate (GFR)
The amount of glomerular filtrate formed each minute is called the glomerular filtration rate or GFR. The body averages about 115 ml/min, with men having slightly higher GFR than women. This results in approximately 180 L of glomerular filtrate produced per day. As a side note, daily urine output is 1-2 L. Most of this filtrate is reabsorbed back into the bloodstream. This is a good thing or we would be spending most of our time in the bathroom!
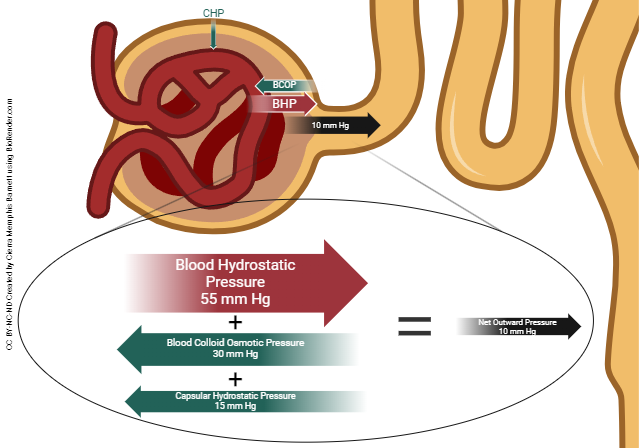
Three pressures contribute to glomerular filtration; one pressure encourages filtration, two oppose it. These pressures are the:
- Glomerular blood hydrostatic pressure: This is simply the pressure of the blood as it enters the glomerulus. This force is pushing blood through the glomerulus
- Blood colloid osmotic pressure: Large proteins that don’t pass through the glomerular membrane create osmotic pressure, pulling fluid back into the glomerular capillaries. Because the water concentration is higher in the capsule than in the blood, water moves from the capsule back into the blood, creating an osmotic pressure. This force opposes the blood hydrostatic pressure.
- Capsular hydrostatic pressure: Like a balloon filled with water, filtrate accumulating in the capsular space produces its own pressure, which pushes back on the glomerular capillaries.
The net filtration pressure is the “net” result of all three influences. The net filtration pressure is what determines whether urine formation takes place. The lower the filtration pressure, the less urine is formed. If the net pressure is zero or negative, it is termed as renal failure.
In a healthy kidney, and under normal circumstances, the pressure generated by the heart (glomerular blood hydrostatic pressure) is greater than opposing forces. The end result of these pressure differences is the passage of fluid and solutes out of the glomerular capillaries and into the glomerular space.
Renal Autoregulation of GFR
The GFR needs to be held constant. If the GFR drops too low, there is a buildup of waste products in the blood. If the GFR is too high, the tubules may not have adequate time to reabsorb essential nutrients, allowing them to be lost in the urine.
Blood pressure may fluctuate quite a bit throughout the day. Things like climbing four flights of stairs, test anxiety, or not even getting enough sleep might elevate blood pressure. The kidneys need to keep a constant glomerular filtration rate, even with normal fluctuations of blood pressure. To maintain an appropriate GFR, the body uses three mechanisms: renal autoregulation, neural regulation, and hormonal regulation.
Renal autoregulation
