Coverings and Fluids of the Brain
Objective 8
Describe the blood supply of the brain and the distribution of cerebrospinal fluid (CSF).
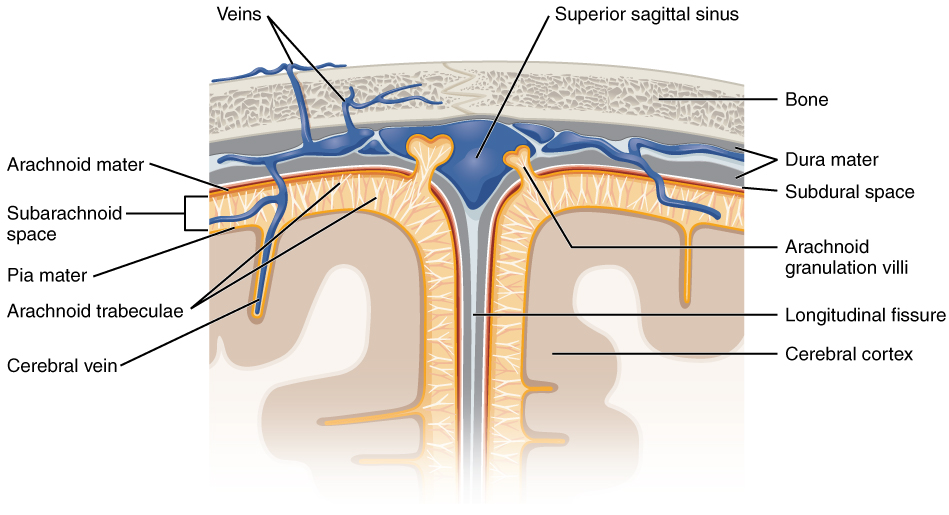
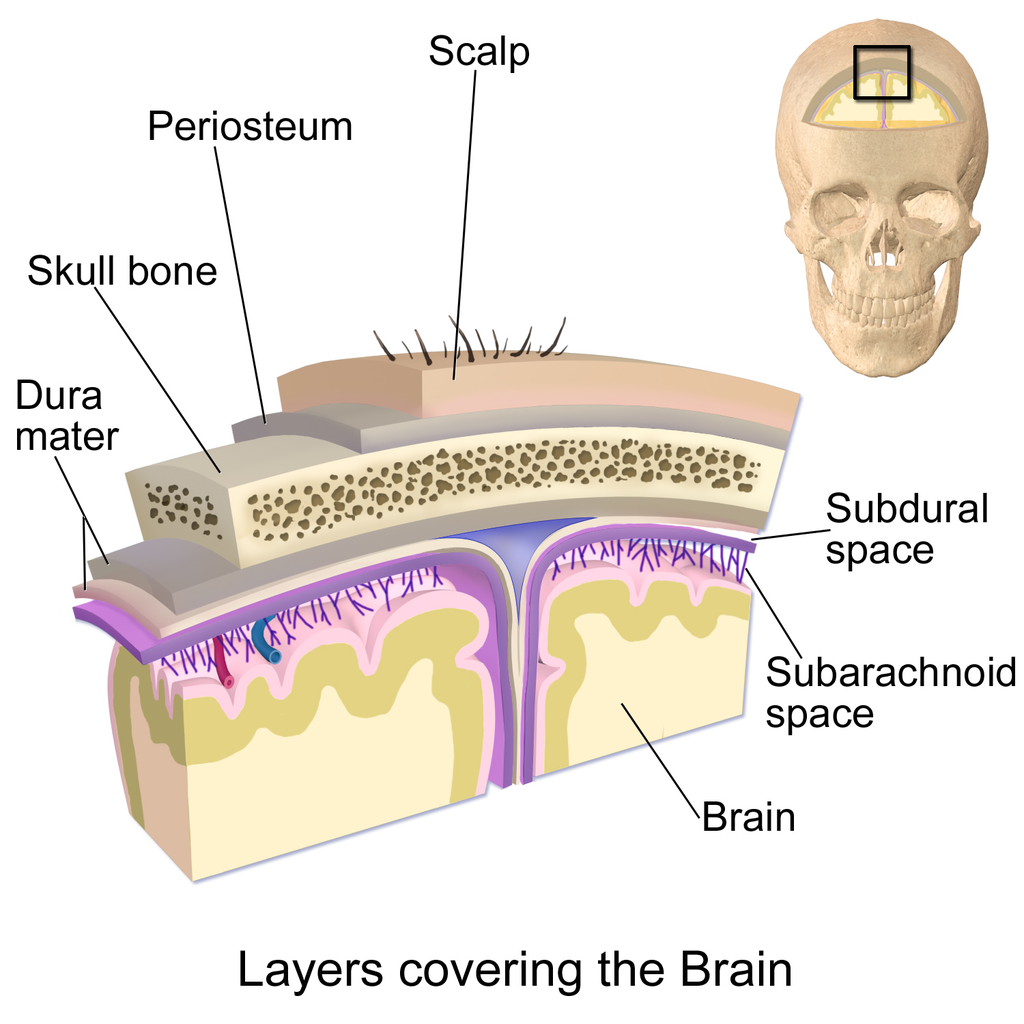
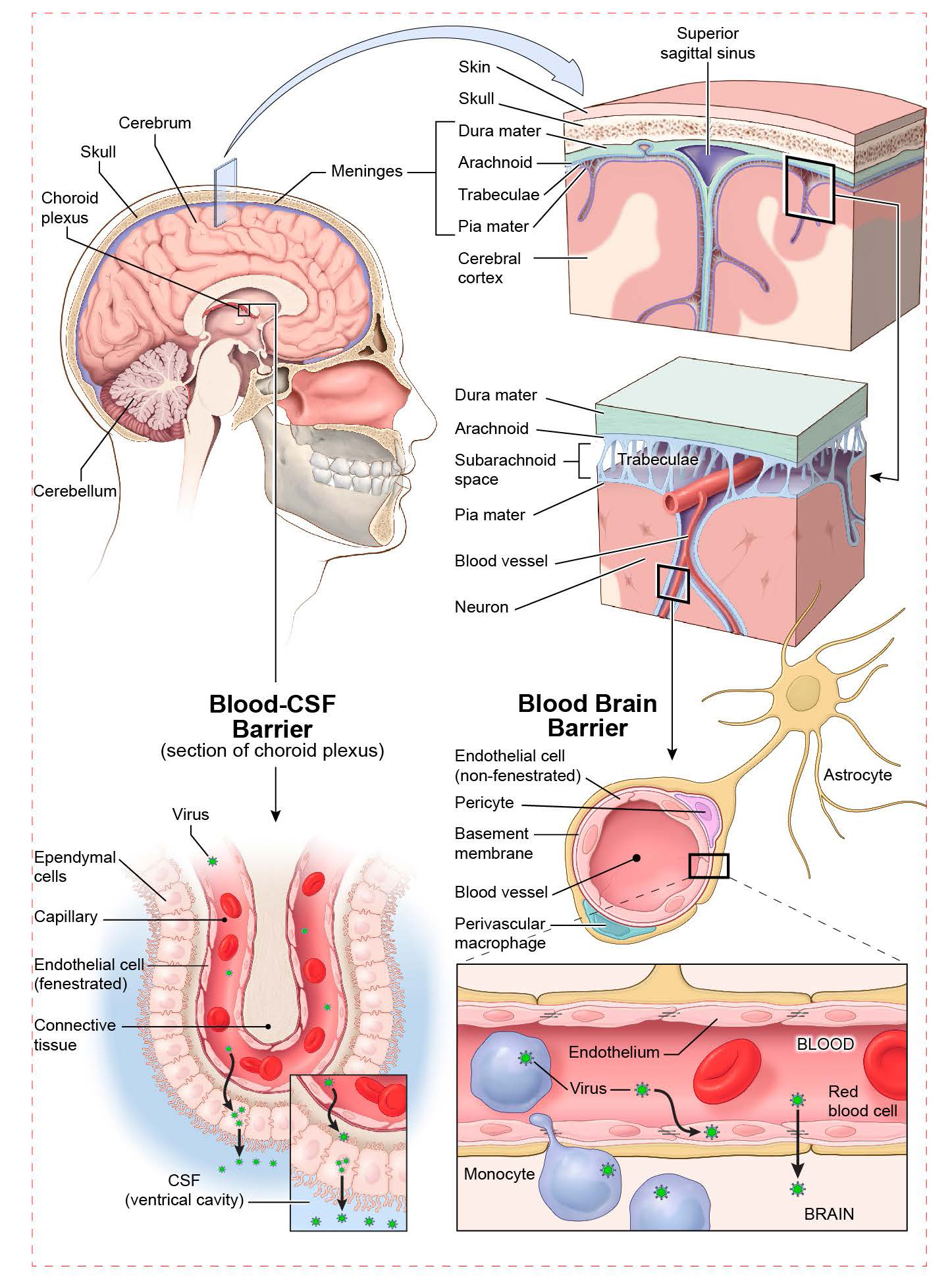
The brain is covered by a three-layered bag. These layers are collectively called the meninges (singular meninx).
From the skull to the surface of the brain, the meninges comprise:
- dura mater (Latin: “tough mother”), a leathery covering;
- arachonoid mater (“spiderweb mother”), which resembles a wet spider web and is normally filled with cerebrospinal fluid (CSF);
- pia mater (“delicate mother”), like a coating of paint on the surface of the brain, which cannot be separated from the substance (parenchyma) of the brain.
How in the world did these meninges get such strange names? They were originally named by a Persian anatomist, Ali ibn Abbas, in the 10th century. There is no Arabic word for “membrane” so he wrote al umm, “the mother”, “the