Large Intestine
Objective 6
Indicate the location of the following regions of the large intestine: cecum, appendix, ascending colon, transverse colon, descending colon, sigmoid colon, rectum, anus. Identify and describe the function of the ileocecal sphincter. Describe the histology and function of the internal and external sphincters of the anus. Explain how rectal distension triggers the defecation reflex. Describe the function of the sphincters. Explain the conscious control of defecation. Define and describe the Valsalva maneuver, including its effects on the GI and cardiovascular systems.
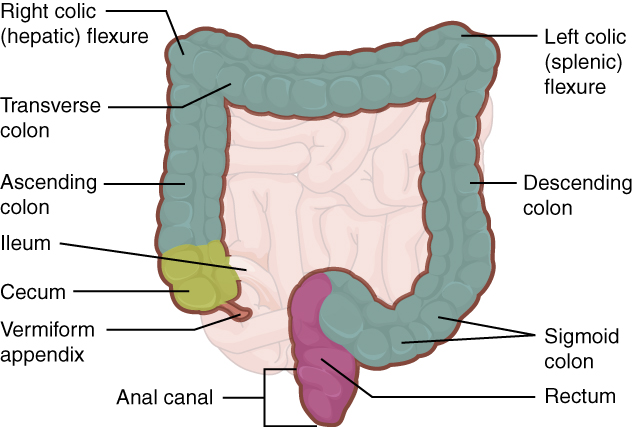
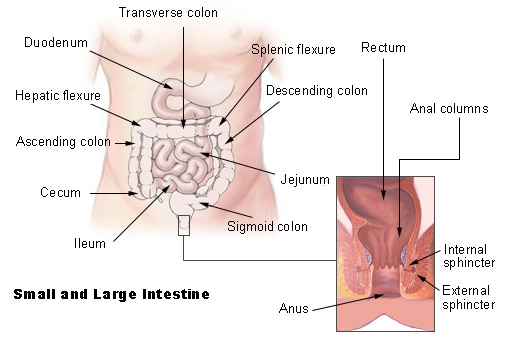
The large intestine is composed of four parts: cecum, colon, rectum, and anus/anal canal.
The large intestine begins where the ileum (the final portion of the small intestine) has an outlet through the ileocecal sphincter into the cecum (Latin cæcus, “blind pouch”). The cecum is a common site for GI problems. Not only does it tend to catch objects that have passed into the large intestine, but it ends in the vermiform appendix (or just appendix), a small wormlike tube that often becomes inflamed (appendicitis). It may even burst, dumping the bacteria-laden intestinal contents into the peritoneal cavity causing peritonitis, a medical emergency. It has recently been proposed that the appendix acts as a reservoir for “friendly” gut bacteria so that their colonies can be replaced after antibiotic treatment (Bollinger RR. J Theoret Biol 249: 826-831, 2007).
The large intestine (colon) continues upward as the ascending colon; crosses from right to left as the transverse colon; and drops down the left flank as the descending colon. At this point, it makes an S-shaped curve (sigmoid colon, from the Greek letter Σ or Roman S). Finally, it attaches to the anus through a straight segment, the rectum (Latin rectus, “straight”).