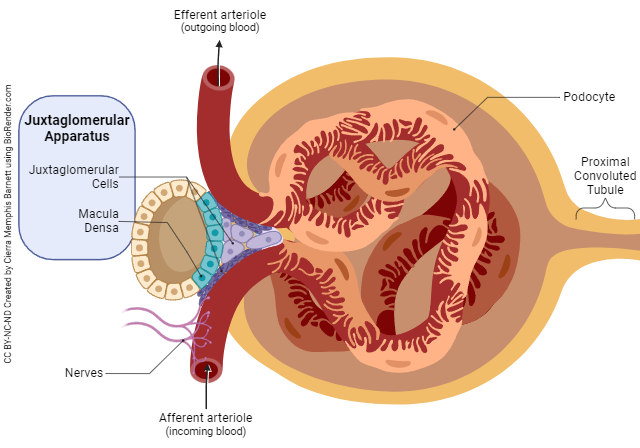
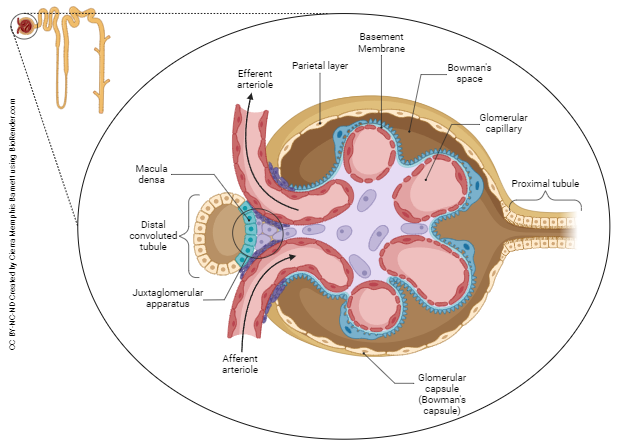
The kidneys can dilate or constrict the afferent and efferent arterioles to keep the blood pressure constant. If the blood pressure is high, the afferent arteriole constricts. This narrows the lumen reducing the blood flow to the glomerulus, thus reducing the glomerular filtration rate. If blood pressure is low, the afferent arteriole dilates increasing renal blood flow and increasing the glomerular filtration rate. Another component of renal autoregulation is control of the GFR by tubuloglomerular feedback. This is regulated by the juxtaglomerular apparatus (JGA). If the GFR is high, electrolytes and water do not have time to be adequately reabsorbed as they pass through the distal convoluted tubule. If a hose were turned on so that the water is slowly dripping, there would be plenty of time to catch the water in a bucket. If a fire hose were turned on, it would be a little harder to catch this water. If the GFR is high, substances are passing through the nephron so fast that they are not adequately reabsorbed. The cells of the macula densa, in the ascending limb of the nephron, detect the increased amounts of electrolytes and water. To minimize water and electrolyte loss, the JGA inhibits the release of the gaseous neurotransmitter NO (nitric oxide). NO is a potent vasodilator. When less NO is released, arterioles constrict. Less blood flows through the afferent arteriole with a subsequent decrease in the GFR. This increases the time to reabsorb electrolytes and water in the tubules.
Neural regulation
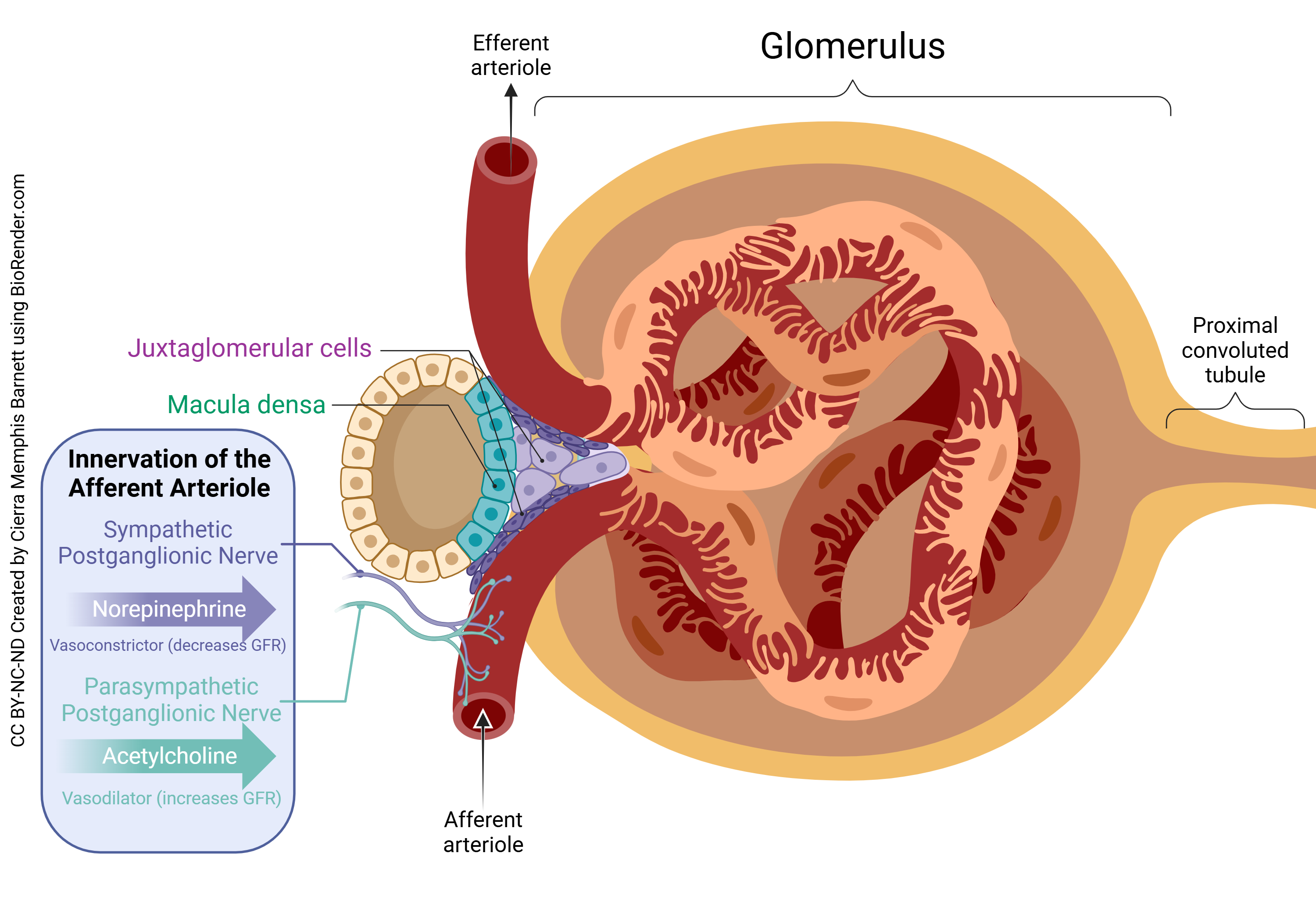
The kidneys are interesting. The renal blood vessels are mainly controlled by the sympathetic nervous system. Norepinephrine released from sympathetic post-ganglionic neurons causes both the afferent and efferent arterioles to constrict which decreases the GFR. Remember that when you’re running from a bear, you don’t have time to pee! And it is a good idea to reabsorb as much water as possible to keep blood pressure high. At rest, this influence is minimal, but with greater norepinephrine release, there is greater constriction of the afferent arteriole, therefore less blood flow to the glomerulus and a lower GFR. Conversely, during periods of relaxation, there is less sympathetic nervous system output. In the kidneys, this means less norepinephrine is released. Remember that norepinephrine is a vasoconstrictor. If less is released, the afferent and efferent arterioles relax (dilate), which increases the GFR (and more urine is produced).
Hormonal Regulation