womb”. The European translators rendered this literally into the Latin “mother” instead of figuratively into the original meaning of mother as a womb, swaddling or covering.
The term epidural, as in epidural anesthesia, means “on top of the dura”. Epidural anesthesia is a deadening agent applied on top of (“epi-”) the dura mater. Patients who suffer bleeding into the brain may have blood collecting in the epidural space (between the skull and dura); tearing apart the subdural region (between the dura and arachnoid); or filling the subarachnoid space (between the arachnoid and the pial surface of the brain).
 The brain has a series of hollow spaces. These are called ventricles.
The brain has a series of hollow spaces. These are called ventricles.
Together, the ventricles and subarachnoid space are filled with cerebrospinal fluid (CSF), a filtrate of blood plasma that cushions and supports the brain, as well as supplying a favorable ionic environment for neurons (that is, isotonic and mostly NaCl). Scientists estimate that the brain, at an average 1400 g, weighs only 50 g when buoyed by CSF.
Cerebrospinal fluid is made in the choroid plexus, a specialized tissue that is found mainly in the lateral ventricles and fourth ventricle. There, the blood is filtered by ependymal cells, a type of glial cell.
CSF is almost identical to plasma; it is slightly lower in glucose and amino acids than plasma, and much lower in protein.
CSF circulates and is turned over about four times a day. It can be sampled with relatively little risk to the patient from the lumbar cistern, a large sac containing the cauda equina floating in CSF which is accessed from the intervertebral space between L2 and L3. Because of the circulation of CSF, a lumbar puncture may detect bleeding that originated (for example) in the subarachnoid space around frontal cortex.
The resorption of CSF is thought to occur in the arachnoid villi, a collection of structures along the midline of the superior aspect of the skull.