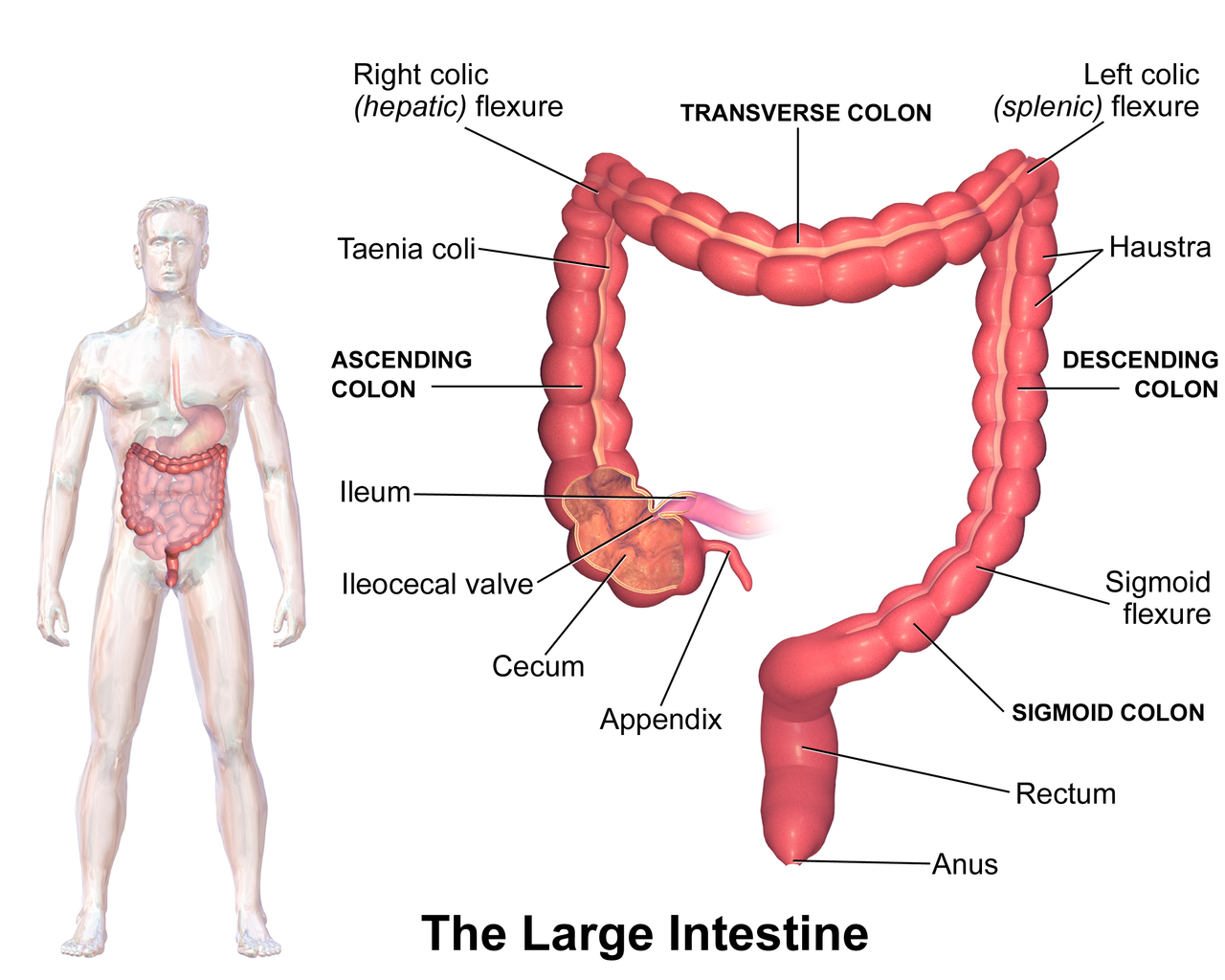
The taeniae coli are 3 longitudinal ribbons of smooth muscle that run along the ascending, transverse, descending, and sigmoid colon. The tonic contraction of these muscles form haustra which are small pouches that give the colon its segmented appearance.
