Infantile Spasms (West Syndrome)
Kobe Christensen and Jim Hutchins
WEST SYNDROME (INFANTILE SPASMS)
Introduction
West Syndrome is a severe epilepsy syndrome of infancy characterized by the triad of symptoms: Infantile spasms, Hypsarrhythmia EEG Pattern, Severe intellectual disability.
History
Infantile Spasms were first described by Dr. W. J West in the early 1840’s. He witnessed what he described as “Bobbing” events noting quick Tonic-Clonic movements of the head occurring in clusters over the span of three minutes.
It wasn’t until nearly 100 years later that the interictal EEG pattern termed Hypsarrhythmia would be connected with the clinical symptoms that Dr. West had described as “Infantile spasms.” The infantile spasms in conjunction with the Hypasarrhythmia EEG pattern would later be termed “West Syndrome.”
Symptoms
As mentioned previously, West Syndrome is classically characterized by the “Triad” of symptoms: Infantile spasms, Hypsarrhythmia EEG pattern, Severe intellectual disability.
Infantile Spasms
Infantile spasms are the characteristic clinical symptom observed during the Ictal period. Infantile spasms are typically broken down into two categories known as the flexor spasm and extensor spasm. The flexor spasm involves the contraction of the flexor muscles in the neck, trunk and limbs that has been described as a “Self-Hugging” motion. The extensor spasm is described as the lateral extension of the neck and truck away from the body. Infantile spasms are also known as Jackknife seizures.
Hypsarrhythmia
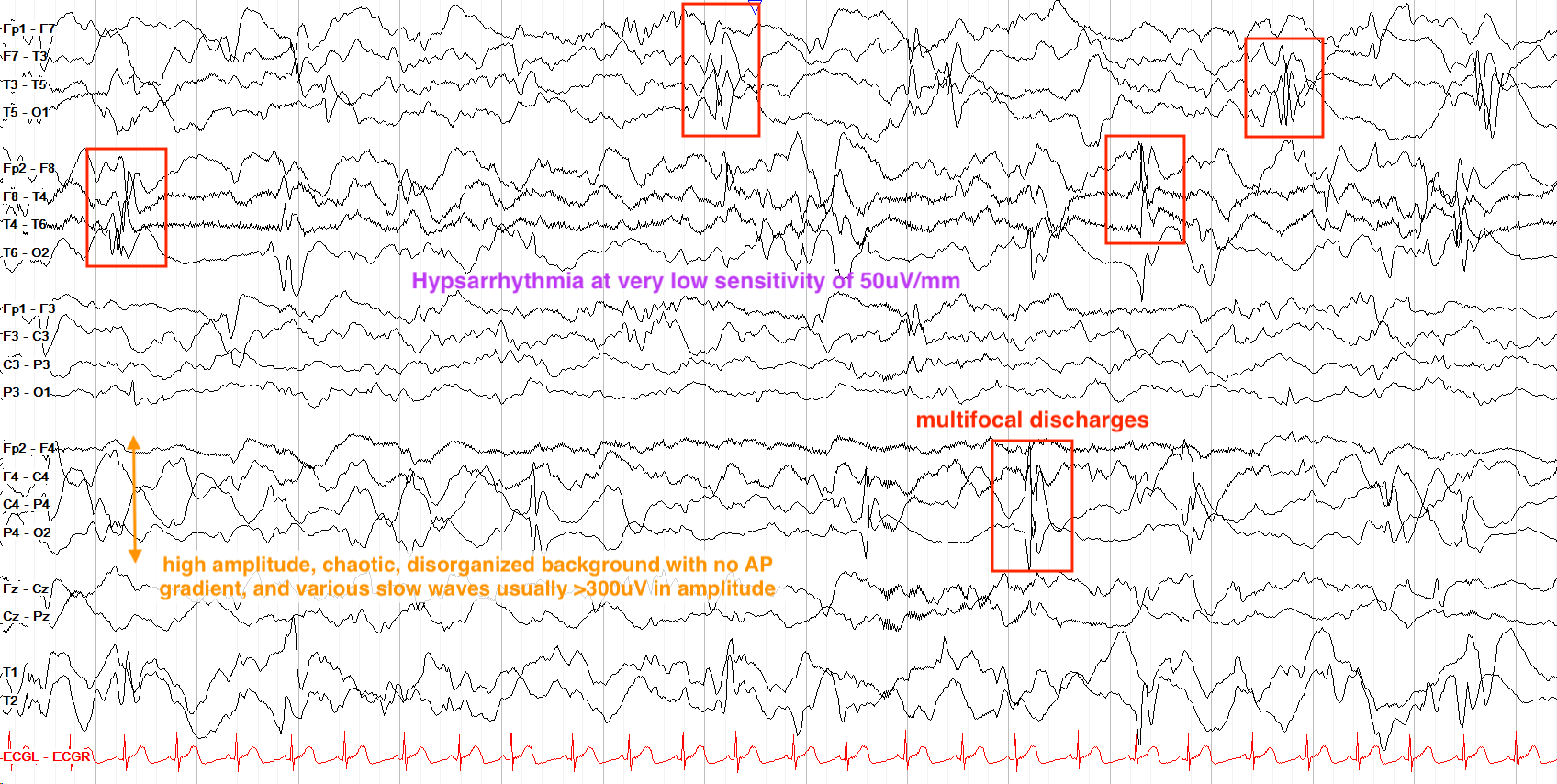
The Hypsarrhythmia pattern is observed during interictal-EEG.