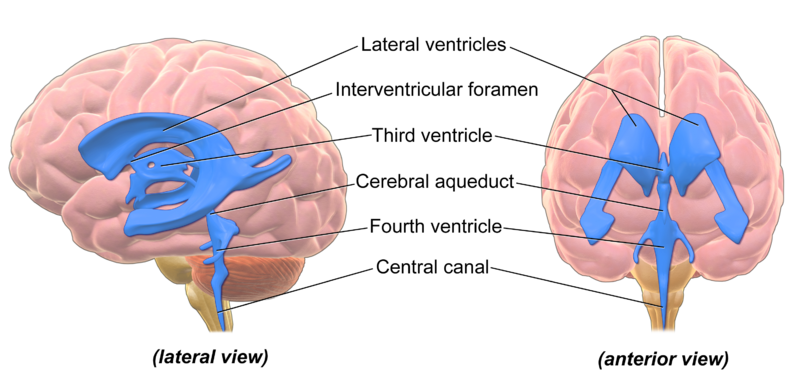
The ventricles include:
- Lateral ventricles, shaped like the letter C with a tail. This pair of ventricles is located beneath the white matter of cerebral cortex. There is no “first” or “second” ventricle, but there should be!
- A third ventricle, which is a slit-like space between the two eggs of the thalamus.
- A fourth ventricle, between the brainstem and cerebellum.
The ventricles are connected to each other by apertures or foramina. The lateral ventricles and third ventricle connect via the interventricular foramina. The third and fourth ventricles are joined by the cerebral aqueduct. The fourth ventricle communicates with the subarachnoid space surrounding the brain and spinal cord via three apertures: two lateral apertures and a single median aperture.
Hydrocephalus can also result from overproduction of CSF, or from slow resorption of CSF. Remember from an earlier objective that CSF can be sampled from the lumbar cistern, the subarachnoid space which contains the free-floating nerve roots of the cauda equina at the caudal end of the spinal cord.
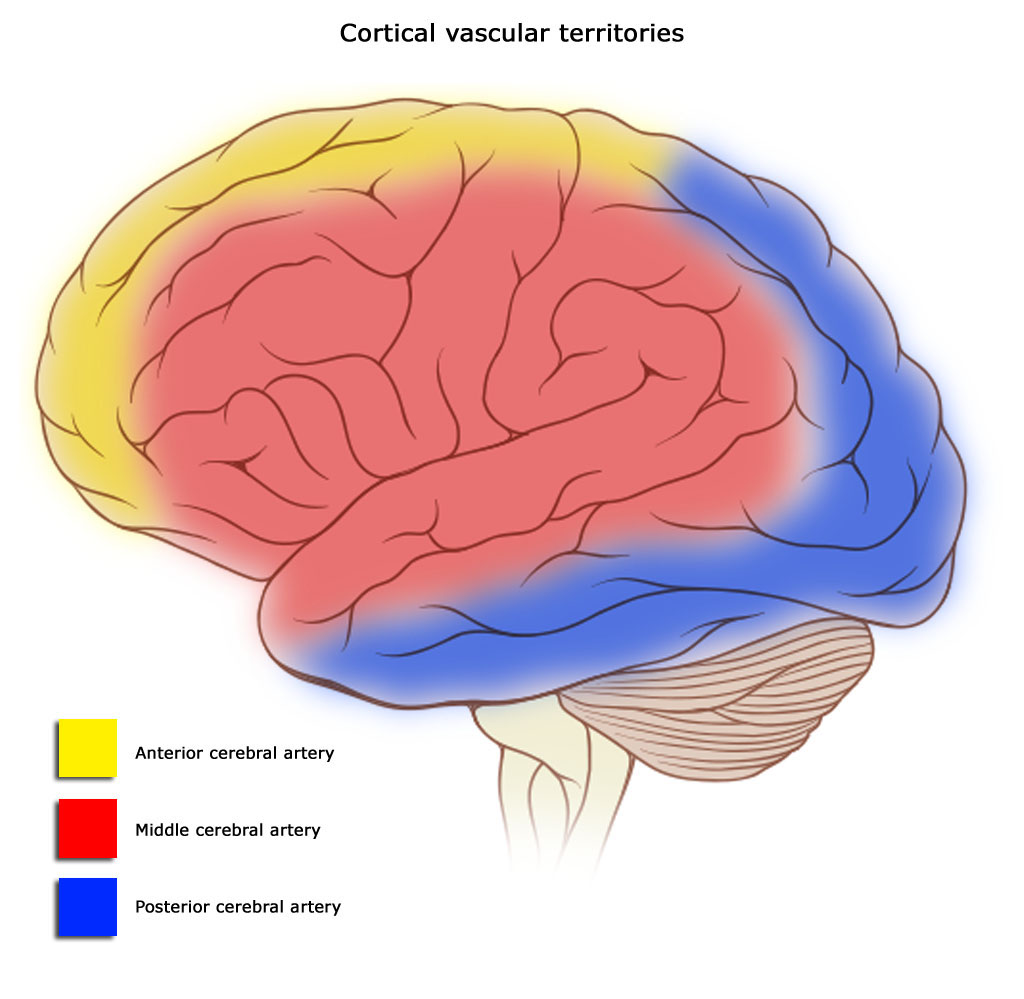
The blood supply to cortex comes from three major arteries:
