Female Reproductive Cycle
Objective 8
Correlate the events of the ovarian and uterine cycles, including hormonal controls.
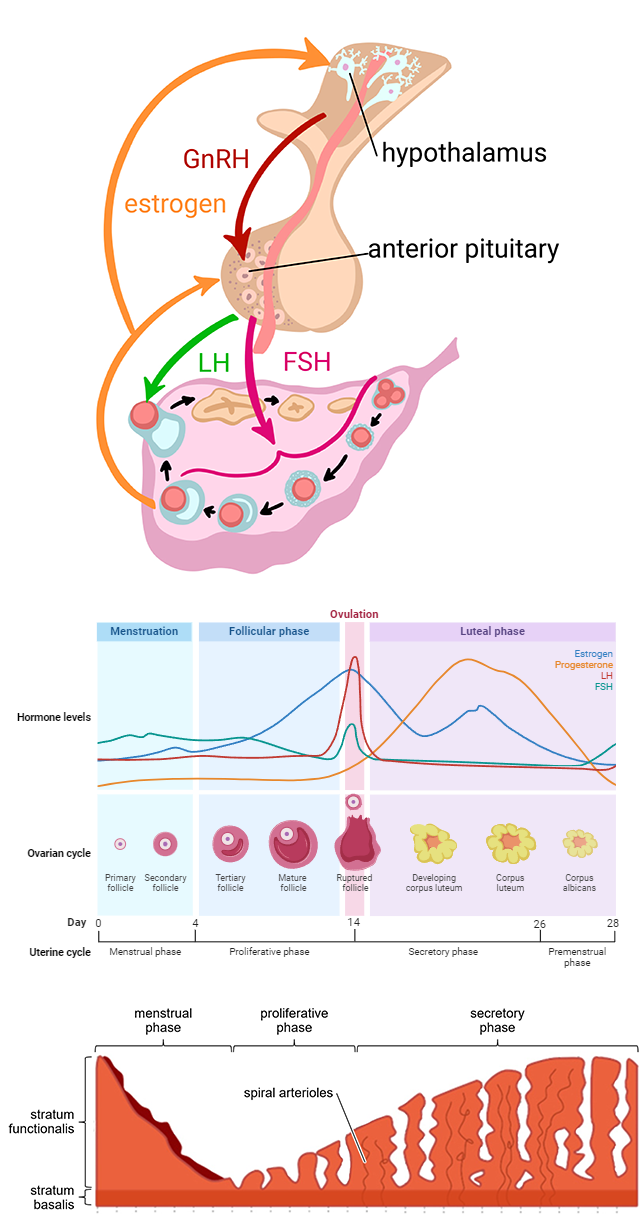 Early in the uterine cycle, during the last half of the menstrual phase and the beginning of the proliferative phase, GnRH from the hypothalamus triggers FSH release from the anterior pituitary. The FSH (follicle stimulating hormone) stimulates a primordial follicle in one ovary to develop into a primary follicle, then a secondary follicle, and, finally, a mature follicle. FSH levels don’t get very high; it doesn’t take much.
Early in the uterine cycle, during the last half of the menstrual phase and the beginning of the proliferative phase, GnRH from the hypothalamus triggers FSH release from the anterior pituitary. The FSH (follicle stimulating hormone) stimulates a primordial follicle in one ovary to develop into a primary follicle, then a secondary follicle, and, finally, a mature follicle. FSH levels don’t get very high; it doesn’t take much.
During this maturation process, the maturing follicle secretes increasing amounts of estrogens, which promote proliferation of the stratum functionalis (proliferative phase). At the same time, the estrogens feed back to the hypothalamus and anterior pituitary to continue release of FSH so the follicle will fully mature.
When estrogens reach a certain level, about day 14, the anterior pituitary releases a sudden surge of FSH and, more importantly, LH (luteinizing hormone), which causes the mature follicle to burst, release the secondary oocyte – ovulation – and then become a corpus luteum.
The corpus luteum is a temporary endocrine organ that secretes progesterone (pro-, in favor of; -gestation) and estrogens. The addition of progesterone maintains the proliferated stratum functionalis and stimulates it to begin secreting (secretory phase) to further prepare for implantation. This is sort of a uterine “waiting period” while the oocyte is traversing the uterine tube and might, or might not, encounter sperm and undergo fertilization.
If no implantation occurs, the corpus luteum begins to degenerate, and progesterone and estrogen production drops significantly. The decrease in these two hormones causes vasoconstriction of the spiral arterioles of the stratum functionalis, depriving the tissue of oxygen and nutrients. In response, the stratum functionalis is shed, beginning the menstrual phase again.
If implantation does occur, the corpus luteum hangs around a bit longer, continuing to release its two hormones until the placenta develops and takes over production of estrogens and progesterone.
 Two additional luteal (ie, produced by the corpus luteum) hormones we haven’t discussed yet are inhibin and relaxin. Inhibin, as the name suggests, inhibits something – in this case, it inhibits the release of FSH and LH from the anterior pituitary (we don’t want another follicle developing/ovulating until the current cycle is complete and implantation has not occurred). Relaxin relaxes the smooth muscle of the uterus to help with implantation. Relaxin also plays a key role during childbirth (parturition), when it relaxes the cervix and the pubic symphysis in preparation for delivery.
Two additional luteal (ie, produced by the corpus luteum) hormones we haven’t discussed yet are inhibin and relaxin. Inhibin, as the name suggests, inhibits something – in this case, it inhibits the release of FSH and LH from the anterior pituitary (we don’t want another follicle developing/ovulating until the current cycle is complete and implantation has not occurred). Relaxin relaxes the smooth muscle of the uterus to help with implantation. Relaxin also plays a key role during childbirth (parturition), when it relaxes the cervix and the pubic symphysis in preparation for delivery.
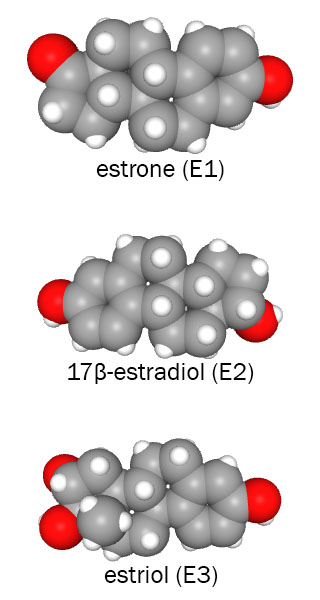
Another note on hormone nomenclature: you might have noticed that we always refer to “estrogens” plural. This is because there are three different chemicals that are called estrogens. In non-pregnant females, 17β-estradiol (E2), made from testosterone, is the predominant estrogen. During menopause and later (as the ovaries are no longer producing E2), estrone (E1) is the main form found in the body. During pregnancy, the main estrogen is estriol (E3), which is actually made by the fetal liver.
Media Attributions
- U20-037a Composite Image Showing Female Reproductive Cycles © Wade, Alexia; Lopez, Rosalba; Hutchins, Jim; Speck-Made and BioRender is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U20-037b Estrogens Space-filling © PubChem is licensed under a Public Domain license