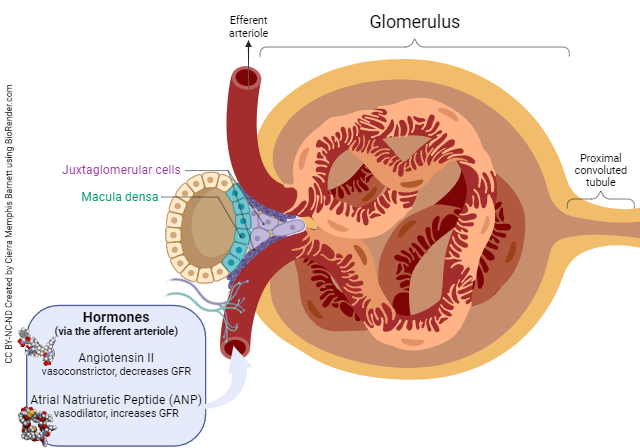 Two main hormones contribute to the GFR, angiotensin II and atrial natriuretic peptide (ANP). Remember in the RAAS system, angiotensin II acts to raise blood pressure by acting as a vasoconstrictor. With increased amounts of angiotensin II, the afferent arteriole vasoconstricts, decreasing the GFR (less blood is getting through). ANP is produced by the cells of the atria of the heart in response to increased blood volume. ANP acts as a vasodilator thereby decreasing blood pressure. Under the influence of ANP the afferent arteriole dilates, allowing more blood flow to the glomerulus. The end result is an increased GFR (more blood gets through), which promotes water and electrolyte dumping in the urine. Sodium (Na) is called natrium in Latin, and uretic means "pertaining to the urine", so this atrial peptide promotes shedding of sodium (natrium) in the urine (uretic).
Two main hormones contribute to the GFR, angiotensin II and atrial natriuretic peptide (ANP). Remember in the RAAS system, angiotensin II acts to raise blood pressure by acting as a vasoconstrictor. With increased amounts of angiotensin II, the afferent arteriole vasoconstricts, decreasing the GFR (less blood is getting through). ANP is produced by the cells of the atria of the heart in response to increased blood volume. ANP acts as a vasodilator thereby decreasing blood pressure. Under the influence of ANP the afferent arteriole dilates, allowing more blood flow to the glomerulus. The end result is an increased GFR (more blood gets through), which promotes water and electrolyte dumping in the urine. Sodium (Na) is called natrium in Latin, and uretic means "pertaining to the urine", so this atrial peptide promotes shedding of sodium (natrium) in the urine (uretic).
Media Attributions
- U19-012 Laboratory Sieves © User:BMK is licensed under a CC BY-SA (Attribution ShareAlike) license
- U19-013 Fenestrated Capillary © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter adapted by Jim Hutchins is licensed under a CC BY (Attribution) license
- U19-014 Podocytes © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U19-015 Layers of the Glomerulus v2 © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U19-016 Renal Corpuscle © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U19-017 Pressure in the Glomerulus © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U19-010 Juxtaglomerular Apparatus and GFR © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U19-019 Neural Regulation of GFR v2 © Cierra Memphis Barnett | BioRender is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U19-020 Hormonal Regulation of GFR © Barnett, Cierra Memphis is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license