- the anterior cerebral artery (ACA);
- the middle cerebral artery (MCA);
- the posterior cerebral artery (PCA).
Territories of these three major arteries are shown in the diagram.
All three of these arteries originate from an anastomosis (joining of blood vessels) at the base of the brain called the Circle of Willis. The Circle of Willis is fed by the anterior circulation, coming from the carotid arteries which rise through the ventral neck; and the posterior circulation, which runs through the vertebral arteries. The vertebral arteries anastomose at the medulla to form the basilar artery.
Branches of the basilar supply the brainstem. The basilar branches at the midbrain level to form the posterior cerebral arteries.
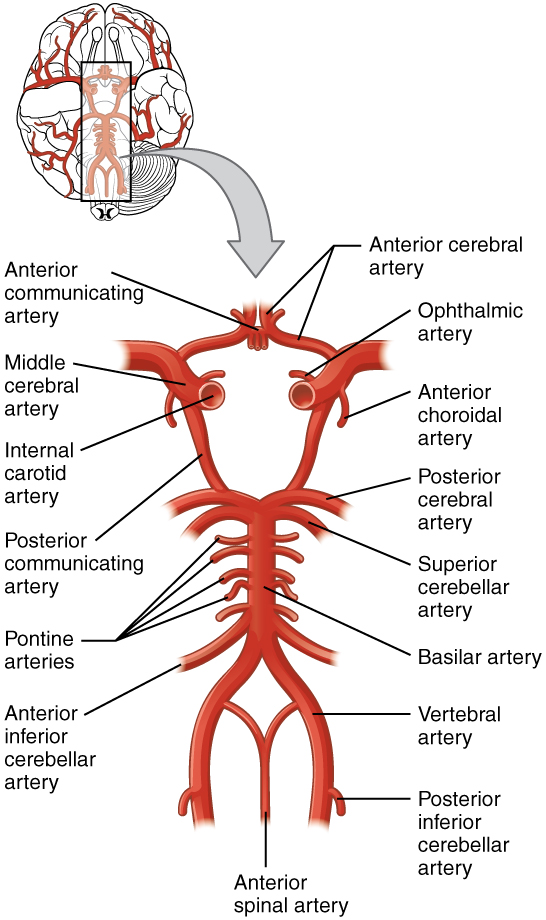
The carotid arteries branch and turn sharply as they reach the base of the brain, forming the anterior and middle cerebral arteries.
All these arteries are connected by a single anterior communicating artery and a pair of posterior communicating arteries, completing the circle.
This image is included just to show you the components of the Circle of Willis; you do not need to know the names of these arteries for this course.