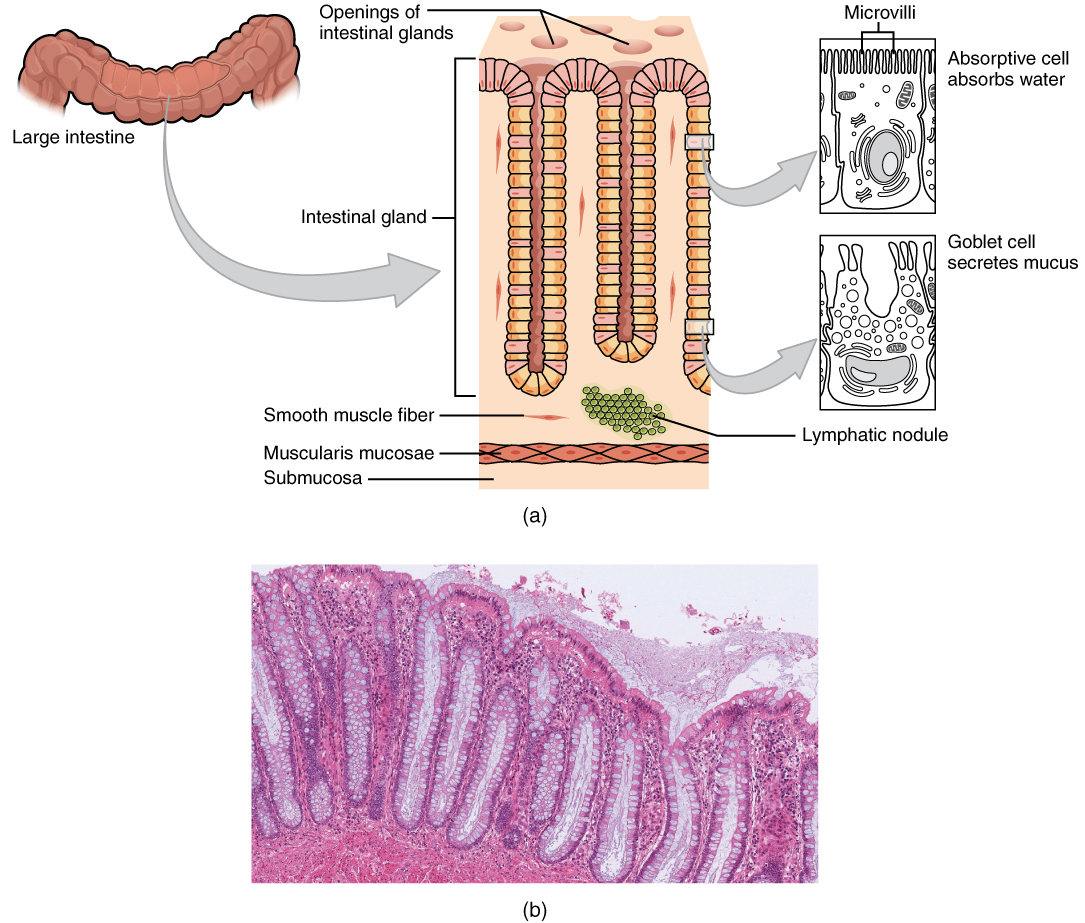
Like the small intestine, the histology of the large intestine follows the “standard” GI tract pattern very closely. In this case, the absorptive surface is limited to absorption of (mostly) water.
Also like the small intestine, the colon has a velvety appearance with numerous microvilli. There are openings for intestinal glands (crypts of Lieberkühn).
While the stomach and small intestine had a large number of cell types, in the colon, only two cell types are present: mucus-secreting goblet cells and water-absorbing absorptive cells. It is the absorptive cells that have microvilli on their surface.
Rather than secrete digestive enzymes, the large intestine mostly relies on bacteria to do its work. It is estimated that the human GI tract harbors 1014 living bacteria; of these, Escherichia coli (E. coli) is the best-known and best-studied. Bacteriodes fragilis, B. melaninogenicus, B. oralis, and Enterococcus fæcalis are also found in everyone’s colon. Feces are about 1/3 bacteria by weight with 3×1011 live bacteria in an average fecal bolus. These bacteria work to make some B vitamins as well as vitamin K, necessary for blood coagulation.