The Hypsarrhythmia pattern is described as a
- High voltage (>300μV)
- Multi-focal
- Slow waves with superimposed spike & wave discharges

Ralphelg, CC BY-SA 3.0, via Wikimedia Commons
Figure 1.1 Awake interictal EEG showing disorganized high amplitude spike and wave compatible with Hypsarrhythmia.
From “The Pediatric EEG”, by David Valentine M.D., 2020, (https://www.learningeeg.com/pediatric). Copyright 2020 by David Valentine
Figure 1.2 Hypsarrhythmia pattern showing multifocal discharges.
Severe Intellectual Disability
In West Syndrome, studies have shown that ~70% of patients have significant intellectual delay. Evidence suggests that longer duration of spasms (Increased seizure frequency) is correlated with worse intellectual outcomes. Even in the case of spontaneous remission of West Syndrome, developmental prognosis is often unfavorable.
Classification of disease
West Syndrome tends to have two classifications of diagnoses pertaining to the origin of disease.
Idiopathic: Suspected to account for ~9-14% of diagnosed West Syndrome. This diagnosis is only given if there is normal development prior to onset of seizures, and there is no suspected underlying disorder.
Cryptogenic: Accounts for the majority of West Syndrome diagnoses. Typically in the case of West Syndrome, this diagnosis indicates that an underlying symptomatic cause is at play, but lacks official diagnosis.
Genetic Factors: Certain genes have been identified as being contributory to West Syndrome. These include the:
- TSC 1 & 2 genes (Known to cause Tuberous Sclerosis which is an autosomal dominants disease associated with another epilepsy syndrome, Sturge-Weber)
- ARX & CDKL5 genes (Both located on the X chromosome with evidence to suggest that a higher incidence of West Syndrome is associated with these genes)
Treatments & Prognosis
Prognosis of West Syndrome is poor and directly related to the severity of disease. Severe intellectual disability is present in nearly 70% of patients. Infantile spasms rarely last until adulthood as in ~50-70% of patients develop another seizure disorder. The evolution from West Syndrome to Lennox-Gastaut syndrome being the most common evolution.
Typical anti-epileptic drugs are often ineffective in patients with West Syndrome. The complete reduction of seizures in patients with West Syndrome is rare and treatment usually aims to decrease seizure frequency but rarely aims to keep patients seizure free.
Typical medications used in the treatment of West Syndrome include ACTH, Vigabatrin, and Corticosteroids. Often times multiple medications will be used together to decrease seizure frequency.
Another common treatment in West Syndrome is the Ketogenic diet. Studies have shown that in conjunction with ACTH, the Ketogenic diet reduced seizure frequency in nearly 65% of patients.
Key Takeaways
- West Syndrome is characterized by a characteristic Hypsarrhytmia EEG pattern, Infantile spasms, and severe intellectual disability.
- The Hypsarrhytmia pattern is a high voltage, slow wave pattern with multifocal spike activity.
- The progression of West Syndrome to Lennox-Gastaut is very common.
- The Ketogenic Diet along with ACTH are the mainline treatments for West Syndrome.
MYOCLONIC-ASTATIC EPILEPSY (DOOSE SYNDROME)
Introduction
Myoclonic-Astatic Epilepsy (MAE), also known as Doose Syndrome is a pediatric seizure disorder commonly affecting children between the ages of 2-5 years that is characterized by frequent myoclonic and atonic seizures. MAE often presents with developmental delay, cognitive impairment, and behavioral challenges.
MAE affects males more often than females at a ratio of 2:1 after the first year of life. During the first year of life literature suggests that MAE will affect the sexes at roughly the same rate.