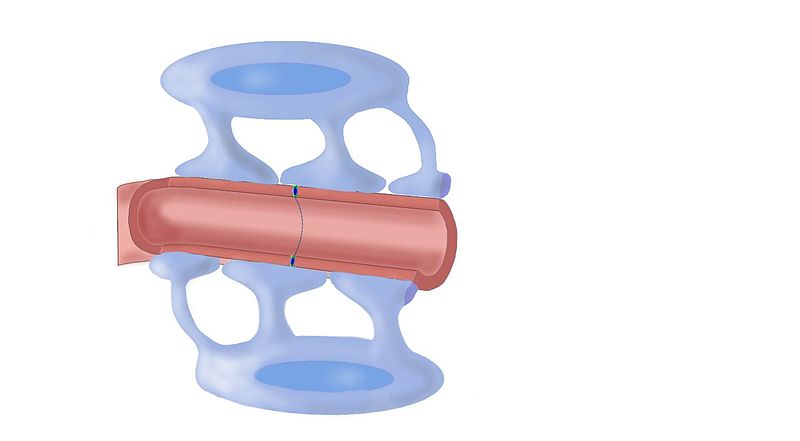
 The brain tightly regulates which substances are allowed into the CNS. The blood-brain barrier (BBB) is a collaboration between the lining of capillaries and the end-feet of astrocytes. It keeps most substances in the bloodstream from entering the brain. There are pumps to bring glucose, some amino acids, and water into the brain. Lipid-soluble molecules can pass through simple diffusion. Waste products are pumped from the brain into the blood. Everything else is kept out, unless the brain is diseased.
The brain tightly regulates which substances are allowed into the CNS. The blood-brain barrier (BBB) is a collaboration between the lining of capillaries and the end-feet of astrocytes. It keeps most substances in the bloodstream from entering the brain. There are pumps to bring glucose, some amino acids, and water into the brain. Lipid-soluble molecules can pass through simple diffusion. Waste products are pumped from the brain into the blood. Everything else is kept out, unless the brain is diseased.
 One exception is the area postrema, also called the “vomiting center.” This small area of the medulla oblongata has no blood-brain barrier, which gives it access to any toxins or irritants which might be circulating in the blood. If it detects them, then it triggers emesis (vomiting) through the nearby vagus nerve.
One exception is the area postrema, also called the “vomiting center.” This small area of the medulla oblongata has no blood-brain barrier, which gives it access to any toxins or irritants which might be circulating in the blood. If it detects them, then it triggers emesis (vomiting) through the nearby vagus nerve.