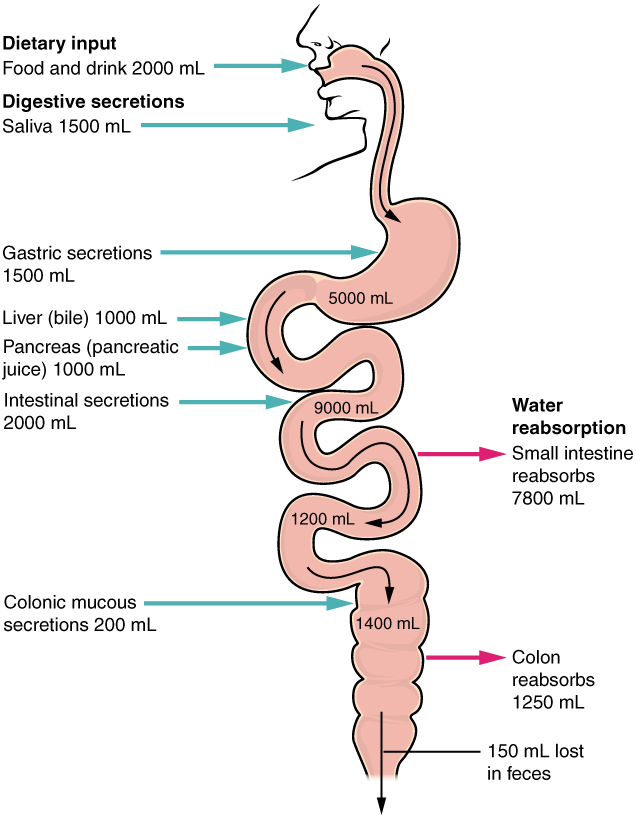
Both the small intestine and large intestine are responsible for water absorption. While water is needed for lubrication, and keeping the materials in the digestive tract in solution, it can safely be removed in the lower part of the small intestine and in the large intestine, when digestion is virtually complete.
The small intestine, by virtue of its greater length, absorbs most of the water that is ingested. Water is ingested both as liquid, and in food. The glands and organs of the GI tract (for example, the salivary glands, stomach, liver and pancreas) secrete fluid into the GI tract every day. Together, these make about 9.2 liters of water per day.
Of this 9.2 liters, the small intestine absorbs 7.8 liters. Thus, about 1.4 liter of water per day passes the ileocecal valve. The large intestine absorbs 1.25 liters, making the feces solid. The 150 ml that is not absorbed is used to keep feces moist so that they may be easily passed.
If the intestines fail to absorb water (as is the case in diseases of the GI tract), diarrhea results. More liquid than normal is excreted, along with relatively small amounts of feces.
If the intestines absorb too much water, then constipation results. The stools are hard and difficult to pass.
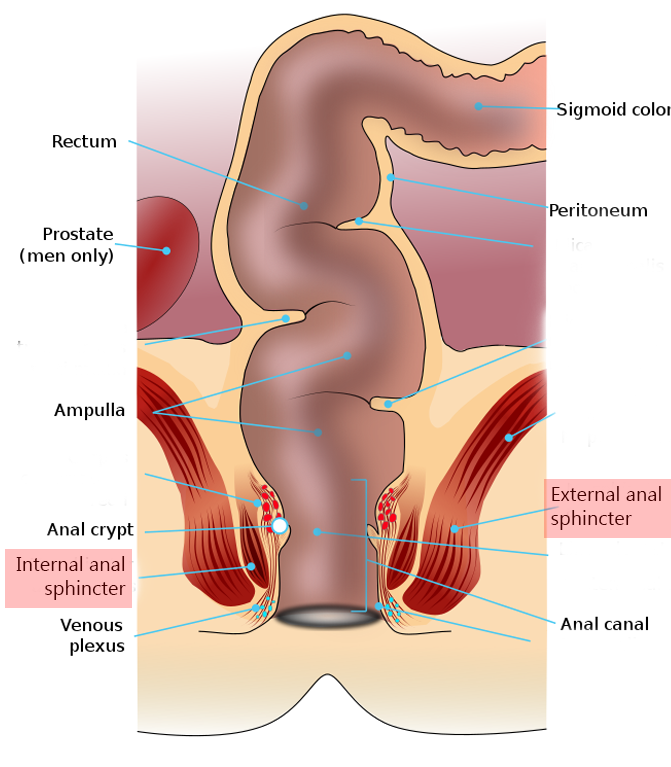
The rectum ends in the anal canal which in turn stops at the anus, the interface between the GI tract and the outside world. Two rings of muscle keep us from embarrassing ourselves publicly, but only one is under our control.