Signs & Symptoms
Epilepsy
MAE's hallmark symptoms are frequent myoclonic and atonic seizures, however it is not uncommon for other seizure types to be witnessed in patients with MAE. Other seizures may include generalized tonic-clonic, absence, tonic, and progression to non-convulsive status epilepticus (NCSE). Patients can have hundreds of seizures in a single day, and most frequently have seizures in the morning shortly after waking. Sometimes these seizures are isolated, but they often tend to cluster thus increasing their risk to slip into status-epilepticus.
EEG in MAE typically reveals bursts of 2-5 Hz polyspike and wave complexes that are generally superimposed onto otherwise normal looking backgrounds. An important feature in differentiating MAE from other pediatric seizure disorders like LGS is the presence of a relatively normal PDR and sleep architecture.
Cognitive Impairment
Cognitive outcomes in MAE are highly variable. Some experience normal cognition while others may have severe intellectual disability. The literature suggests that seizure frequency is correlated to the cognitive outcome as those who attain freedom from seizures tend to have more favorable cognitive outcomes. Changes in behavior are another commonly associated symptom with MAE. Up to 1/5th of documented MAE cases are diagnosed with ADHD.
Treatment & Prognosis
Treatment efficacy of MAE varies as some enter complete remission of seizures, and others have intractable epilepsy. MAE is largely considered a generalized seizure disorder and is treated as such with ethosuximide which is a common AED for controlling generalized seizures. The standard of care is to pair the AED's with dietary therapy which most often consists of the ketogenic diet.
Prognosis in MAE varies depending on the age of onset, frequency of seizures, and seizure control. The literature suggests that roughly 3 in 5 children will have a complete remission from seizures and no longer require treatment. In other children, seizure control may range from well controlled to intractable. In children who do not have seizure freedom, cognitive impairment tends to increase in severity.
Key Takeaways
- Myoclonic-Astatic Epilepsy (MAE) is characterized by frequent myoclonic and atonic seizures.
- Bursts of 2-5 Hz polyspike and wave discharges superimposed onto otherwise normal backgrounds are a common characteristic of MAE.
- Prognosis is often dependent on factors such as seizure frequency, age of onset, and seizure type.
- Dietary therapy is effective in the treatment of MAE.
Chapter under construction. If you have questions, or want to help in the writing or editing process, please contact hutchins.jim@gmail.com.
ELECTRICAL STATUS EPILEPTICUS OF SLEEP (ESES)
Introduction
Electrical Status Epilepticus in Sleep (ESES) is a condition that is characterized by an EEG pattern of continuous spike and wave discharges during non-REM (NREM) sleep. ESES presents with cognitive decline, likely as a result of almost constant epileptiform activity during sleep which may lead to significant cognitive decline.
Signs & Symptoms
Onset
ESES typically affects children between the ages of 2 and 12 with a peak onset between 4 and 8 years old.
Cognitive Effects
A hallmark of ESES is regression in their development. Normal sleep processes are critical for consolidating memories, processing information, and the ability to learn new skills. Due to the frequent disturbance of sleep, many children with ESES experience a loss of previously acquired skills particularly in language and memory. Some children will experience significant behavior and emotional challenges that may be misinterpreted as ADHD or other behavioral disorders.
Epilepsy
ESES is defined by frequent epileptiform rather than physical seizures though some children may experience absence, atonic, myoclonic, or focal seizure types. Seizure frequency is noted to be heavily correlated with cognitive regression in these patients.
EEG Findings
Characteristic Discharges
The key EEG pattern in the diagnosis of ESES are continuous (or nearly continuous) spike and wave discharges during NREM sleep. These discharges are isolated to NREM sleep, as during wakefulness and REM sleep the pattern may partially or completely disappear.
During NREM sleep, discharges are generally between 1-3 Hz spike and wave discharges that are often generalized, but may appear more focal in some cases. During wakefulness and REM sleep, it is more likely to see discontinuous, focal or multifocal epileptiform discharges. Due to the sleep dependence of ESES, clinical guidelines generally recommend a prolonged EEG capturing multiple sleep cycles to aid in diagnosis.
Spike-Wave Index (SWI)
The SWI is used to measure the percentage of NREM sleep that is marked by epileptiform discharges. For diagnosis of ESES, the SWI is typically >85%, though there is some debate among researchers as different studies have quoted a highly variable range between 25%-85% of NREM sleep being considered ESES.
(Insert photo of ESES when given permission)
Treatments & Prognosis
Antiepileptic Drugs (AEDs)
Commonly used AEDs in the treatment of of ESES include, levetiracetam, valproate and ethosuximide. These medications are not generally given as a monotherapy, but rather together in some type of combination therapy. AEDs generally prove useful as they can decrease the frequency of discharges during sleep, however complete remission is not commonly reached.