The BBB is nice to have, but one problem is that it can keep out drugs (particularly antibiotics) that we might want to use to help a patient. It is important to design drugs to be used in the brain so that they can circumvent this barrier. For example, if a bacterium penetrates the blood-brain barrier, it can be difficult to deliver antibiotics to the area of infection.
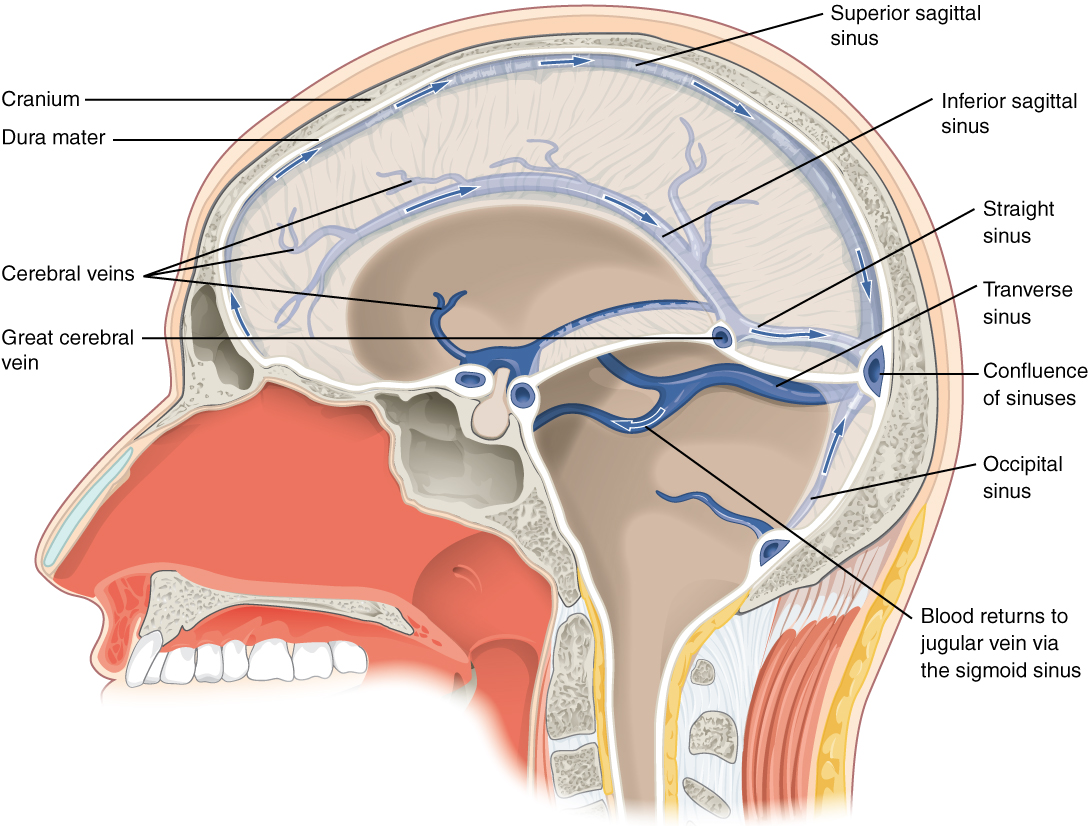 The brain has few veins that resemble the round tubes found in other parts of the body. Rather, in most locations, blood collects in sinuses, open areas that collect deoxygenated blood from a network of feeder vessels.
The brain has few veins that resemble the round tubes found in other parts of the body. Rather, in most locations, blood collects in sinuses, open areas that collect deoxygenated blood from a network of feeder vessels.
Two main sinuses, found along the midline, are the superior sagittal sinus and the inferior sagittal sinus. A much smaller occipital sinus drains blood from the occipital area and runs along the midline as well.
Two pairs of sinuses pass laterally. The more superficial pair are the transverse sinuses. The deeper pair are the great cerebral veins (of Galen). These form a T-shaped arrangement with the straight sinus.
The straight sinus, the occipital sinus, the superior sagittal sinus, and the two transverse sinuses all come together at a single point called the confluence of sinuses. The sigmoid sinus connects all these structures to the jugular veins, which ultimately drain the deoxygenated blood from the brain.
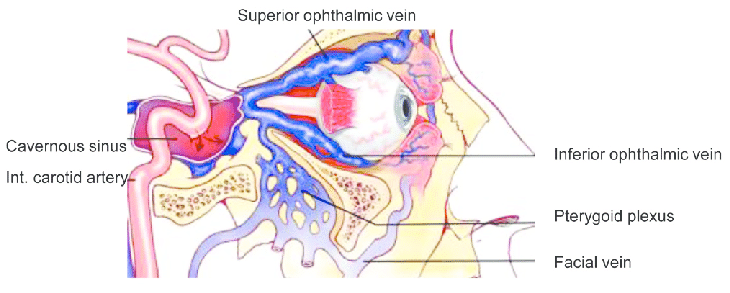
The cavernous sinuses, near the eyes on either side of the head, are venous sinuses that contain several important structures: several cranial nerves and the internal carotid arteries. These sinuses receive drainage from the area of the nose and eyes.