An inner ring of smooth muscle, the internal anal sphincter, is under autonomic control. An outer ring of striated muscle, the external anal sphincter, is responsible for voluntary control over the bowel.
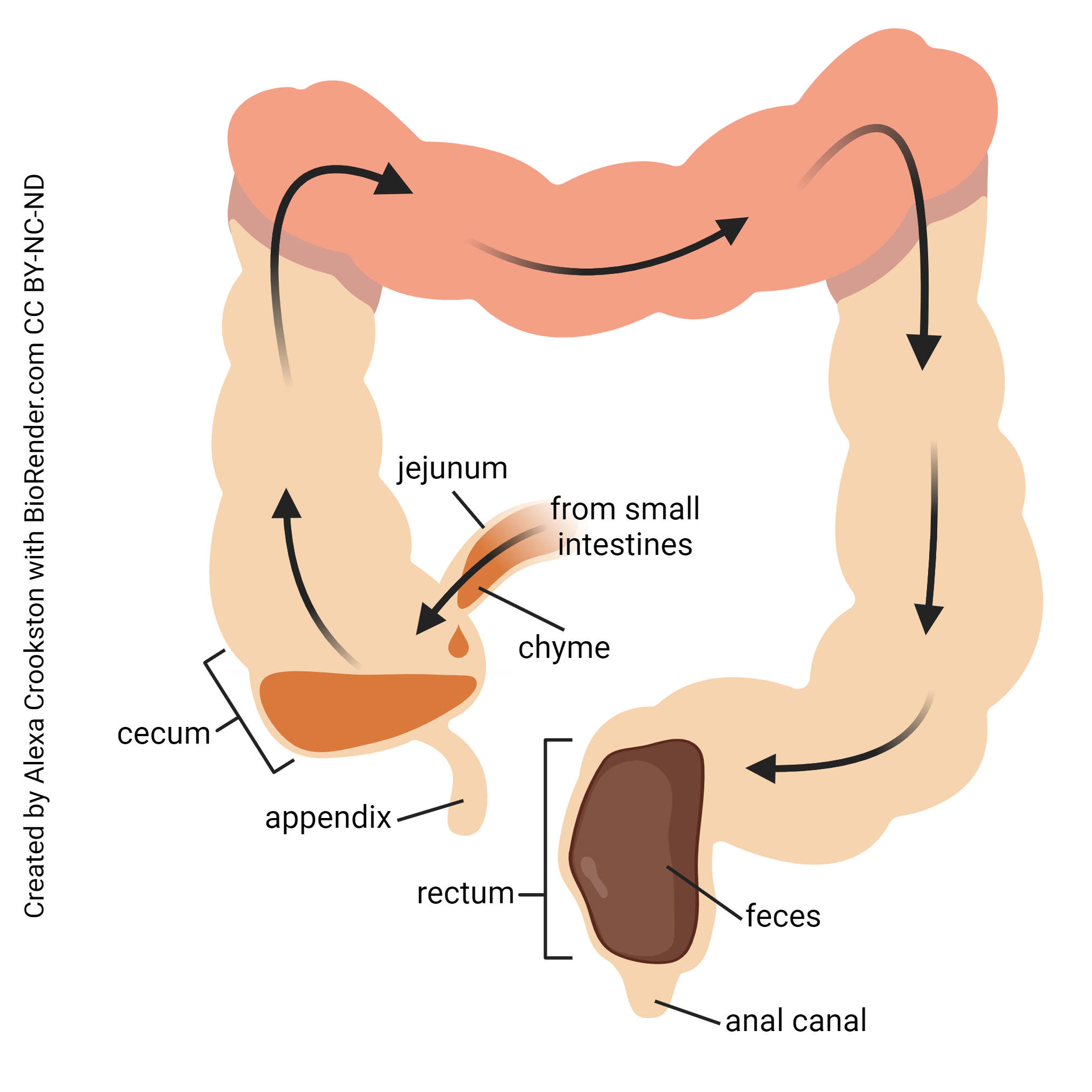
Like swallowing, the defecation reflex is a mixture of autonomic and voluntary motor control. Distension (enlargement) of the rectum activates stretch receptors in the wall of the rectum. The internal anal sphincter, under autonomic control, relaxes involuntarily.