Prognosis
In children with ESES, seizures and epileptiform during sleep tend to spontaneously resolve after puberty. However, cognitive decline as a result of ESES typically persists into adulthood. Capturing ESES earlier in life is important to reducing the severity of cognitive decline into adulthood as delayed treatment generally leads to a worse cognitive outcome.
Associated With Landau-Kleffner Syndrome
Landau-Kleffner syndrome is marked by a severe regression of language development and status epilepticus during sleep. EEG in Landau-Kleffner is usually lateralized as opposed to the diffuse nature of ESES. Children with Landau-Kleffner are still referred to as having ESES, and it is important to know that while all Landau-Kleffner patients have a form of ESES, not all ESES patients are diagnosed with Landau-Kleffner syndrome.
Case Study
Scenario
A 5 year old child with no prior medical history is referred to a neurologist due to significant language regression and attention difficulties in school.
EEG Findings
Wakeful EEG showed multifocal sharps suggesting potential epilepsy. Upon falling asleep, the monitoring technician noticed nearly continuous spike and wave discharges with a frequency of 2-2.5 Hz. These discharges abruptly stopped when the patient entered REM sleep, and shortly restarted as the sleep cycle continued. The technician noted that about 90% of the NREM sleep cycle was marked by these continuous epileptiform discharges.
Diagnosis
Electrical Status Epilepticus in Sleep (ESES).
Key Takeaways
- ESES affects children between the ages of 2 and 12, and will spontaneously resolve after puberty.
- EEG during NREM sleep will show nearly continuous 1-3 Hz spike and wave discharges that make up >85% of the non-REM sleep cycle.
- Language regression, cognitive decline, and behavioral challenges are symptoms of ESES.
- ESES is seen in Landau-Kleffner syndrome, though typically in Landau-Kleffner syndrome ESES is only seen unilaterally on EEG.
https://www.youtube.com/watch?v=b_MWLv31c34
H5P
RETT SYNDROME
Introduction
Rett Syndrome is a rare pediatric neurodevelopmental disorder that primarily affects females and is characterized by severe cognitive and physical impairment. Rett Syndrome is primarily caused by the MECP2 gene, which plays a crucial role in regulating gene expression during brain development.
Symptoms
Cognitive Impairment
The hallmark symptom of Rett Syndrome is a loss of purposeful gross motor skills. Rett Syndrome has a slow onset of symptoms, and is typically diagnosed between 1-2 years of age. Most commonly, parents will notice a regression of acquired skills like language and social engagement followed by a regression in large motor skills (I.E. Patient goes from walking to primarily crawling). Along with a loss of purposeful motor movement, repetitive and uncontrolled hand movements such as hand-wringing or hand-washing motions become ever apparent in patients with Rett Syndrome. Epilepsy, scoliosis, and gait abnormalities are also common symptoms seen in Rett Syndrome.
Epilepsy
In the literature, there are not many findings of characteristic EEG patterns in patients with Rett Syndrome. Early in Rett Syndrome, EEG's typically tend to be normal. As Rett Syndrome begins to progress centrotemporal spikes may be seen with a clinical correlation of motor impairment. As Rett Syndrome further progresses abnormalities during sleep may be seen followed by diffuse background slowing and multifocal spike and wave activity.
Figure 5.1 Rett Syndrome patient with Scoliosis
Konstantinos C Soultanis, corresponding author1 Alexandros H Payatakes,2,3 Vasilios T Chouliaras,2 Georgios C Mandellos,2 Nikolaos E Pyrovolou, Fani M Pliarchopoulou,4 and Panayotis N Soucacos1, CC BY 2.5 via Wikimedia Commons
Treatment & Prognosis
Prognosis
While most individuals with Rett Syndrome live well into adulthood, cognitive prognosis remains quite poor. Almost all patients with Rett Syndrome require 24 hour support as they maintain a cognitive level to that of a 1 year old.
Treatment
There are no direct pharmacological treatments for Rett Syndrome. However, anti-epileptic drugs are frequently used to decrease seizure frequency. Various types of therapy can help to improve the quality of life for those with Rett Syndrome, but at this time there is no treatment for the cognitive impairment experienced by these patients.
Key Takeaways
- Rett Syndrome is a neurodevelopmental disorder that primarily affects females.
- Caused by a mutation in the MECP2 gene, children with Rett Syndrome tend to develop normally until 6-18 months of age.
- The hallmark symptom for Rett Syndrome is the regression of gross motor function.
- There are no known treatments or cures for Rett Syndrome.