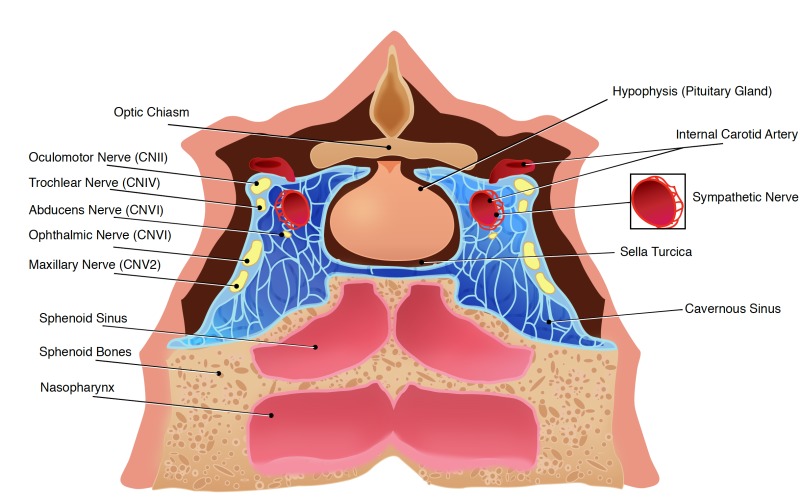
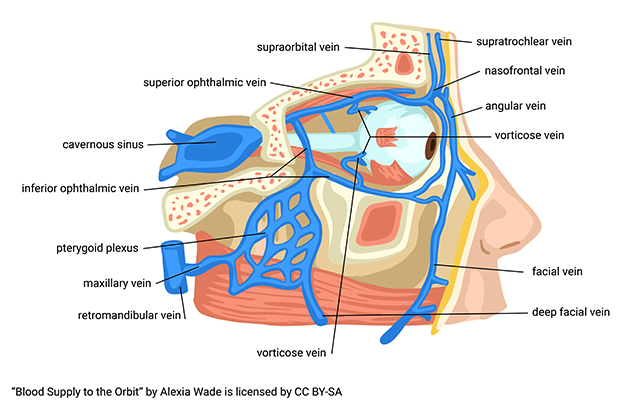
For that reason, a roughly-defined three-sided region centered around the nose carries a lurid and attention-grabbing name: The Triangle of Death. The reason for this emo name is because an infection in this area can easily invade the cavernous sinus and from there the important structures carried inside. If you’ve ever been told you’ll die if you pop nose zits, this is why.
Media Attributions
- U11-090 Meninges © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U11-091 Brain Layers © BruceBlaus is licensed under a CC BY (Attribution) license
- U11-092 Ventricles © Hoofring, Alan is licensed under a Public Domain license
- U11-093 Ventricles Brain © BruceBlaus is licensed under a CC BY (Attribution) license
- U11-094 Cerebral Vascular Territories © Gaillard, Frank Dr. is licensed under a CC BY-SA (Attribution ShareAlike) license
- U11-095 Circle of Willis © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U11-096 Drugs and Blood Brain Barrier © Díaz-Perlas, Cristina; Oller-Salvia, Benjamí; Sánchez-Navarro, Macarena; Teixidó, Meritxell; & Giralt, Ernest is licensed under a CC BY-NC (Attribution NonCommercial) license
- U11-097 Blood Brain Barrier © Sykepleiepluss.com is licensed under a CC BY-SA (Attribution ShareAlike) license
- U11-098 Meninges and BBB © NIH Medical Arts is licensed under a CC BY-NC (Attribution NonCommercial) license
- U11-099 Dural Sinuses and Veins © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U11-100 Cavernous Sinus Fistula © Celik, Ozlem; Buyuktas, Deram; Islak, Civan1; Sarici, A Murat2; Gundogdu, A Sadi is licensed under a CC BY-SA (Attribution ShareAlike) license
- U11-101 Cavernous Sinus © Kuybu, Okkes MD and Diana is licensed under a CC BY-SA (Attribution ShareAlike) license
- U11-102 Venous Drainage to Cavernous Sinus © Wade, Alexia is licensed under a CC BY-SA (Attribution ShareAlike) license