Babies need diapers because they lack the ability to control the external anal sphincter. Fortunately for humankind, we all have parents who helped to wire our brains to our external anal sphincters and so we only relax this voluntary muscle when it’s socially appropriate to do so.
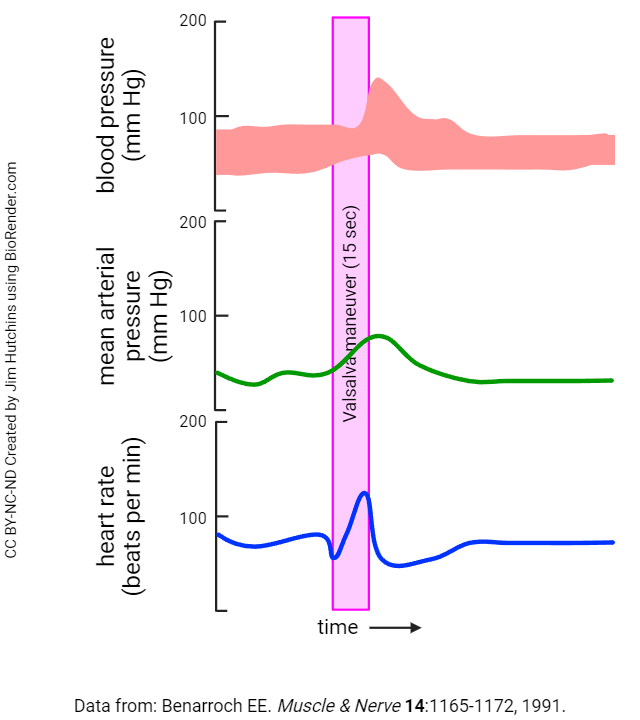
A group of techniques each called a Valsalva maneuver increase intra-abdominal pressure. One example includes “popping” the ears by closing the nose and mouth and blowing. Straining against a stool, or similar maneuvers which increase intrathoracic and intra-abdominal pressure, are also Valsalva maneuvers. “By increasing the intrathoracic and intra-abdominal pressure, the straining results in a decrease in the venous return of blood to the heart with an increase in venous pressure, progressive arterial pressure reduction, and, consequently, a progressive compensatory baroreflex-mediated heart rate increase.” (Junqueira LF. Adv Physiol Educ 32:100–106, 2008)
- Phase I: straining produces an ↑ systolic arterial pressure (transient)
- Phase II: continued straining ↓ arterial pressure, ↑ heart rate (this tachycardia is due to the increased sympathetic response of the carotid sinus reflex mentioned in cardiovascular)
- Phase III: as the strain is released, sudden ↓ arterial pressure, ↑ heart rate to maximum
- Phase IV: heart rate drops, and bradycardia (↓ heart rate) “overshoots” before a return to normal heart rate and blood pressure
Media Attributions
- U18-035 Large Intestine Anatomy © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U18-036 Large Intestine 2 © BruceBlaus is licensed under a CC BY (Attribution) license
- U18-037 Large Intestine Histology © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U18-038 Digestive Secretions Absorption of Water © Betts, J. Gordon; Young, Kelly A.; Wise, James A.; Johnson, Eddie; Poe, Brandon; Kruse, Dean H. Korol, Oksana; Johnson, Jody E.; Womble, Mark & DeSaix, Peter is licensed under a CC BY (Attribution) license
- U18-039 Anal Sphincters © National Cancer Institute is licensed under a Public Domain license
- U18-041 Rectum Anatomy © Kübelbeck, Armin is licensed under a CC BY-SA (Attribution ShareAlike) license
- U18-040 Large Intestines Defecation © Crookston, Alexa is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- U18-042 Valsalva Effects on BP HR © Hutchins, Jim is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license

